Significance of immuno-inflammatory indexes and lymphocyte subsets in the prognosis of newly diagnosed multiple myeloma
-
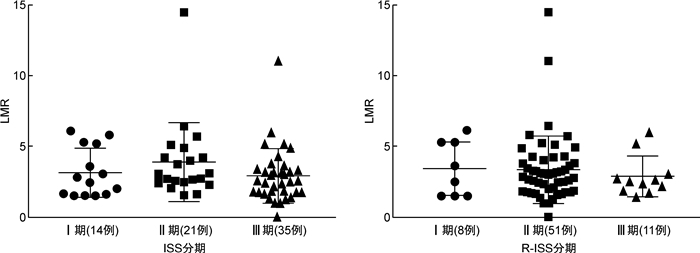
摘要: 目的 探讨免疫炎性指标和淋巴细胞亚群在初诊多发性骨髓瘤(NDMM)患者预后判断中的作用。方法 回顾性分析2018年6月—2019年12月我院血液科收治的NDMM患者的临床资料,包括免疫炎性指标中性粒细胞/淋巴细胞比值(NLR)、淋巴细胞/单核细胞比值(LMR)、血小板/淋巴细胞比值(PLR)以及不同淋巴细胞亚群水平,对其临床特征、治疗反应和预后情况进行分析。结果 ① 共纳入70例NDMM患者,中位发病年龄64(37~78)岁,男女比例1.9∶1.0;不同ISS及R-ISS分期的患者LMR水平比较差异有统计学意义(P=0.018、0.004),而NLR、PLR及外周血淋巴细胞亚群水平比较差异无统计学意义。②分别以各免疫炎性指标的中位数作为cut-off值将患者分为高低2组,结果显示高NLR组总缓解率明显低于低NLR组(54.3% vs 82.9%,P=0.010),而高LMR组、高CD3+T细胞表达组及高NK细胞表达组总缓解率分别为91.4%、80.6%及82.9%,明显高于低水平组的45.9%、55.9%及54.3%(P<0.001、P=0.026和P=0.010)。③70例患者的疗效均可评估,总缓解率为68.6%(48/70),19例疾病进展患者中8例使用以达雷妥尤单抗为基础的联合化疗,结果显示达雷妥尤单抗治疗前后外周血淋巴细胞亚群变化差异无统计学意义。④单因素分析显示,ISS分期、R-ISS分期、β2-微球蛋白、LMR、PLR、CD3+CD8+百分比、CD4/CD8比值是患者总生存的影响因素(P<0.05);多因素分析显示,R-ISS分期(HR=8.001,95%CI2.222~28.812,P=0.001)、CD4/CD8比值(HR=3.875,95%CI1.005~14.946,P=0.049)是影响患者总生存的独立危险因素。⑤根据患者伴有不良预后因素的免疫指标(LMR、PLR、CD3+CD8+百分比、CD4/CD8比值)个数,将患者分为伴有0或1个、2个和≥3个预后不良因素组,3组间总生存时间比较差异有统计学意义(P=0.000 3)。结论 免疫炎性指标和外周血淋巴细胞亚群可反映机体免疫状态,在一定程度上对NDMM患者的预后判断有价值,值得临床深入研究。Abstract: Objective To explore the role of immuno-inflammatory indexes and lymphocyte subsets in the prognosis of newly diagnosed multiple myeloma(NDMM) patients.Methods The clinical characteristics, including immuno-inflammatory indexes neutrophil/lymphocyte ratio(NLR), lymphocyte/monocyte ratio(LMR), platelet/lymphocyte ratio(PLR) and different lymphocyte subsets, treatment response and prognosis of NDMM patients admitted to our hospital from June 2018 to December 2019 were retrospectively analyzed.Results ① The median age of 70 NDMM patients was 64(37-78) years, and the male to female ratio was 1.9∶1.0. The LMR levels of patients with different ISS and R-ISS stages were significantly different(P=0.018, 0.004, respectively), while there were no significant differences in NLR, PLR and lymphocyte subsets. ②Patients were divided into high and low groups with the median of each immuno-inflammatory index as a cut-off value, respectively. The overall remission rate(ORR) in the high NLR group was significantly lower than that in the low NLR group(54.3% vs 82.9%,P=0.010). The ORR in the high LMR group, high CD3+T cell expression group and high NK cell expression group were 91.4%, 80.6%, and 82.9%, significantly higher than 45.9%, 55.9%, and 54.3% in the low group(P< 0.001,P=0.026,P=0.010). ③The curative effect of 70 patients was evaluable, and the ORR was 68.6%(48/70). Eight cases of the 19 patients with disease progression were treated with combination chemotherapy based on daratumumab, and there was no significant difference in the changes of lymphocyte subsets before and after treatment with daratumumab. ④The univariate analysis revealed that ISS stage, R-ISS stage, β2-microglobulin, LMR, PLR, CD3+CD8+percentage, and CD4/CD8 ratio were the risk factors for the overall survival of patients with NDMM(P< 0.05). The multivariate analysis revealed that R-ISS stage(HR=8.001, 95%CI2.222-28.812,P=0.001), CD4/CD8 ratio(HR=3.875, 95%CI1.005-14.946,P=0.049) were the independent risk factors for the overall survival of patients with NDMM. ⑤Patients were divided into groups with 0 or 1, 2 and ≥3 adverse prognostic factors according to the number of immune indexes(LMR, PLR, CD3+CD8+percentage, CD4/CD8 ratio) with adverse prognostic factors, the result revealed that the more prognostic factors were associated with shorter median overall survival time(P=0.000 3).Conclusion Immuno-inflammatory indexes and lymphocyte subsets can reflect the immune status of the body, which is valuable for judging the prognosis of NDMM patients to a certain extent and worthy of further clinical study.
-
Key words:
- immuno-inflammatory indexes /
- lymphocyte subsets /
- immune function /
- multiple myeloma /
- prognosis
-

-
表 1 初诊MM患者不同水平免疫生物标志物疗效比较
因素 例数 ORR(48例) sCR/CR(17例) 因素 例数 ORR(48例) sCR/CR(17例) 例(%) P 例(%) P 例(%) P 例(%) P NLR 0.010 0.403 CD3+CD8+ 0.091 0.409 <2.34 35 29(82.9) 10(28.6) <26.0% 31 18(58.1) 9(29.0) ≥2.34 35 19(54.3) 7(20.0) ≥26.0% 39 30(76.9) 8(20.5) LMR <0.001 0.050 CD4/CD8 <0.001 0.073 <2.73 35 16(45.9) 5(14.3) 正常 55 46(83.6) 16(29.1) ≥2.73 35 32(91.4) 12(34.3) ≤1 15 2(13.3) 1(6.7) PLR 0.122 0.403 CD3-CD19+ 1.000 0.780 <116.50 35 21(60.0) 10(28.6) <5.4% 35 24(68.6) 9(25.7) ≥116.50 35 27(77.1) 7(20.0) ≥5.4% 35 24(68.6) 8(22.9) CD3+ 0.026 0.679 NK 0.010 0.403 <74.0% 34 19(55.9) 9(26.5) <14.3% 35 19(54.3) 7(20.0) ≥74.0% 36 29(80.6) 8(22.2) ≥14.3% 35 29(82.9) 10(28.6) CD3+CD4+ 0.607 0.403 <42.5% 35 23(65.7) 7(20.0) ≥42.5% 35 25(71.4) 10(28.6) 表 2 8例使用达雷妥尤单抗治疗前后外周血淋巴细胞亚群水平比较
M(范围) 组别 CD3+/% CD3+CD4+/% CD3+CD8+/% CD4/CD8 CD3-CD19+/% NK/% 治疗前 75(50~90) 44.0(31~55) 24(17~100) 0.66(0.16~1.43) 3.45(1.90~11.90) 19.35(6.10~32.80) 治疗后 76(45~96) 28.5(20~66) 33(24~48) 0.60(0.27~2.54) 1.75(0.40~3.80) 18.65(1.20~29.40) Z -0.421 -0.981 -1.120 -0.560 -1.859 -0.700 P 0.674 0.326 0.263 0.575 0.063 0.484 表 3 影响初诊MM患者OS的单因素及多因素分析
因素 单因素分析 多因素分析 HR(95%CI) P HR(95%CI) P 年龄(<65岁vs ≥65岁) 2.642(0.571~12.730) 0.214 ISS分期(Ⅰ/Ⅱ期vs Ⅲ期) 5.993(1.282~28.005) 0.023 R-ISS分期(Ⅰ/Ⅱ期vs Ⅲ期) 13.240(3.930~44.605) <0.001 8.001(2.222~28.812) 0.001 Hb(<115 g/L vs ≥115 g/L) 0.413(0.053~3.229) 0.400 Cr(<177 μmol/L vs ≥177 μmol/L) 3.104(0.894~10.775) 0.074 ALB(<35 g/L vs ≥35 g/L) 0.807(0.238~2.734) 0.731 Ca2+(<2.55 mmol/L vs ≥2.55 mmol/L) 0.773(0.099~6.053) 0.807 LDH(<245 U/L vs ≥245 U/L) 2.704(0.535~8.031) 0.291 β2-MG(<5.5 mg/L vs ≥5.5 mg/L) 4.819(1.260~18.430) 0.022 NLR(<2.34 vs ≥2.34) 2.174(0.630~7.505) 0.219 LMR(<2.73 vs ≥2.73) 0.211(0.046~0.977) 0.047 PLR(<116.50 vs ≥116.50) 0.171(0.036~0.801) 0.025 CD3+(<74.0% vs ≥74.0%) 0.530(0.155~1.819) 0.313 CD3+CD4+(<42.5% vs ≥42.5%) 2.515(0.713~8.876) 0.152 CD3+CD8+(<26.0% vs ≥26.0%) 0.239(0.062~0.920) 0.037 CD4/CD8(≤1 vs正常) 7.809(2.283~26.710) <0.001 3.875(1.005~14.946) 0.049 CD3-CD19+(<5.4% vs ≥5.4%) 0.941(0.286~3.101) 0.920 NK(<14.3% vs ≥14.3%) 1.594(0.465~5.460) 0.458 -
[1] Rajkumar SV. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management[J]. Am J Hematol, 2020, 95(5): 548-567. doi: 10.1002/ajh.25791
[2] Lemaire M, Deleu S, De Bruyne E, et al. The microenvironment and molecular biology of the multiple myeloma tumor[J]. Adv Cancer Res, 2011, 110: 19-42.
[3] De Raeve HR, Vanderkerken K. The role of the bone marrow microenvironment in multiple myeloma[J]. Histol Histopathol, 2005, 20(4): 1227-1250.
[4] Adams-Huet B, Jialal I. The neutrophil count is superior to the neutrophil/lymphocyte ratio as a biomarker of inflammation in nascent metabolic syndrome[J]. Ann Clin Biochem, 2019, 56(6): 715-716. doi: 10.1177/0004563219866221
[5] 张林, 陈玥, 张宝红. 血小板-淋巴细胞比率、中性粒细胞-淋巴细胞比率及红细胞分布宽度在冠心病严重程度中的诊断价值[J]. 临床心血管病杂志, 2020, 36(9): 824-827. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202009010.htm
[6] 乾叶子, 杨威, 吕媛媛, 等. N端脑钠肽前体、可溶性人基质裂解素2及血小板/淋巴细胞比值对慢性心力衰竭的诊断价值[J]. 临床心血管病杂志, 2021, 37(3): 239-243. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202103011.htm
[7] Krenn-Pilko S, Langsenlehner U, Thurner EM, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients[J]. Br J Cancer, 2014, 110(10): 2524-2530. doi: 10.1038/bjc.2014.163
[8] Diem S, Schmid S, Krapf M, et al. Neutrophil-to-Lymphocyte ratio(NLR)and Platelet-to-Lymphocyte ratio(PLR)as prognostic markers in patients with non-small cell lung cancer(NSCLC)treated with nivolumab[J]. Lung Cancer, 2017, 111: 176-181. doi: 10.1016/j.lungcan.2017.07.024
[9] Lee SF, Ng TY, Spika D. Prognostic value of lymphocyte-monocyte ratio at diagnosis in Hodgkin lymphoma: a meta-analysis[J]. BMC Cancer, 2019, 19(1): 338. doi: 10.1186/s12885-019-5552-1
[10] Stefaniuk P, Szymczyk A, Podhorecka M. The Neutrophil to Lymphocyte and Lymphocyte to Monocyte Ratios as New Prognostic Factors in Hematological Malignancies-A Narrative Review[J]. Cancer Manag Res, 2020, 12: 2961-2977. doi: 10.2147/CMAR.S245928
[11] Belotti A, Doni E, Bolis S, et al. Peripheral blood lymphocyte/monocyte ratio predicts outcome in follicular lymphoma and in diffuse large B-cell lymphoma patients in the rituximab era[J]. Clin Lymphoma Myeloma Leuk, 2015, 15(4): 208-213. doi: 10.1016/j.clml.2014.10.001
[12] 中国医师协会血液科医师分会, 中华医学会血液学分会, 中国医师协会多发性骨髓瘤专业委员会. 中国多发性骨髓瘤诊治指南(2020年修订)[J]. 中华内科杂志, 2020, 59(5): 341-346. doi: 10.3760/cma.j.cn112138-20200304-00179
[13] Pessoa DMR, Vidriales MB, Paiva B, et al. Analysis of the immune system of multiple myeloma patients achieving long-term disease control by multidimensional flow cytometry[J]. Haematologica, 2013, 98(1): 79-86. doi: 10.3324/haematol.2012.067272
[14] 朱成斌, 蔡春莲. 血常规指标对初诊多发性骨髓瘤临床分期和预后预测价值的研究[J]. 临床血液学杂志, 2021, 34(10): 723-727. http://lcxz.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=017072ce-7cb9-428d-ae01-fb6bc3b30c5e
[15] Romano A, Laura PN, Cerchione C, et al. The NLR and LMR ratio in newly diagnosed MM patients treated upfront with novel agents[J]. Blood Cancer J, 2017, 7(12): 649. doi: 10.1038/s41408-017-0019-6
[16] Kelkitli E, Atay H, Cilingir F, et al. Predicting survival for multiple myeloma patients using baseline neutrophil/lymphocyte ratio[J]. Ann Hematol, 2014, 93(5): 841-846. doi: 10.1007/s00277-013-1978-8
[17] Shi L, Qin X, Wang H, et al. Elevated neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio and decreased platelet-to-lymphocyte ratio are associated with poor prognosis in multiple myeloma[J]. Oncotarget, 2017, 8(12): 18792-18801. doi: 10.18632/oncotarget.13320
[18] Joshua D, Suen H, Brown R, et al. The T Cell in Myeloma[J]. Clin Lymphoma Myeloma Leuk, 2016, 16(10): 537-542. doi: 10.1016/j.clml.2016.08.003
[19] Huang LQ, Wang JX, He K, et al. Analysis of peripheral blood T-cell subsets and regulatory T-cells in multiple myeloma patients[J]. Cell Mol Biol(Noisy-le-grand), 2018, 64(5): 113-117. doi: 10.14715/cmb/2018.64.5.19
[20] Pittari G, Vago L, Festuccia M, et al. Restoring Natural Killer Cell Immunity against Multiple Myeloma in the Era of New Drugs[J]. Front Immunol, 2017, 8: 1444. doi: 10.3389/fimmu.2017.01444
[21] Kawano Y, Roccaro AM, Ghobrial IM, et al. Multiple Myeloma and the Immune Microenvironment[J]. Curr Cancer Drug Targets, 2017, 17(9): 806-818.
[22] 许婷, 唐亚男, 何月茹, 等. NK细胞及调节性T细胞在多发性骨髓瘤中的表达水平及其意义[J]. 临床血液学杂志, 2020, 33(3): 187-190. http://lcxz.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=bcdb4b01-8a28-4b88-a77c-7866afd5710a
[23] Koike M, Sekigawa I, Okada M, et al. Relationship between CD4(+)/CD8(+)T cell ratio and T cell activation in multiple myeloma: reference to IL-16[J]. Leuk Res, 2002, 26(8): 705-711. doi: 10.1016/S0145-2126(01)00192-8
[24] 朱明霞, 万文丽, 王晶, 等. 45例多发性骨髓瘤患者细胞免疫功能变化及其临床意义[J]. 中华血液学杂志, 2014, 35(12): 1053-1057. doi: 10.3760/cma.j.issn.0253-2727.2014.12.002
[25] Pick M, Vainstein V, Goldschmidt N, et al. Daratumumab resistance is frequent in advanced-stage multiple myeloma patients irrespective of CD38 expression and is related to dismal prognosis[J]. Eur J Haematol, 2018, 100(5): 494-501. doi: 10.1111/ejh.13046
-




 下载:
下载:
