Clinical features and prognostic analysis of diffuse large B-cell lymphoma in oral cavity and maxillofacial region
-
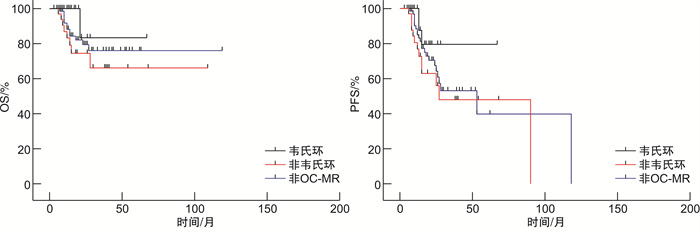
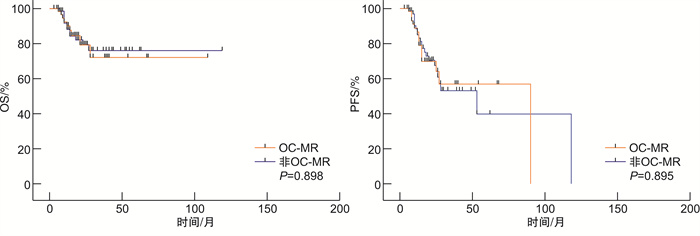
摘要: 目的 分析口腔颌面部弥漫大B细胞淋巴瘤(OC-MR DLBCL)患者临床特征,探讨其预后及可能影响因素。方法 回顾性收集2015年1月—2022年3月收治的60例OC-MR DLBCL患者临床资料,并与67例非OC-MR DLBCL患者进行比较。Kaplan-Meier法计算生存率,log-rank检验和Cox回归模型进行单因素及多因素生存预后分析。结果 60例OC-MR DLBCL患者中,男41例,女19例,中位年龄64岁;non-GCB型占71.4%,Ann Arbor Ⅰ/Ⅱ期占58.3%,60.0%患者属于IPI评分(0~2分)低危组。OC-MR DLBCL与非OC-MR DLBCL患者比较,性别、年龄及Hans分类分布差异无统计学意义,但Ⅲ/Ⅳ期及IPI高危患者占比均较低(P < 0.05)。OC-MR DLBCL患者ORR为91.7%,其中CR率60.0%,1年OS率为91.3%,2年OS率为63.6%;非OC-MR患者ORR为88.0%,CR率53.0%,1年OS率为89.6%,2年OS率为75.6%。OC-MR与非OC-MR组DLBCL患者间OS及PFS比较,差异无统计学意义(P>0.05))。生存分析显示IPI评分高危及起病于非韦氏环的OC-MR DLBCL患者预后不良,IPI是影响OS及PFS的独立预后因素(P < 0.05)。非OC-MR组患者生存较韦氏环起病患者差,优于非韦氏环者,但均差异无统计学意义(P>0.05)。结论 OC-MR DLBCL患者有特异性临床特征,多数处于早期及低危状态,整体预后不优于非OC-MR DLBCL。IPI及不同起病部位是影响OC-MR DLBCL预后的重要因素。Abstract: Objective To analyze the clinical features and explore the prognosis factors of patients with diffuse large B-cell lymphoma of oral cavity and maxillofacial region(OC-MR DLBCL).Methods The clinical data of 60 DLBCL patients in OC-MR and 67 DLBCL patients in non-OC-MR was collected retrospectively. All patients were treated at Shanghai Ninth People's Hospital between January 2015 and March 2022. Kaplan-Meier method was used to calculate survival rates, and the prognostic factors for survival were analyzed by using the log-rank univariate test and the Cox regression multivariate model.Results In this study, 60 OC-MR DLBCL patients with a median age of 64 years old were recruited, including 41 males and 19 females. The non-Germinal center B-cell-like(non-GCB) immunopheno type accounted for 71.4% in OC-MR DLBCL, Ann Arbor stage Ⅰ/Ⅱ accounted for 58.3%, and the low-risk IPI(score 0-2) accounted for 60.0%. Compared with non-OC-MR DLBCL patients, there were no significant differences in gender, age, and Hans classification distribution, while the Ann Arbor stage Ⅰ/Ⅱ, normal LDH, and low-risk IPI were more often in OC-MR DLBCL(P < 0.05). The objective response rate(ORR) and complete response(CR) rate for OC-MR DLBCL were 91.7% and 60.0%, The 1-year overall survival(OS) rate and 2-year OS rate were 91.3% and 63.6%. The ORR and CR for non-OC-MR DLBCL were 88.0% and 53.0%, the 1-year OS and 2-year OS were 89.6% and 75.6%. There were no significant difference in OS and progression-free survival(PFS) between OC-MR and non-OC-MR(P>0.05). Survival analysis showed that OC-MR DLBCL with high-risk IPI or disease originated in non-Waldeyer's ring had a poorer prognosis, high-risk IPI was the independent prognostic indicator(P < 0.05). The DLBCL of non-OC-MR had an inferior survival when compared to Waldeyer's ring originated DLBCL, but better than non-Waldeyer's ring originated OC-MR DLBCL, even though no significant differences(P>0.05).Conclusion OC-MR DLBCL patients display distinct clinical features, most of them are in an early and low-risk state. While the overall prognosis is not superior to non-OC-MR DLBCL. IPI and different primary sites of OC-MR seem to be important factors for prognosis of patients.
-
Key words:
- oral cavity /
- maxillofacial /
- diffuse large B-cell lymphoma /
- Waldeyer's ring /
- prognosis
-

-
表 1 OC-MR与非OC-MR DLBCL患者临床特征比较
例(%) 临床特征 OC-MR (n=60) 非OC-MR (n=67) P 性别 0.708 男 41(68.3) 43(64.2) 女 19(31.7) 24(35.8) 年龄/岁 0.203 ≤60 19(31.7) 29(43.3) >60 41(68.3) 38(56.7) Hans分型 0.417 GCB 17(28.3) 14(20.9) non-GCB 43(71.7) 50(74.6) 不清 0 3(4.5) Ann Arbor分期 <0.001 Ⅰ/Ⅱ 35(58.3) 17(25.4) Ⅲ/Ⅳ 25(41.7) 50(74.6) LDH 0.013 正常 35(58.3) 24(35.8) 升高 25(41.7) 43(64.2) ECOG评分/分 0.031 < 2 49(81.7) 43(64.2) ≥2 11(18.3) 24(35.8) 结外器官累及/个 0.148 < 2 29(48.3) 23(34.3) ≥2 31(51.7) 44(65.7) IPI评分/分 0.003 低危(0~2) 36(60.0) 22(32.8) 高危(3~5) 24(40.0) 45(67.2) Ki67/% 0.183 < 70 22(36.7) 17(25.4) ≥70 38(63.3) 50(74.6) 表 2 OC-MR与非OC-MR DLBCL患者预后的比较
疗效 OC-MR (n=60) 非OC-MR (n=67) P CR/例(%) 36(60.0) 37(55.2) 0.597 PR/例(%) 19(31.7) 23(34.3) 0.851 1年OS率/% 91.3 91.4 >0.990 2年OS率/% 63.6 75.6 0.385 1年PFS率/% 87.0 87.9 >0.990 2年PFS率/% 54.5 63.4 0.592 表 3 OC-MR DLBCL生存相关因素分析
临床特征 例数(%) OS PFS 单因素 多因素 单因素 多因素 P HR 95%CI P P HR 95%CI P 发病部位 0.037 3.88 0.7~72.3 0.205 0.05 2.19 0.68~9.74 0.232 韦氏环 27(45.0) 非韦氏环 33(55.0) Hans分型 0.709 0.483 GCB 17(28.3) non-GCB 43(71.7) IPI评分/分 0.003 0.10 0.01~0.53 0.028 0.002 0.26 0.06~0.67 0.012 低危(0~2) 36(60.0) 高危(3~5) 24(40.0) Ki67/% 0.249 0.449 < 70 22(36.7) ≥70 38(63.3) -
[1] Cabeçadas J, Martinez D, Andreasen S, et al. Lymphomas of the head and neck region: an update[J]. Virchows Arch, 2019, 474(6): 649-665. doi: 10.1007/s00428-019-02543-7
[2] Rodrigues-Fernandes CI, de Souza LL, Santos-Costa S, et al. Clinicopathological analysis of oral diffuse large B-cell lymphoma, NOS: A systematic review[J]. J Oral Pathol Med, 2019, 48(3): 185-191. doi: 10.1111/jop.12802
[3] Shi Y, Han Y, Yang J, et al. Clinical features and outcomes of diffuse large B-cell lymphoma based on nodal or extranodal primary sites of origin: Analysis of 1085 WHO classified cases in a single institution in China[J]. Chin J Cancer Res, 2019, 31(1): 152-161. doi: 10.21147/j.issn.1000-9604.2019.01.10
[4] Guevara-Canales JO, Morales-Vadillo R, Cava-Vergiú CE, et al. Survival in patients with oral and maxillofacial diffuse large B-cell lymphoma[J]. Braz Oral Res, 2013, 27(4): 349-355. doi: 10.1590/S1806-83242013005000018
[5] Zou H, Yang H, Zou Y, et al. Primary diffuse large B-cell lymphoma in the maxilla: A case report[J]. Medicine(Baltimore), 2018, 97(20): e10707.
[6] 谢萌, 张青青, 郭瑞昕, 等. 头颈部弥漫大B细胞淋巴瘤的临床特征分析[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(1): 1-7. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202201001.htm
[7] 黄丹丹, 杨全新, 黄玮, 等. 头颈不同部位结外非霍奇金淋巴瘤的病理及影像学特征比较[J]. 分子影像学杂志, 2020, 43(2): 207-212. https://www.cnki.com.cn/Article/CJFDTOTAL-FZYX202002006.htm
[8] Rodrigues-Fernandes CI, Junior AG, Soares CD, et al. Oral and oropharyngeal diffuse large B-cell lymphoma and high-grade B-cell lymphoma: A clinicopathologic and prognostic study of 69 cases[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2021, 131(4): 452-462. e4. doi: 10.1016/j.oooo.2020.11.005
[9] Li S, Young KH, Medeiros LJ. Diffuse large B-cell lymphoma[J]. Pathology, 2018, 50(1): 74-87. doi: 10.1016/j.pathol.2017.09.006
[10] Nowakowski GS, Feldman T, Rimsza LM, et al. Integrating precision medicine through evaluation of cell of origin in treatment planning for diffuse large B-cell lymphoma[J]. Blood Cancer J, 2019, 9(6): 48. doi: 10.1038/s41408-019-0208-6
[11] Abdelwahed Hussein MR. Non-Hodgkin's lymphoma of the oral cavity and maxillofacial region: a pathologist viewpoint[J]. Expert Rev Hematol, 2018, 11(9): 737-748. doi: 10.1080/17474086.2018.1506326
[12] Ruppert AS, Dixon JG, Salles G, et al. International prognostic indices in diffuse large B-cell lymphoma: a comparison of IPI, R-IPI, and NCCN-IPI[J]. Blood, 2020, 135(23): 2041-2048. doi: 10.1182/blood.2019002729
[13] 王小琴, 刘良发. 102例头颈部淋巴瘤的临床分析[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(2): 177-180. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202002019.htm
[14] Huber F, Zwickl-Traxler E, Pecherstorfer M, et al. Evaluation of Ki-67 as a Prognostic Marker in Diffuse Large B-Cell Lymphoma-A Single-Center Retrospective Cohort Study[J]. Curr Oncol, 2021, 28(6): 4521-4529. doi: 10.3390/curroncol28060383
[15] 孙悦, 许宏, 郭振清, 等. 探索18F-FDG PET/CT SUVmax、SUVsum及病理Ki67表达等在非霍奇金淋巴瘤中的临床应用价值[J]. 临床血液学杂志, 2021, 34(1): 18-23. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202101005.htm
[16] Xia S, Yue J, Chen X, et al. Clinicopathological and genetic characteristics of diffuse large B-cell lymphoma of the oropharyngeal and maxillofacial region[J]. Oral Dis, 2021, 27(3): 448-456. doi: 10.1111/odi.13578
[17] Tilly H, Morschhauser F, Sehn LH, et al. Polatuzumab Vedotin in Previously Untreated Diffuse Large B-Cell Lymphoma[J]. N Engl J Med, 2022, 386(4): 351-363. doi: 10.1056/NEJMoa2115304
[18] Yin X, Xu A, Fan F, et al. Incidence and Mortality Trends and Risk Prediction Nomogram for Extranodal Diffuse Large B-Cell Lymphoma: An Analysis of the Surveillance, Epidemiology, and End Results Database[J]. Front Oncol, 2019, 9: 1198. doi: 10.3389/fonc.2019.01198
[19] 刘睿, 黄方, 厉嘉琪, 等. 成人原发扁桃体弥漫大B细胞淋巴瘤预后预测模型的构建及其临床意义[J]. 临床血液学杂志, 2021, 34(3): 197-201. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202103012.htm
[20] Lee DY, Kang K, Jung H, et al. Extranodal involvement of diffuse large B-cell lymphoma in the head and neck: An indicator of good prognosis[J]. Auris Nasus Larynx, 2019, 46(1): 114-121. doi: 10.1016/j.anl.2018.05.006
[21] 李环, 吴涛, 刘秋琳, 等. 早期韦氏环弥漫大B细胞淋巴瘤预后分析[J]. 中华放射肿瘤学杂志, 2019, 28(12): 896-900. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLFY201605014.htm
[22] Jiang FF, Yan AH. Survival analysis of 8785 malignant lymphoma cases in the oral and nasal cavities in the USA: a cohort study[J]. BMJ Open, 2021, 11(12): e048876.
-




 下载:
下载: