-
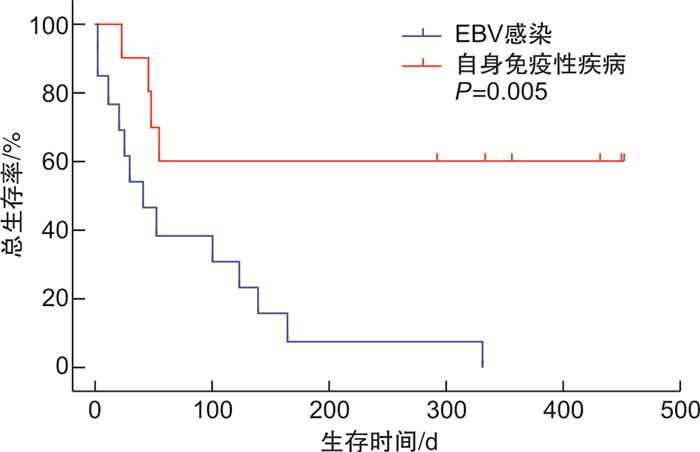
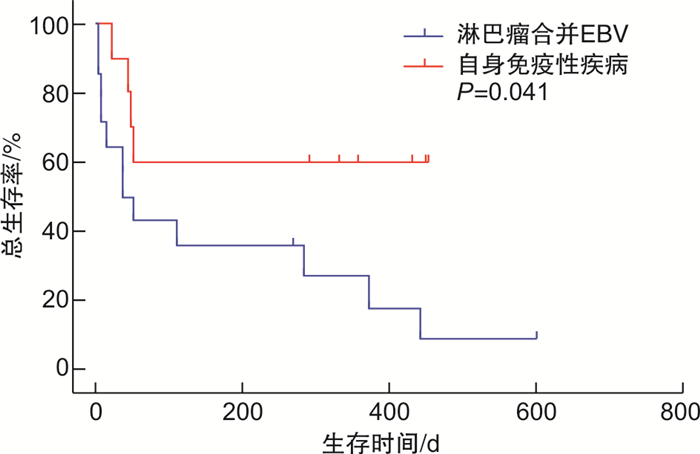
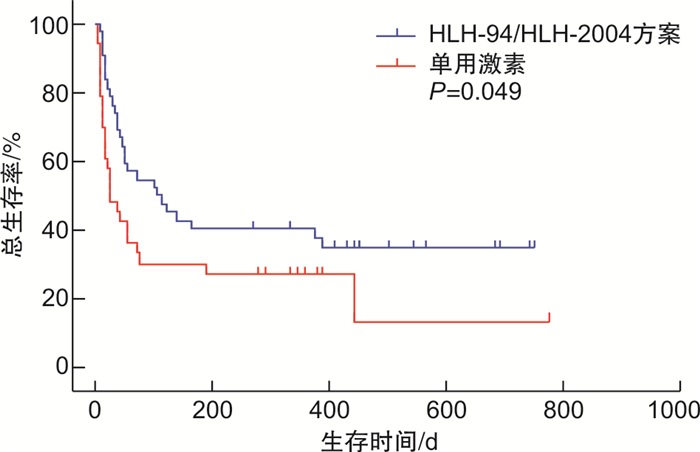
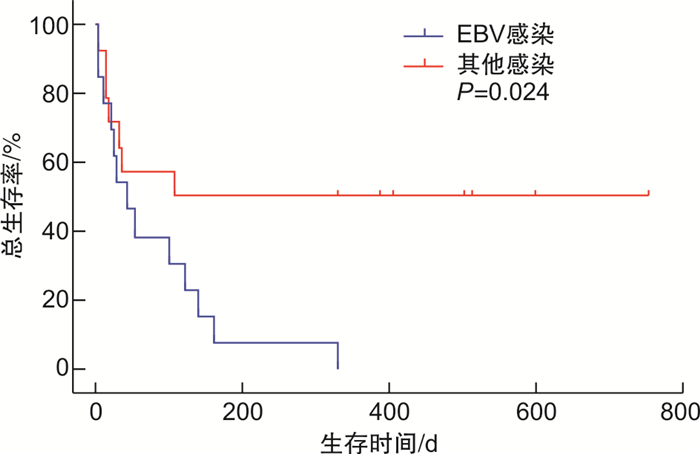
摘要: 目的 研究成人继发性噬血细胞综合征(HLH)患者的临床特征及预后相关因素。方法 回顾性分析2019年9月—2021年2月就诊于我院血液科的95例初诊继发性HLH患者的临床资料,分析其临床特征、治疗及预后因素。结果 95例患者的中位年龄51(19~79)岁;最常见病因为淋巴瘤,共34例(35.8%)。95例患者中64例(67.4%)死亡,中位生存时间72 d。Cox单因素分析表明,成人继发性HLH的预后受性别、中性粒细胞水平、血小板计数、肌酐、尿素氮、活化部分凝血活酶时间等因素影响(P< 0.05)。多因素Cox回归分析结果发现,中性粒细胞 < 1.0×109/L、活化部分凝血活酶时间>50 s、尿素氮升高是成人继发性HLH的独立预后影响因素(P< 0.05)。结论 成人继发性HLH的预后受多方面因素影响,中性粒细胞 < 1.0×109/L、活化部分凝血活酶时间>50 s、尿素氮升高是患者死亡的独立危险因素。Abstract: Objective To explore the clinical features and prognostic factors of adult patients with secondary hemophagocytic syndrome(HLH).Methods The clinical data of 95 newly diagnosed patients with secondary HLH who were hospitalized from September 2019 to February 2021 were retrospectively analyzed, and clinical features, survival, and prognostic factors of patients were analyzed.Results The median age of 95 patients was 51(19-79) years old. The most common cause was lymphoma, with 34 cases(35.8%). Of the 95 patients, 64 cases(67.4%) died and the median survival time was 72 days. Cox univariate analysis showed that sex, neutrophil level, platelet count, creatinine, urea nitrogen, and activated partial thromboplastin time were related to the prognosis of secondary HLH in adults(P< 0.05). Multivariate Cox regression analysis showed that neutrophil < 1.0×109/L, activated partial thromboplastin time>50 s, and elevated urea nitrogen were independent prognostic factors for secondary HLH in adults(P< 0.05).Conclusion The prognosis of adult secondary HLH is affected by many factors, neutrophil < 1.0×109L, activated partial thromboplastin time>50 s and elevated urea nitrogen are independent risk factors of death.
-
Key words:
- adult /
- hemophagocytic syndrome /
- clinical features /
- prognostic analysis
-

-
表 1 生存组与死亡组患者间发病年龄及检查结果比较
M(P25,P75) 因素 存活组(64例) 死亡组(31例) Z P 发病年龄/岁 48.0(32.0,58.0) 53.0(39.5,65.0) -1.485 0.138 血红蛋白/(g·L-1) 81.0(69.0,95.0) 83.0(70.3,93.0) -0.048 0.962 中性粒细胞/(×109·L-1) 3.9(1.1,5.3) 1.3(0.7,2.9) -0.279 0.005 PLT/(×109·L-1) 50.0(25.0,91.0) 22.5(12.3,41.8) -3.593 0.001 CRP/(mg·L-1) 64.0(31.6,112.9) 49.4(20.3,93.7) -0.633 0.527 降钙素原/(ng·mL-1) 1.0(0.4,5.1) 0.5(0.2,1.4) -2.029 0.042 ALT/(U·L-1) 93.0(35.0,128.0) 68.0(37.8,208.8) -0.127 0.899 AST/(U·L-1) 113.0(49.0,334.0) 144.5(52.0,340.0) -0.452 0.651 LDH/(U·L-1) 828.5(482.3,870.5) 1 255.0(574.0,2 469.0) -1.458 0.145 纤维蛋白原/(g·L-1) 1.3(0.9,3.0) 1.3(1.0,2.1) -0.131 0.896 TT/s 19.5(17.6,26.4) 20.6(17.7,28.0) -0.548 0.584 PT/s 13.2(12.4,14.5) 12.8(11.7,14.7) -0.619 0.536 APTT/s 31.9(29.4,38.3) 36.2(30.7,48.3) -2.084 0.037 D-二聚体/(mg·L-1) 6.8(2.3,17.1) 3.5(1.0,10.0) -1.631 0.103 肌酐/(μmol·L-1) 50.0(40.0,63.0) 67.0(49.5,86.0) -2.747 0.006 尿素氮/(mmol·L-1) 4.7(4.1,6.1) 7.4(5.3,10.1) -3.667 0.001 总胆红素/(μmol·L-1) 14.5(8.6,28.6) 23.4(13.5,61.3) -2.155 0.031 白蛋白/(g·L-1) 26.1(24.6,31.2) 26.7(23.6,29.1) -0.329 0.742 血钙/(mmol·L-1) 2.0(1.9,2.1) 2.0(1.9,2.1) -1.142 0.253 血钠/(mmol·L-1) 135.0(132.0,138.0) 135.0(131.0,138.0) -1.079 0.280 铁蛋白/(μmol·L-1) 15 043.5(1 962.3,41 067.3) 13 595.0(3 029.5,28 467.8) -0.219 0.827 甘油三酯/(mmol·L-1) 3.2(1.8,4.1) 2.7(2.1,3.6) -0.503 0.615 表 2 95例HLH患者预后影响因素的单因素和多因素分析
因素 单因素分析 多因素分析 HR(95%CI) P HR(95%CI) P 性别(男) 1.734(1.056~2.849) 0.030 1.176(0.671~2.061) 0.571 中性粒细胞 < 1.0×109/L 1.919(1.158~3.182) 0.013 1.723(1.027~2.894) 0.039 PLT < 100×109/L 3.332(1.044~10.635) 0.042 2.528(0.764~8.371) 0.129 肌酐 > 115 μmol/L 2.486(1.321~4.680) 0.005 1.133(0.512~2.504) 0.758 尿素氮 > 8.2 mmol/L 2.214(1.327~3.694) 0.002 1.897(1.065~3.381) 0.030 APTT > 50 s 2.261(1.245~4.108) 0.007 2.142(1.090~2.142) 0.027 降钙素原 > 4.6 ng/mL 0.523(0.225~1.215) 0.132 总胆红素 > 25 μmol/L 1.946(1.188~3.188) 0.080 -
[1] 噬血细胞综合征中国专家联盟, 中华医学会儿科学分会血液学组. 噬血细胞综合征诊治中国专家共识[J]. 中华医学杂志, 2018, 98(2): 91-95.
[2] Ponnatt TS, Lilley CM, Mirza KM. Hemophagocytic Lymphohistiocytosis[J]. Arch Pathol Lab Med, 2022, 146(4): 507-519. doi: 10.5858/arpa.2020-0802-RA
[3] Bhatt NS, Oshrine B, An Talano J. Hemophagocytic lymphohistiocytosis in adults[J]. Leuk Lymphoma, 2019, 60(1): 19-28. doi: 10.1080/10428194.2018.1482543
[4] Griffin G, Shenoi S, Hughes GC. Hemophagocytic lymphohistiocytosis: An update on pathogenesis, diagnosis, and therapy[J]. Best Pract Res Clin Rheumatol, 2020, 34(4): 101515. doi: 10.1016/j.berh.2020.101515
[5] Apodaca E, Rodríguez-Rodríguez S, Tuna-Aguilar EJ, et al. Prognostic Factors and Outcomes in Adults with Secondary Hemophagocytic Lymphohistiocytosis: A Single-center Experience[J]. Clin Lymphoma Myeloma Leuk, 2018, 18(10): e373-e380. doi: 10.1016/j.clml.2018.06.014
[6] 文菁菁, 许芳, 周巧林, 等. 成年人继发性噬血细胞综合征临床特点及预后分析[J]. 白血病·淋巴瘤, 2021, 30(2): 78-81.
[7] 张潇然, 刘业成, 刘继海, 等. EBV感染相关噬血细胞综合征患者的免疫功能评价及相关性分析[J]. 临床急诊杂志, 2020, 21(6): 437-441. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202006003.htm
[8] 沈子园, 贺晨露, 孙倩, 等. 124例成人噬血细胞综合征临床预后分析: 一项淮海淋巴瘤协作组多中心回顾性研究[J]. 中华血液学杂志, 2021, 42(10): 800-806. https://www.cnki.com.cn/Article/CJFDTOTAL-XZYX202110004.htm
[9] 赵晨星, 闫子勋, 胡建达. EBV阳性弥漫大B细胞淋巴瘤的诊疗进展[J]. 临床血液学杂志, 2020, 33(9): 654-658. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202009015.htm
[10] 吴凡, 张家奎, 陶千山, 等. 获得性噬血细胞综合征临床特征及预后研究[J]. 重庆医学, 2021, 50(4): 591-594. https://www.cnki.com.cn/Article/CJFDTOTAL-CQYX202104011.htm
[11] Song Y, Wang Y, Wang Z. Requirement for etoposide in the initial treatment of Epstein-Barr virus-associated haemophagocytic lymphohistiocytosis[J]. Br J Haematol, 2019, 186(5): 717-723. doi: 10.1111/bjh.15988
[12] 《中华传染病杂志》编辑委员会. 中国宏基因组学第二代测序技术检测感染病原体的临床应用专家共识[本文附更正][J]. 中华传染病杂志, 2020, 38(11): 681-689. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYX202107002.htm
[13] 高兴娟, 杨兴唐, 刘守珠, 等. ICU患者肺部真菌感染预测模型的建立和预测效能评价[J]. 临床血液学杂志, 2021, 34(6): 403-406, 411. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202106006.htm
[14] 王艳红, 胡佳佳, 巴俊慧, 等. 以多器官功能衰竭为表现的噬血细胞综合征25例分析[J]. 中华重症医学电子杂志(网络版), 2019, 5(4): 325-329. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZYD201904006.htm
[15] La Rosée P, Horne A, Hines M, et al. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults[J]. Blood, 2019, 133(23): 2465-2477. doi: 10.1182/blood.2018894618
[16] Song Y, Wang J, Wang Y, et al. Requirement for containing etoposide in the initial treatment of lymphoma associated hemophagocytic lymphohistiocytosis[J]. Cancer Biol Ther, 2021, 22(10-12): 598-606. doi: 10.1080/15384047.2021.1996139
[17] Naymagon L, Tremblay D, Mascarenhas J. The Efficacy of Etoposide-Based Therapy in Adult Secondary Hemophagocytic Lymphohistiocytosis[J]. Acta Haematol, 2021, 144(5): 560-568. doi: 10.1159/000514920
[18] Carter SJ, Tattersall RS, Ramanan AV. Macrophage activation syndrome in adults: recent advances in pathophysiology, diagnosis and treatment[J]. Rheumatology(Oxford), 2019, 58(1): 5-17. doi: 10.1093/rheumatology/key006
[19] Lu M, Xie Y, Guan X, et al. Clinical analysis and a novel risk predictive nomogram for 155 adult patients with hemophagocytic lymphohistiocytosis[J]. Ann Hematol, 2021, 100(9): 2181-2193. doi: 10.1007/s00277-021-04551-7
[20] Zhou M, Li L, Zhang Q, et al. Clinical features and outcomes in secondary adult hemophagocytic lymphohistiocytosis[J]. QJM, 2018, 111(1): 23-31. doi: 10.1093/qjmed/hcx183
[21] Zhao Y, Lu D, Ma S, et al. Risk factors of early death in adult patients with secondary hemophagocytic lymphohistiocytosis: a single-institution study of 171 Chinese patients[J]. Hematology, 2019, 24(1): 606-612. doi: 10.1080/16078454.2019.1660458
[22] 金魁, 王玉兰, 汪跃国, 等. 不同感染部位脓毒症急性肾损伤发生率及相关死亡风险分析[J]. 临床急诊杂志, 2021, 22(7): 445-452. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202107002.htm
[23] Esmaili H, Mostafidi E, Mehramuz B, et al. An update on renal involvement in hemophagocytic syndrome(macrophage activation syndrome)[J]. J Nephropathol, 2016, 5(1): 8-14.
[24] Wang J, Zhang R, Wu X, et al. Ruxolitinib-combined doxorubicin-etoposide-methylprednisolone regimen as a salvage therapy for refractory/relapsed haemophagocytic lymphohistiocytosis: a single-arm, multicentre, phase 2 trial[J]. Br J Haematol, 2021, 193(4): 761-768. doi: 10.1111/bjh.17331
[25] Boonstra PS, Ahmed A, Merrill SA, et al. Ruxolitinib in adult patients with secondary hemophagocytic lymphohistiocytosis[J]. Am J Hematol, 2021, 96(4): E103-E105.
[26] 尤亚红, 王晶石, 王昭. 噬血细胞性淋巴组织细胞增多症诊疗进展回顾[J]. 中华医学信息导报, 2021, 36(1): 10-10. https://www.cnki.com.cn/Article/CJFDTOTAL-JYYL201822050.htm
[27] Hua Z, He L, Zhang R, et al. Serum ferritin is a good indicator for predicting the efficacy of adult HLH induction therapy[J]. Ann Med, 2022, 54(1): 283-292. doi: 10.1080/07853890.2022.2027513
[28] Allen CE, Yu X, Kozinetz CA, et al. Highly elevated ferritin levels and the diagnosis of hemophagocytic lymphohistiocytosis[J]. Pediatr Blood Cancer, 2008, 50(6): 1227-1235. doi: 10.1002/pbc.21423
[29] Sarangi R, Pathak M, Padhi S, et al. Ferritin in hemophagocytic lymphohistiocytosis(HLH): current concepts and controversies[J]. Clin Chim Acta, 2020, 510: 408-415. doi: 10.1016/j.cca.2020.07.053
[30] Zhou J, Zhou J, Shen DT, et al. Development and validation of the prognostic value of ferritin in adult patients with hemophagocytic lymphohistiocytosis[J]. Orphanet J Rare Dis, 2020, 15(1): 71. doi: 10.1186/s13023-020-1336-6
[31] Zhou J, Zhou J, Wu ZQ, et al. A novel prognostic model for adult patients with hemophagocytic lymphohistiocytosis[J]. Orphanet J Rare Dis, 2020, 15(1): 215. doi: 10.1186/s13023-020-01496-4
-

| 引用本文: | 曹富娇, 郭洁, 姜中兴. 成人继发性噬血细胞综合征的临床特征及预后分析[J]. 临床血液学杂志, 2022, 35(9): 668-673. doi: 10.13201/j.issn.1004-2806.2022.09.012 |
| Citation: | CAO Fujiao, GUO Jie, JIANG Zhongxing. Clinical features and prognosis of adult secondary hemophagocytic syndrome[J]. J Clin Hematol, 2022, 35(9): 668-673. doi: 10.13201/j.issn.1004-2806.2022.09.012 |
- Figure 1.
- Figure 2.
- Figure 3.
- Figure 4.



 下载:
下载: