Relationship between levels of PLT, D-D, autoantibody SOX2, MAGEA1 and PCNA and prognosis of patients with small cell lung cancer
-
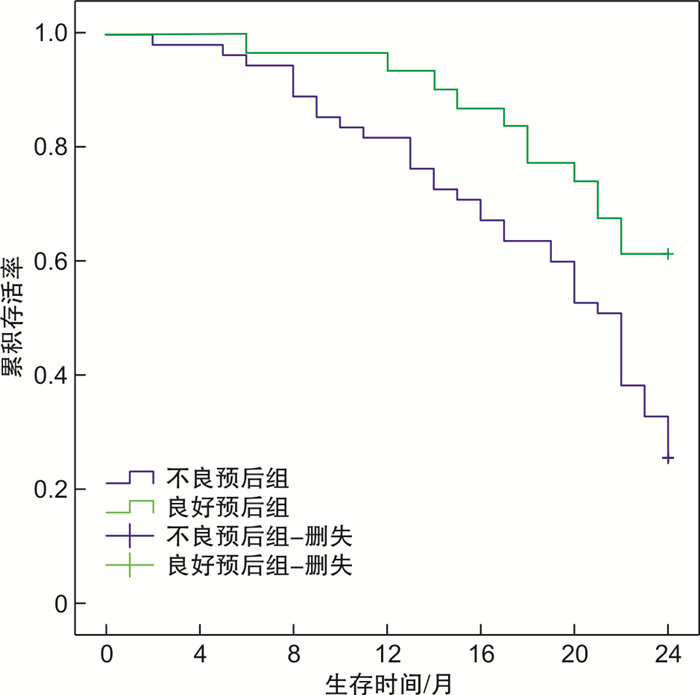
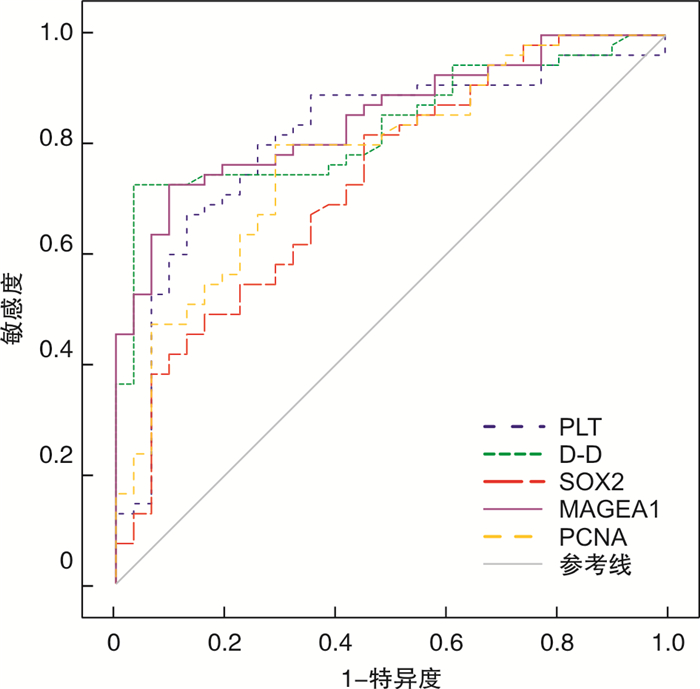
摘要: 目的 探究血小板计数(PLT)、D-二聚体(D-D)、自身抗体SOX2、MAGEA1、抗增殖细胞核抗原抗体(PCNA)水平与小细胞肺癌(SCLC)患者预后的关系。方法 回顾性分析2017年1月至2018年1月86例疑似SCLC患者的临床资料,根据随访1年内是否发生病情进展、死亡将其分为良好预后组31例与不良预后组55例,比较2组PLT、D-D、SOX2、MAGEA1、PCNA水平,采用logistic回归分析模型分析PLT、D-D、SOX2、MAGEA1、PCNA水平与SCLC患者预后情况的相关性,采用受试者工作特征(ROC)曲线评估上述指标对SCLC患者预后情况的预测效能,采用Kaplan-Meier生存曲线对2组患者2年内生存情况进行分析比较。结果 不良预后组PLT、D-D、SOX2、MAGEA1、PCNA水平均显著高于良好预后组(P < 0.05);logistic回归分析显示,PLT、D-D、SOX2、MAGEA1、PCNA水平与SCLC患者的预后具有显著相关性(P < 0.05);ROC曲线分析发现,上述指标预测SCLC患者预后情况的曲线下面积分别为0.810、0.834、0.731、0.849、0.777,截断值分别为287.02×109/L、2.34 mg/L、31.61 U/mL、13.52 U/mL、42.93%,预测效能良好(P < 0.05);Kaplan-Meier生存曲线分析显示,不良预后组平均生存期为18.50个月,显著短于良好预后组的21.35个月(P < 0.05)。结论 PLT、D-D、SOX2、MAGEA1、PCNA水平与SCLC患者的预后具有相关性,可用于评估SCLC患者预后生存情况。Abstract: Objective To explore the relationship between levels of platelet count(PLT), D-dimer(D-D), autoantibody SOX2, MAGEA1 and proliferating cell nuclear antigen(PCNA) and prognosis of patients with small cell lung cancer(SCLC).Methods The clinical data of 86 patients with suspected SCLC between January 2017 and January 2018 were retrospectively analyzed. According to whether the disease progression or death occurred within 1 year of follow-up, the patients were divided into good prognosis group(31 cases) and poor prognosis group(55 cases). The levels of PLT, D-D, SOX2, MAGEA1 and PCNA were compared between the two groups. Logistic regression analysis model was used to analyze the correlation between the levels of PLT, D-D, SOX2, MAGEA1 and PCNA and prognosis of patients with SCLC. Receiver operating characteristic(ROC) curve was used to evaluate the predictive efficiency of the above indicators on prognosis of patients with SCLC. Kaplan-Meier survival curve was used to analyze and compare the survival status within 2 years in the two groups of patients.Results The levels of PLT, D-D, SOX2, MAGEA1 and PCNA in poor prognosis group were significantly higher than those in good prognosis group(P < 0.05). Logistic regression analysis showed that the levels of PLT, D-D, SOX2, MAGEA1 and PCNA were significantly correlated with the prognosis of patients with SCLC(P < 0.05). ROC curve analysis found that the AUC values of the above indicators in predicting the prognosis of patients with SCLC were 0.810, 0.834, 0.731, 0.849 and 0.777, and the cut-off values were 287.02×109/L, 2.34 mg/L, 31.61 U/mL, 13.52 U/mL and 42.93% respectively, with good predictive efficiency(P < 0.05). Kaplan-Meier survival curve analysis showed that the average survival time with 18.50 months of poor prognosis group was significantly shorter than 21.35 months of good prognosis group(P < 0.05).Conclusion The levels of PLT, D-D, SOX2, MAGEA1 and PCNA may be correlated with the prognosis of patients with SCLC and can be used to evaluate the prognosis and survival status of patients with SCLC.
-
Key words:
- small cell lung cancer /
- platelet count /
- D-dimer /
- SOX2 /
- MAGEA1
-

-
表 1 2组PLT、D-D、SOX2、MAGEA1、PCNA水平比较
X±S 组别 例数 PLT /(×109·L-1) D-D /(mg·L-1) SOX2 /(U·L-1) MAGEA1 /(U·L-1) PCNA /% 不良预后组 55 297.01±30.41 2.68±0.86 39.85±10.17 15.48±4.03 50.29±10.34 良好预后组 31 264.99±25.33 1.71±0.62 29.54±12.59 9.97±3.53 39.27±9.60 t 4.967 5.517 4.137 6.357 4.866 P < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 表 2 PLT、D-D、SOX2、MAGEA1、PCNA水平与SCLC患者预后的相关性分析
指标 β SE Waldχ2 P OR PLT 0.249 0.066 14.233 < 0.001 1.282 D-D 0.251 0.073 11.822 < 0.001 1.285 SOX2 0.219 0.075 8.526 0.003 1.244 MAGEA1 0.209 0.068 9.446 0.002 1.232 PCNA 0.239 0.082 8.495 0.003 1.269 表 3 ROC曲线参数
指标 AUC 95%CI 敏感度/% 特异度/% PLT 0.810 0.711~0.887 87.10 67.27 D-D 0.834 0.739~0.906 96.77 72.73 SOX2 0.731 0.625~0.821 54.84 81.82 MAGEA1 0.849 0.755~0.917 90.32 72.73 PCNA 0.777 0.674~0.860 70.97 80.00 -
[1] 张磊, 任千里, 赵伟. 小细胞肺癌CT影像学特征及其组织病理特征相关性分析[J]. 中华肺部疾病杂志(电子版), 2021, 14(1): 101-104. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFBD202101020.htm
[2] Wang Y, Zou S, Zhao Z, et al. New insights into small-cell lung cancer development and therapy[J]. Cell BiolInt, 2020, 44(8): 1564-1576.
[3] Chauhan AF, Liu SV. Small Cell Lung Cancer: Advances in Diagnosis and Management[J]. Semin Respir Crit Care Med, 2020, 41(3): 435-446. doi: 10.1055/s-0039-1700566
[4] 张爽, 程颖. 小细胞肺癌治疗新进展[J]. 中国肿瘤临床, 2021, 48(10): 501-505. doi: 10.3969/j.issn.1000-8179.2021.10.048
[5] 薛守貌, 王凤丽. 非小细胞肺癌患者凝血功能与肿瘤转移复发的相关性研究[J]. 标记免疫分析与临床, 2021, 28(6): 993-996. https://www.cnki.com.cn/Article/CJFDTOTAL-BJMY202106022.htm
[6] 吾热丽卡·艾力, 迪力夏提·依明. 血清PCNA、TIMP-1水平检测联合SPECT检查对肺癌骨转移的诊断价值[J]. 中国医师杂志, 2021, 23(2): 211-214, 222.
[7] Schaefer T, Lengerke C. SOX2 protein biochemistry in stemness, reprogramming, and cancer: the PI3K/AKT/SOX2 axis and beyond[J]. Oncogene, 2020, 39(2): 278-292. doi: 10.1038/s41388-019-0997-x
[8] Iura K, Kohashi K, Yasutake N, et al. Cancer-testis antigens are predominantly expressed in uterine leiomyosarcoma compared with non-uterine leiomyosarcoma[J]. Oncol Lett, 2018, 15(1): 441-446.
[9] 王丽. 中国原发性肺癌诊疗规范(2015年版)[J]. 中华肿瘤杂志, 2015, 37(7): 433-436. https://www.cnki.com.cn/Article/CJFDTOTAL-GWHH201607001.htm
[10] 王珊珊, 王巍伟, 潘磊, 等. 肺癌患者凝血功能变化及其临床意义[J]. 标记免疫分析与临床, 2020, 27(10): 1637-1641. https://www.cnki.com.cn/Article/CJFDTOTAL-BJMY202010001.htm
[11] Hou C, Jiang F, Ma H, et al. Prognostic role of preoperative platelet, fibrinogen, and D-dimer levels in patients with non-small cell lung cancer: A multicenter prospective study[J]. Thorac Cancer, 2019, 10(2): 304-311.
[12] Pang M, Zhao F, Yu P, et al. The significance of coagulation and fibrinolysis-related parameters in predicting postoperative venous thrombosis in patients with breast cancer[J]. Gland Surg, 2021, 10(4): 1439-1446.
[13] Krause J, Frost CL. In Vitro Screening of Synthetic Fluorogenic Substrates for Detection of Cancer Procoagulant Activity[J]. Protein J, 2018, 37(2): 151-163.
[14] Gu RH, Tan B, Ma J, et al. Diagnostic value of the combined detection of CEA, NSE and IL-18 for lung cancer and their relationship with apoptosis gene Bcl-2[J]. J Biol Regul Homeost Agents, 2020, 34(5): 1637-1646.
[15] Wang Z, Kang L, Zhang H, et al. AKT drives SOX2 overexpression and cancer cell stemness in esophageal cancer by protecting SOX2 from UBR5-mediated degradation[J]. Oncogene, 2019, 38(26): 5250-5264.
-




 下载:
下载: