Effect of EBV infection in central nervous system on prognosis of patients with EBV-associated hemophagocytic lymphohistiocytosis
-
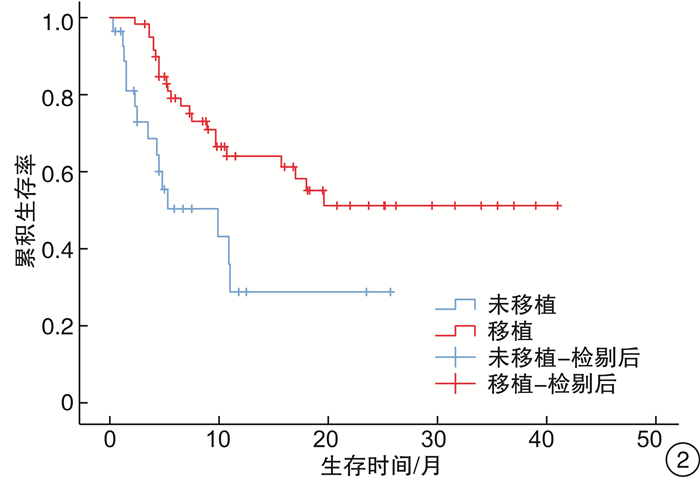
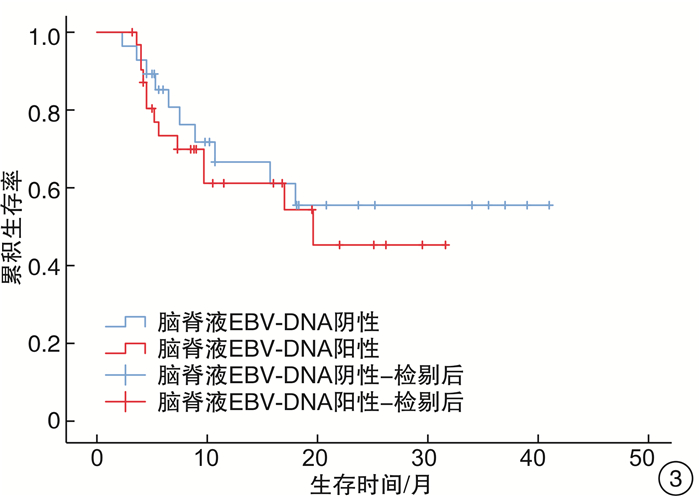
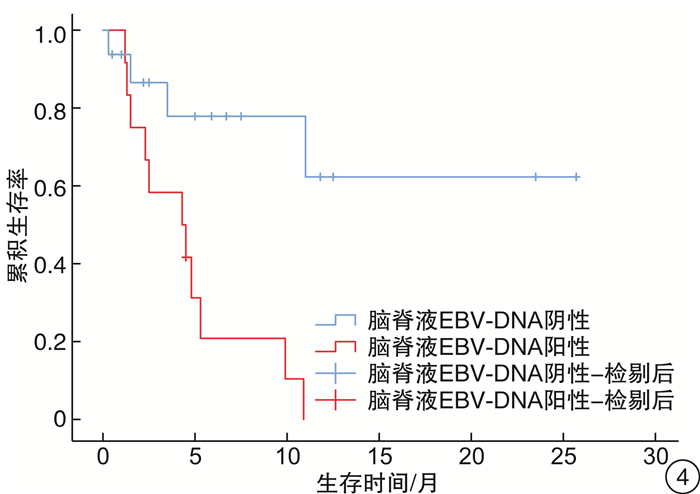
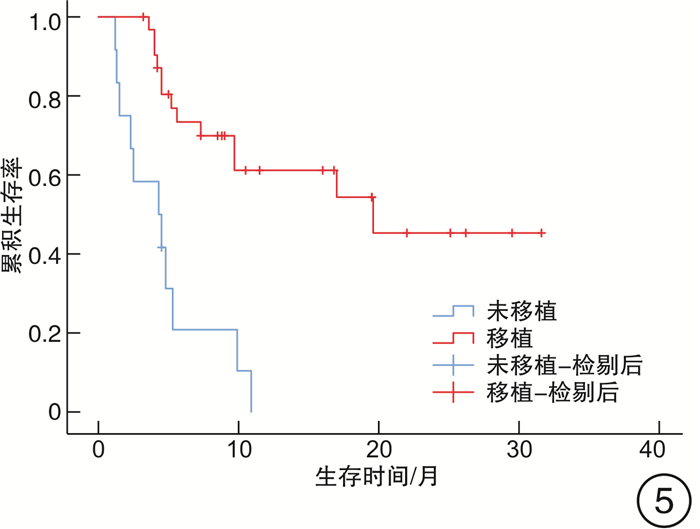
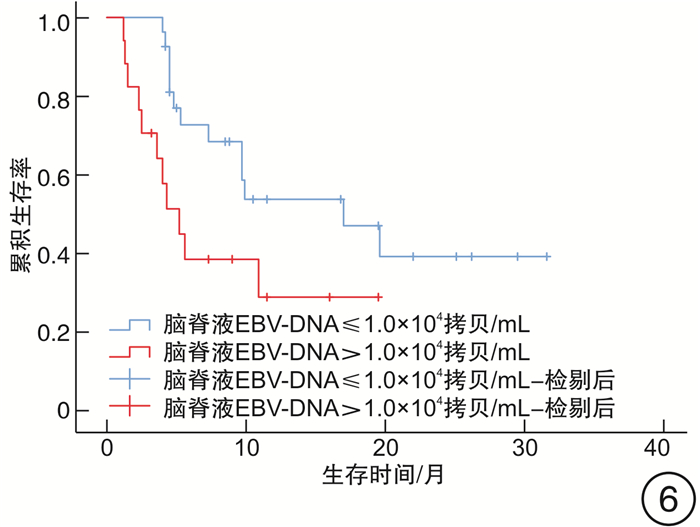
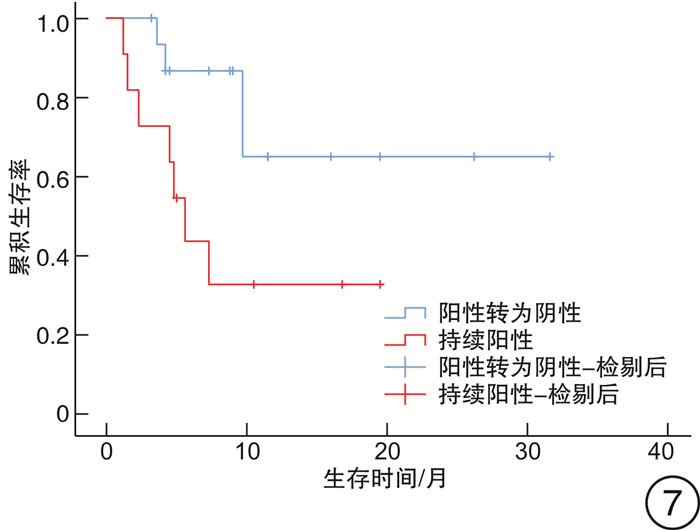
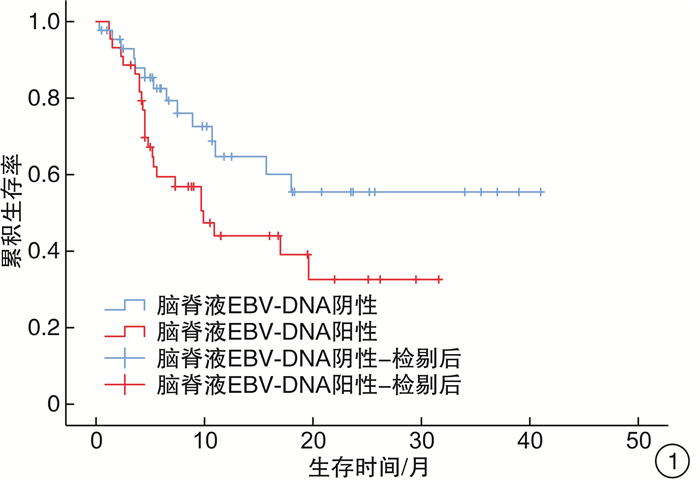
摘要: 目的 探讨中枢神经系统EB病毒(EBV)感染对EBV相关噬血细胞综合征(EBV-HLH)患者预后的影响。方法 回顾性分析2017年1月1日—2019年9月1日我院血液科诊治的88例EBV-HLH患者的临床资料,该88例患者全部完善腰椎穿刺及脑脊液EBV-DNA检测。临床资料包括患者性别、年龄、脑脊液EBV-DNA拷贝数、脑脊液白细胞、潘氏试验、脑脊液总蛋白、脑脊液葡萄糖,是否行异基因造血干细胞移植(allo-HSCT)、预后、生存时间等。结果 EBV+患者(44例)的脑脊液白细胞、潘氏试验、脑脊液总蛋白、脑脊液葡萄糖指标与EBV-患者(44例)比较,差异均无统计学意义;EBV+患者的生存时间明显差于EBV-患者(7.3个月vs 8.2个月,P=0.049)。行allo-HSCT患者(60例)的生存时间明显优于未行allo-HSCT患者(28例)(9.8个月vs 4.7个月,P=0.040)。在44例脑脊液EBV-DNA阳性患者中,行allo-HSCT患者(32例)的生存时间明显优于未行allo-HSCT患者(12例)(19.6个月vs 4.3个月,P< 0.001)。此44例患者脑脊液最高EBV-DNA拷贝数的中位数为1.0×104拷贝/mL,以1.0×104拷贝/mL为界,脑脊液EBV-DNA拷贝数高的患者(17例)生存时间明显差于脑脊液EBV-DNA拷贝数低的患者(27例)(5.2个月vs 17.0个月,P=0.030)。在31例多次进行脑脊液EBV-DNA检测的患者中,27例患者首次脑脊液EBV-DNA阳性。将此27例患者根据脑脊液EBV-DNA是否由阳性转为阴性分组,脑脊液EBV-DNA阳性转为阴性患者(16例)的生存时间明显优于脑脊液EBV-DNA持续阳性患者(11例)(9.4个月vs 5.0个月,P=0.038)。结论 在EBV-HLH患者中,中枢神经系统EBV感染是一个不良预后因素。脑脊液EBV-DNA拷贝数及变化趋势对EBV-HLH患者的预后存在影响,监测脑脊液EBV-DNA拷贝数变化具有重要意义。对于脑脊液EBV-DNA阳性的EBV-HLH患者,allo-HSCT可以改善其预后。
-
关键词:
- 噬血细胞综合征 /
- 中枢神经系统 /
- EB病毒感染 /
- 异基因造血干细胞移植
Abstract: Objective To explore the effect of EBV infection in central nervous system on the prognosis of patients with EBV-associated hemophagocytic lymphohistiocytosis(EBV-HLH).Methods Clinical data of 88 patients with EBV-HLH diagnosed and treated in our hospital from January 1, 2017 to September 1, 2019 were retrospectively analyzed. All 88 patients completed lumbar puncture and cerebrospinal fluid EBV-DNA detection. Clinical data included patients' gender, age, copy number of EBV-DNA in cerebrospinal fluid, cerebrospinal fluid leukocytes, pan test, cerebrospinal fluid total protein and glucose in routine biochemical examination of cerebrospinal fluid, whether allogeneic hematopoietic stem cell transplantation(allo-HSCT) was performed, prognosis, survival time and so on.Results There was no significant difference in cerebrospinal fluid leukocytes, pan test, cerebrospinal fluid total protein and glucose between EBV+ patients(44 cases) and EBV- patients(44 cases), and the survival time in EBV+ patients was significantly worse than that in EBV- patients(7.3 months vs 8.2 months,P=0.049). The survival time in patients underwent allo-HSCT(60 cases) was significantly better than that in patients without allo-HSCT(28 cases)(9.8 months vs 4.7 months,P=0.040). Among the 44 patients with EBV-DNA positive in cerebrospinal fluid, the survival time in patients underwent allo-HSCT(32 cases) was significantly better than that in patients without allo-HSCT(12 cases)(19.6 months vs 4.3 months,P< 0.001). The median of the highest EBV-DNA copy number in cerebrospinal fluid was 1.0×104 copies/mL, taking 1.0×104 copies/mL as the boundary, the survival time of patients with high EBV-DNA copy number in cerebrospinal fluid(17 cases) was significantly worse than that of patients with low EBV-DNA copy number in cerebrospinal fluid(27 cases)(5.2 months vs 17.0 months,P=0.030). Among 31 patients who underwent cerebrospinal fluid EBV-DNA detection for many times, 27 cases were positive for EBV-DNA in cerebrospinal fluid for the first time. And they were divided into 2 groups according to whether the cerebrospinal fluid EBV-DNA detection changed from positive to negative. The survival time of patients in the cerebrospinal fluid EBV-DNA changed from positive to negative group(16 cases) was significantly better than that in the cerebrospinal fluid EBV-DNA continuous positive group(11 cases)(9.4 months vs 5.0 months,P=0.038).Conclusion EBV infection of the central nervous system is a poor prognostic factor in patients with EBV-HLH. The EBV-DNA copy number and changes in EBV-DNA in cerebrospinal fluid can affect the prognosis of patients with EBV-HLH. It is of great significance to monitor the changes in EBV-DNA copy number in the cerebrospinal fluid. Allo-HSCT can improve the prognosis of EBV-HLH patients with EBV-DNA positive in cerebrospinal fluid. -

-
[1] 王昭, 王晶石. 成人噬血细胞综合征诊断与治疗进展[J]. 临床血液学杂志, 2022, 35(1): 1-5. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202201001.htm
[2] 刘艺, 郭涛. 血液系统肿瘤治疗相关噬血细胞综合征的诊疗进展[J]. 临床血液学杂志, 2022, 35(1): 16-20. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202201004.htm
[3] Tothova Z, Berliner N. Hemophagocytic Syndrome and Critical Illness: New Insights into Diagnosis and Management[J]. J Intensive Care Med, 2015, 30(7): 401-412. doi: 10.1177/0885066613517076
[4] Imashuku S. Treatment of Epstein-Barr virus-related hemophagocytic lymphohistiocytosis(EBV-HLH); update 2010[J]. J Pediatr Hematol Oncol, 2011, 33(1): 35-39. doi: 10.1097/MPH.0b013e3181f84a52
[5] Magaki S, Ostrzega N, Ho E, et al. Hemophagocytic lymphohistiocytosis associated with Epstein-Barr virus in the central nervous system[J]. Hum Pathol, 2017, 59: 108-112. doi: 10.1016/j.humpath.2016.07.033
[6] Jovanovic A, Kuzmanovic M, Kravljanac R, et al. Central nervous system involvement in hemophagocytic lymphohistiocytosis: A singlecenter experience[J]. Pediatr Neurol, 2014, 50(3): 233-237. doi: 10.1016/j.pediatrneurol.2013.10.014
[7] Horne A, Trottestam H, Aricò M, et al. Frequency and spectrum of central nervous system involvement in 193 children with haemophagocytic lymphohistiocytosis[J]. Br J Haematol, 2008, 140(3): 327-335. doi: 10.1111/j.1365-2141.2007.06922.x
[8] Henter JI, Horne A, Aricó M, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis[J]. Pediatr Blood Cancer, 2007, 48(2): 124-131. doi: 10.1002/pbc.21039
[9] Fryer JF, Heath AB, Wilkinson DE, et al. A collaborative study to establish the 1st WHO International Standard for Epstein-Barr virus for nucleic acid amplification techniques[J]. Biologicals, 2016, 44(5): 423-433. doi: 10.1016/j.biologicals.2016.04.010
[10] Wang Y, Camelo-Piragua S, Abdullah A, et al. Neuroimaging features of CNS histiocytosis syndromes[J]. Clin Imaging, 2020, 60(1): 131-140. doi: 10.1016/j.clinimag.2019.10.001
[11] Ma W, Li XJ, Li W, et al. MRI findings of central nervous system involvement in children with haemophagocytic lymphohistiocytosis: correlation with clinical biochemical tests[J]. Clin Radiol, 2021, 76(2): 9-17.
[12] Wang J, Wang Y, Wu L, et al. PEG-aspargase and DEP regimen combination therapy for refractory Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis[J]. J Hematol Oncol, 2016, 9(1): 84. doi: 10.1186/s13045-016-0317-7
[13] Chen J, Wang X, He P, et al. Viral etiology, clinical and laboratory features of adult hemophagocytic lymphohistiocytosis[J]. J Med Virol, 2016, 88(3): 541-549. doi: 10.1002/jmv.24359
[14] Jordan MB, Allen CE, Weitzman S, et al. How I treat hemophagocytic lymphohistiocytosis[J]. Blood, 2011, 118(15): 4041-4052. doi: 10.1182/blood-2011-03-278127
[15] SparberSauer M, Hönig M, Schulz AS, et al. Patients with early relapse of primary hemophagocytic syndromes or with persistent CNS involvement may benefit from immediate hematopoietic stem cell transplantation[J]. Bone Marrow Transplant, 2009, 44(6): 333-338. doi: 10.1038/bmt.2009.34
[16] Song Y, Pei RJ, Wang YN, et al. Central Nervous System Involvement in Hemophagocytic Lymphohistiocytosis in Adults: A Retrospective Analysis of 96 Patients in a Single Center[J]. Chin Med J, 2018, 131(7): 776-783. doi: 10.4103/0366-6999.228234
-




 下载:
下载: