Comparison of clinical features and T lymphocyte subsets between myelodysplastic syndrome and aplastic anemia
-
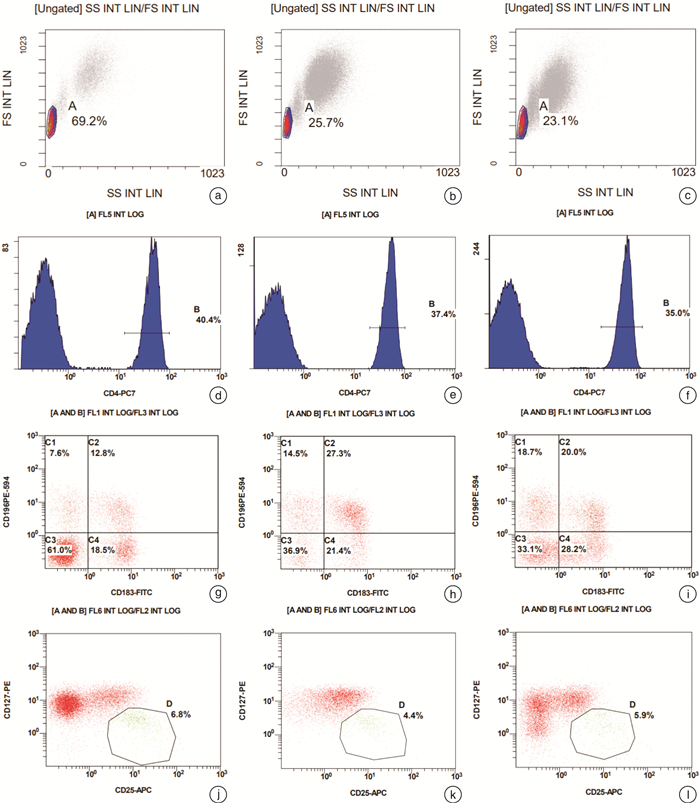
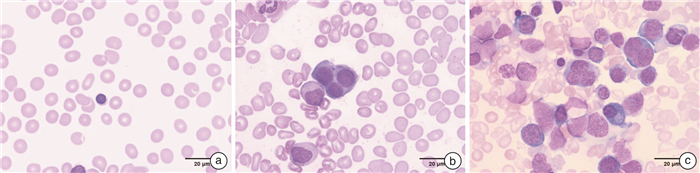
摘要: 目的 探讨再生障碍性贫血(AA)、AA继发骨髓增生异常综合征伴多系病态造血(MDS-MLD)和原发性MDS-MLD外周血常规及骨髓像特点,并分析T淋巴细胞亚群情况,为临床诊疗提供依据。方法 选取2021年1月1日至2021年10月30日就诊的AA、AA继发MDS-MLD和原发性MDS-MLD患者各15例,用流式细胞仪检测外周血常规中Th1、Th2、Th17和Treg淋巴细胞比例,分析2组间T淋巴亚群差异,并收集所有患者入组时骨髓形态学和细胞遗传学信息。结果 ① AA继发MDS-MLD相较于原发性MDS-MLD病程更长(P< 0.01);②AA相较于AA继发MDS-MLD外周血常规中淋巴细胞百分比明显升高(P< 0.05);③骨髓中AA继发MDS-MLD相较于AA红系增加(P< 0.05)、淋系减少(P< 0.01),原发性MDS-MLD相较于AA红系增加(P< 0.01)、淋系(P< 0.01)和粒红比(P< 0.05)减少,原发性MDS-MLD相较于AA继发MDS-MLD淋系减少(P< 0.05);④外周血中AA继发MDS-MLD相较于AA Th2细胞(P< 0.01)减低,Th17细胞(P< 0.01)、Th1/Th2(P< 0.05)和Th17/Treg(P< 0.01)增高;原发性MDS-MLD相较于AA Th2细胞(P< 0.05)减低,Th1/Th2水平(P< 0.05)增高;AA继发MDS-MLD相较于原发性MDS-MLD Th17细胞(P< 0.01)和Th17/Treg(P< 0.01)增高。结论 外周血常规和骨髓像中各系占比和细胞形态在AA和MDS-MLD鉴别中有重要作用,同时3组间T淋巴细胞各亚群存在差异,有助于临床诊疗。Abstract: Objective To investigate the characteristics of peripheral blood and bone marrow images of aplastic anemia (AA), AA secondary MDS-MLD and primary MDS-MLD, and analyze the T lymphocyte subsets, so as to provide evidence for clinical diagnosis and treatment.Methods Fifteen patients diagnosed as AA, AA secondary MDS-MLD and primary MDS-MLD in each group from Xiyuan Hospital, China Academy of Chinese Medical Sciences from January 1, 2021 to October 30, 2021 were selected. The proportion of Th1, Th2, Th17 and Treg lymphocytes in peripheral blood images were detected by flow cytometry. The differences in T lymphocyte subsets between the two groups were analyzed, and bone marrow morphological and cytogenetic information of all patients at enrollment was collected.Results ① AA secondary MDS-MLD had a longer course of disease than primary MDS-MLD(P< 0.01); ②Compared with AA secondary MDS-MLD, the percentage of lymphocytes in AA was significantly increased(P< 0.05); ③In bone marrow, AA secondary MDS-MLD compared with AA the erythrocytes increased(P< 0.05) and lymphocyte decreased(P< 0.01); primary MDS-MLD compared with AA the erythrocytes increased(P< 0.01), lymphocyte decreased(P< 0.01) and the granulocyte to erythrocyte ratio decreased(P< 0.05); primary MDS-MLD compared with AA secondary MDS-MLD lymphocyte decreased(P< 0.05); ④In the peripheral blood, AA secondary MDS-MLD compared with AA the Th2 decreased(P< 0.01), while Th17(P< 0.01), Th1/Th2(P< 0.05) and Th17/Treg(P< 0.01) levels increased; primary MDS-MLD compared with AA Th2 decreased(P< 0.05) and Th1/Th2 levels increased(P< 0.05); AA secondary MDS-MLD compared with primary MDS-MLD the Th17(P< 0.01) and Th17/Treg levels(P< 0.01) increased.Conclusion The proportion of each line and cell morphology in peripheral blood and bone marrow images might play an important role in the identification of AA and MDS-MLD. At the same time, there were differences in T lymphocyte subsets among the three groups, which may be helpful for clinical diagnosis and treatment.
-

-
表 1 3组一般情况
例,X±S 项目 AA
(15例)AA继发MDS
(15例)原发性MDS
(15例)性别 男 9 7 7 女 6 8 8 年龄/岁 30.40±18.72 33.93±12.60 43.40±20.43 病程/年 5.00±3.93 9.07±7.88 2.00±1.41 输血 否 10 7 13 是 5 8 2 表 2 3组外周血常规结果
X±S 项目 AA(15例) AA继发MDS(15例) 原发性MDS(15例) F/HC P WBC/(×109·L-1) 2.69±0.90 2.49±1.09 3.03±2.65 0.932 0.628 RBC/(×1012·L-1) 2.77±1.02 2.67±1.06 2.39±0.94 1.580 0.454 HGB/(g·L-1) 90.33±33.72 86.60±36.46 77.20±24.19 0.675 0.514 PLT/(×109·L-1) 38.87±30.22 31.80±35.99 62.07±67.14 2.510 0.285 GR/% 33.61±15.41 49.12±22.78 46.27±19.67 2.672 0.081 LY/% 60.31±15.03 43.21±18.21 47.34±18.40 3.999 0.026 表 3 3组骨髓像结果
例(%),X±S 项目 AA
(15例)AA继发MDS
(15例)原发性MDS
(15例)增生度 Ⅰ级 0 0 1(6.67) Ⅱ级 0 2(13.33) 6(40.00) Ⅲ级 2(13.33) 8(53.33) 7(46.67) Ⅳ级 9(60.00) 1(6.67) 1(6.67) Ⅴ级 4(26.67) 4(26.67) 0 粒系形态 异常 0 10(66.67) 14(93.33) 未见异常 15(100.00) 5(33.33) 1(6.67) 红系形态 异常 0 12(80.00) 14(93.33) 未见异常 15(100.00) 3(20.00) 1(6.67) 巨核形态 异常 0 3(20.00) 6(40.00) 未见异常 15(100.00) 12(80.00) 9(60.00) 粒系/% 26.73±10.38 38.33±15.97 36.67±15.36 红系/% 8.37±12.64 28.07±16.44 47.07±18.36 粒红比 7.33±9.86 2.55±5.29 1.06±0.95 淋系/% 63.23±17.43 31.57±20.17 15.20±11.30 表 4 3组T淋巴亚群结果
X±S 项目 AA(15例) AA继发MDS(15例) 原发性MDS(15例) F/HC P Th1细胞/% 7.39±2.38 8.81±2.85 9.78±3.28 2.646 0.083 Th2细胞/% 22.15±5.20 15.17±4.31 17.97±6.25 6.554 0.003 Th1/Th2 0.35±0.15 0.70±0.52 0.62±0.35 10.204 0.006 Th17细胞/% 4.80±2.36 7.49±2.74 5.07±1.97 5.848 0.006 Treg细胞/% 3.05±1.02 2.51±0.72 3.31±0.90 3.142 0.054 Th17/Treg 1.68±0.85 3.21±1.49 1.54±0.41 12.430 < 0.001 -
[1] Keel S, Geddis A. The clinical and laboratory evaluation of patients with suspected hypocellular marrow failure[J]. Hematology Am Soc Hematol Educ Program, 2021, 2021(1): 134-142. doi: 10.1182/hematology.2021000244
[2] Fenaux P, Haase D, Santini V, et al. Myelodysplastic syndromes: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2021, 32(2): 142-156. doi: 10.1016/j.annonc.2020.11.002
[3] 中华医学会血液学分会. 骨髓增生异常综合征中国诊断与治疗指南(2019年版)[J]. 中华血液学杂志, 2019, 40(2): 89-97.
[4] Killick SB, Bown N, Cavenagh J, et al. Guidelines for the diagnosis and management of adult aplastic anaemia[J]. Br J Haematol, 2016, 172(2): 187-207. doi: 10.1111/bjh.13853
[5] 中华医学会血液学分会红细胞疾病(贫血)学组. 再生障碍性贫血诊断治疗专家共识[J]. 中华血液学杂志, 2010, 31(11): 790-792. doi: 10.3760/cma.j.issn.0253-2727.2010.11.022
[6] Durrani J, Maciejewski JP. Idiopathic aplastic anemia vs hypocellular myelodysplastic syndrome[J]. Hematology Am Soc Hematol Educ Program, 2019, 2019(1): 97-104. doi: 10.1182/hematology.2019000019
[7] 张婷, 陈洋, 李瑞鑫, 等. 再生障碍性贫血髓系肿瘤基因突变靶向测序临床研究[J]. 临床血液学杂志, 2021, 34(3): 168-171. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202103006.htm
[8] Zhang D, Yu J, Liu L, et al. Acute arrest of hemopoiesis presenting as severe aplastic anemia: a retrospective analysis[J]. Hematology, 2021, 26(1): 1057-1063. doi: 10.1080/16078454.2021.2010329
[9] Wang Y, Huang L, Hua Y, et al. Impact of iron overload by transfusion on survival and leukemia transformation of myelodysplastic syndromes in a single center of China[J]. Hematology, 2021, 26(1): 874-880. doi: 10.1080/16078454.2021.1989806
[10] Bennett JM. Changes in the Updated 2016: WHO Classification of the Myelodysplastic Syndromes and Related Myeloid Neoplasms[J]. Clin Lymphoma Myeloma Leuk, 2016, 16(11): 607-609. doi: 10.1016/j.clml.2016.08.005
[11] Furlong E, Carter T. Aplastic anaemia: Current concepts in diagnosis and management[J]. J Paediatr Child Health, 2020, 56(7): 1023-1028. doi: 10.1111/jpc.14996
[12] Hellström-Lindberg E, Tobiasson M, Greenberg P. Myelodysplastic syndromes: moving towards personalized management[J]. Haematologica, 2020, 105(7): 1765-1779. doi: 10.3324/haematol.2020.248955
[13] 赵琴. 骨髓穿刺涂片联合活检病理切片在全血细胞减少性血液疾病诊断中的价值分析[J]. 临床医药文献电子杂志, 2019, 6(69): 131-132. https://www.cnki.com.cn/Article/CJFDTOTAL-LCWX201969116.htm
[14] Ai X, Li B, Xu Z, et al. Multiplex ligation-dependent probe amplification and fluorescence in situ hybridization for detecting chromosome abnormalities in myelodysplastic syndromes: A retrospective study[J]. Medicine(Baltimore), 2021, 100(18): e25768.
[15] Park S, Anderson NL, Canaria DA, et al. Granzyme-Producing CD4 T Cells in Cancer and Autoimmune Disease[J]. Immunohorizons, 2021, 5(12): 909-917. doi: 10.4049/immunohorizons.2100017
[16] Saenz SA, Local A, Carr T, et al. Small molecule allosteric inhibitors of RORγt block Th17-dependent inflammation and associated gene expression in vivo[J]. PLoS One, 2021, 16(11): e0248034. doi: 10.1371/journal.pone.0248034
[17] Li R, Wang R, Zhong S, et al. TGF-β1-overexpressing mesenchymal stem cells reciprocally regulate Th17/Treg cells by regulating the expression of IFN-γ[J]. Open Life Sci, 2021, 16(1): 1193-1202. doi: 10.1515/biol-2021-0118
[18] Reed J, Wetzel SA. Trogocytosis-Mediated Intracellular Signaling in CD4+ T Cells Drives TH2-Associated Effector Cytokine Production and Differentiation[J]. J Immunol, 2019, 202(10): 2873-2887. doi: 10.4049/jimmunol.1801577
[19] Giovazzino A, Leone S, Rubino V, et al. Reduced regulatory T cells(Treg)in bone marrow preferentially associate with the expansion of cytotoxic T lymphocytes in low risk MDS patients[J]. Br J Haematol, 2019, 185(2): 357-360. doi: 10.1111/bjh.15496
[20] 姚文亚. 骨髓增生异常综合征患者血清LDH、SF、Th17水平变化及临床价值[J]. 临床血液学杂志, 2022, 35(4): 264-267. https://whxhyy.xml-journal.net/article/doi/10.13201/j.issn.1004-2806.2022.04.007
[21] 唐旭东, 麻柔, 刘锋, 等. 再生障碍性贫血CD4+ /CD8+ T亚群的CD45RA+ /RO+ 表达与中医辨证分型的相关性研究[J]. 四川中医, 2006, 24(1): 14-16. https://www.cnki.com.cn/Article/CJFDTOTAL-SCZY200601007.htm
[22] 杨晓红, 唐旭东, 许勇钢, 等. 转录因子T-bet和GATA-3对再生障碍性贫血免疫失衡的作用[J]. 广东医学, 2010, 31(3): 290-292. https://www.cnki.com.cn/Article/CJFDTOTAL-GAYX201003013.htm
-




 下载:
下载: