-
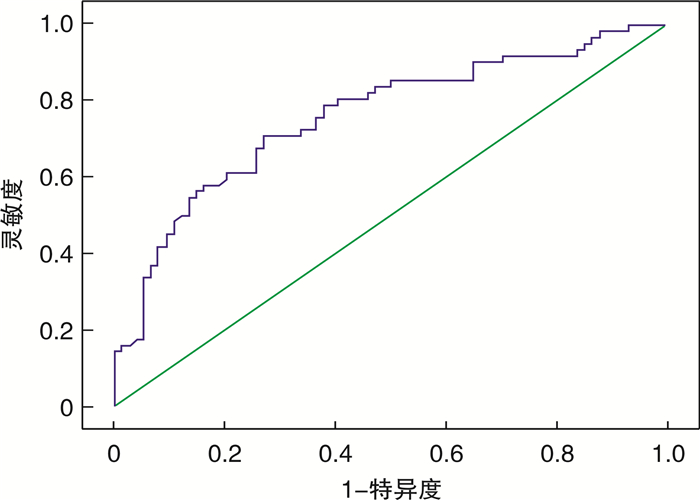
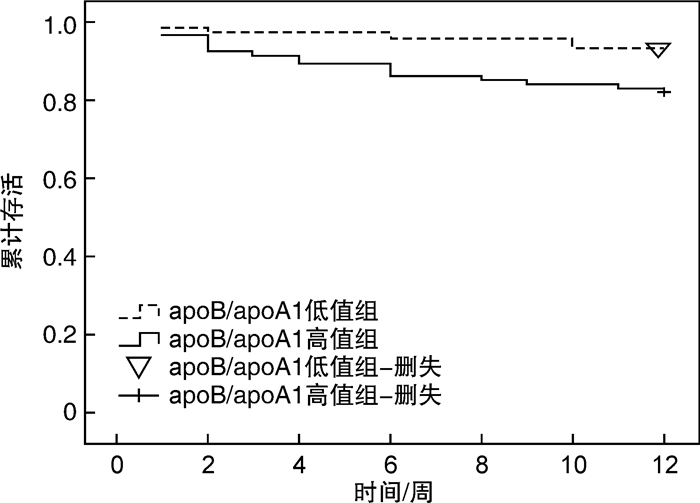
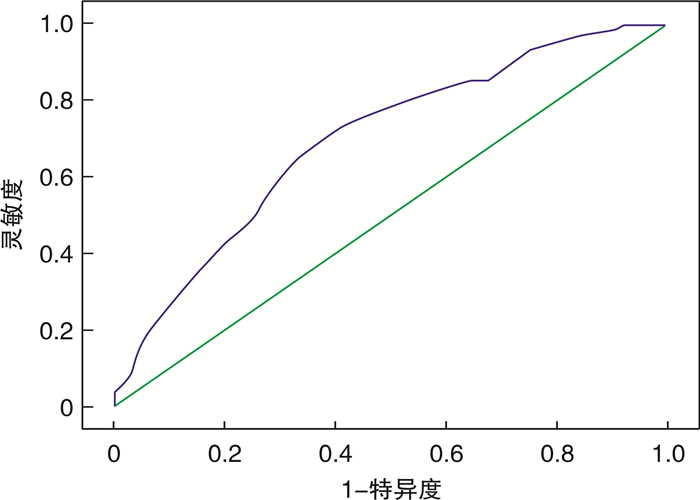
摘要: 目的 分析载脂蛋白B(apoB)/载脂蛋白A1(apoA1)对脑出血(ICH)患者预后不佳的影响和预测价值。方法 回顾性分析太和中医院治疗的ICH患者172例,收集患者入院时临床资料、血脂、出凝血功能等结果,根据发病后12周预后情况,将ICH分为预后不佳组和预后良好组,分析apoB/apoA1对预后不佳预测价值和影响。结果 apoB/apoA1预测ICH预后不佳曲线下面积为0.700(0.613~0.786),最佳截断值为0.850。apoB/apoA1高值组患者基底节出血占比、体重指数(BMI)、出血量≥30 mL占比、Rankin量表评分(mRS)3~6分占比、mRS 4~6分占比、死亡率、总胆固醇(TC)、总甘油三脂(TG)、低密度脂蛋白(LDL)、apoB、中性粒细胞/淋巴细胞(NLR)、红细胞分布宽度(RDW)、D二聚体(D-D)均明显高于低值组,HDL、apoA1明显低于低值组(P < 0.05)。校正各种混杂因素前后,apoA、apoB/apoA1均为mRS 3~6分、mRS 4~6分、全因死亡的影响因素(P>0.05),无论校正混杂因素与否,apoB均不为ICH全因死亡的影响因素(P>0.05)。单因素和多因素分析显示,年龄、基底节出血、出血量≥30 mL、apoB/apoA1≥0.850、NLR、D-D均为ICH预后不佳的独立影响因素(P < 0.05),OR值分别为1.879、2.842、2.319、6.520、2.742、3.026。综合指标(综合所有独立影响因素)预测ICH预后不佳曲线下面积为0.782(0.672~0.863)。Cox回归分析显示,ICH患者apoB/apoA1≥0.850死亡风险是apoB/apoA1 < 0.850的3.928倍。Kaplan-Meier生存曲线显示,apoB/apoA1低值组累计生存率高于apoB/apoA1高值组(χ2=4.969,P=0.026)。结论 apoB/apoA1对ICH预后不佳有一定的预测价值,且为预后不佳和全因死亡的影响因素。Abstract: Objective To analyze the predictive value of apolipoprotein B(apoB)/apolipoprotein A1(apoA1) for poor prognosis in patients with intracerebral hemorrhage(ICH).Methods A total of 172 patients with ICH in Taihe Hospital of Traditional Chinese Medicine were retrospectively analyzed. The clinical data, blood lipid and coagulation function were collected. According to the 12-weeks follow-up, patients were divided into poor prognosis group and good prognosis group, in order to analyze the predictive value and impact of apoB/apoA1 on poor prognosis.Results The AUC of apoB/apoA1 for predicting poor prognosis in ICH was 0.700(0.613-0.786), and the optimal cut-off value was 0.85. The proportion of basal ganglia bleeding, BMI, proportion of bleeding volume ≥ 30 mL, proportion of Rankin scale score(mRS) 3-6, proportion of mRS 4-6, mortality, total cholesterol(TC), total triglyceride(TG), low density lipoprotein(LDL), apoB, neutrophil/lymphocyte(NLR), red blood cell distribution width(RDW), D-dimer(D-D) in the apoB/apoA1 high group were significantly higher than those in the low group, while HDL and apoA1 were significantly lower than those in the low group(all P < 0.05). Before and after adjusting for various confounding factors, apoA and apoB/apoA1 were both influencing factors of mRS 3-6, mRS 4-6, and all-cause mortality(all P < 0.05), and regardless of whether confounding factors were adjusted or not, apoB was not an influencing factor of all-cause mortality in ICH(all P>0.05). The univariate and multivariate analysis showed that age, basal ganglia hemorrhage, hemorrhage volume ≥30 mL, apoB/apoA1≥0.85, NLR, and D-D were all independent influencing factors for poor prognosis in ICH(P < 0.05), the OR values were 1.879, 2.842, 2.319, 6.520, 2.742 and 3.026 respectively. The AUC of composite index(combining all independent influencing factors) for predicting poor prognosis in ICH was 0.782(0.672-0.863). The Cox regression analysis showed that the death risk of apoB/apoA1≥0.85 in patients with ICH was 3.928 times than that of apoB/apoA1 < 0.85. The Kaplan-Meier survival curve showed that the survival rate of the apoB/apoA1 low group was higher than that of the apoB/apoA1 high group(χ2=4.969, P=0.026).Conclusion apoB/apoA1 had a certain predictive value for poor prognosis in ICH, and was an influencing factor for poor prognosis and all-cause death.
-
Key words:
- intracerebral hemorrhage /
- apolipoprotein B /
- apolipoprotein A1 /
- poor prognosis /
- all-cause death
-

-
表 1 不同apoB/apoA1的ICH患者临床资料差异
临床资料 高值组(n=95) 低值组(n=77) t/χ2 P 男/例(%) 71(74.74) 56(72.73) 0.089 0.766 年龄/岁 63.11±9.62 62.25±10.01 0.573 0.568 BMI/(kg·m-2) 26.12(23.78,28.01) 25.57(23.01,27.85) 4.552 0.032 疾病史/例(%) 卒中 9(9.47) 8(10.39) 0.040 0.841 糖尿病 19(20.00) 13(16.88) 0.273 0.601 高血压 76(80.00) 55(71.43) 1.721 0.190 用药史/例(%) 抗血小板药物 13(13.68) 8(10.39) 0.431 0.512 糖尿病药物 16(16.84) 12(15.58) 0.049 0.824 降压药物 42(44.21) 39(50.65) 0.708 0.400 降脂药物 16(16.84) 18(23.38) 1.145 0.285 出血部位/例(%) 基底节 53(55.79) 31(40.26) 4.105 0.043 额叶 7(73.68) 6(7.79) 0.011 0.917 顶叶 10(10.53) 16(20.78) 3.484 0.062 枕页 5(5.26) 10(12.99) 3.187 0.074 丘脑 18(18.95) 12(15.58) 0.334 0.563 颞叶 10(10.53) 5(6.49) 0.869 0.351 出血量≥30 mL/例(%) 47(49.47) 25(32.47) 5.054 0.025 预后/例(%) 12周时mRS 3~6分 46(48.42) 14(18.18) 17.120 <0.001 12周时mRS 4~6分 38(40.00) 12(15.58) 12.296 <0.001 死亡 17(17.89) 5(6.49) 4.956 0.026 实验室指标 TG/(mmol·L-1) 1.61(1.13,2.12) 1.24(0.58,1.86) 2.175 0.033 TC/(mmol·L-1) 4.87(4.23,5.21) 4.22(3.81,4.92) 5.662 <0.001 HDL/(mmol·L-1) 1.06(0.75,1.56) 1.41(0.96,2.01) 5.321 <0.001 LDL/(mmol·L-1) 3.32(2.62,4.01) 3.09(2.08,3.85) 2.644 0.007 apoA1/(g·L-1) 1.18±0.27 1.51±0.32 7.335 <0.001 apoB/(g·L-1) 1.18±0.32 0.84±0.24 7.726 <0.001 PT/s 11.52±2.02 11.41±1.98 0.358 0.721 APTT/s 30.82±3.96 30.12±3.77 1.178 0.241 FIB/(g·L-1) 2.85±0.96 2.66±0.92 1.315 0.190 NLR 5.81±1.21 5.37±1.04 2.523 0.013 RDW/% 12.96±1.42 12.54±1.30 2.003 0.047 D-D/(mg·L-1) 3.85±1.42 3.42±1.24 2.089 0.038 表 2 血脂变量间相关性分析
变量 apoB/apoA1 TC TG HDL LDL apoA1 TC 0.367 TG 0.221 0.410 HDL -0.252 -0.102 -0.110 LDL 0.354 0.198 0.120 -0.096 apoA1 -0.570 0.252 0.087 0.421 0.102 apoB 0.512 0.554 0.321 0.094 0.498 0.110 表 3 apoB/apoA1与mRS、全因死亡关系
M(P25,P75) 变量 apoB apoA1 apoB/apoA1 OR(95%CI) P OR(95%CI) P OR(95%CI) P mRS 3~6分 模型1 2.31(1.09,9.13) 0.032 0.72(0.15,0.93) 0.032 3.01(1.52,7.95) 0.003 模型2 2.11(0.95,10.62) 0.095 0.78(0.23,0.95) 0.041 2.89(1.44,8.96) 0.015 模型3 4.14(1.24,20.11) 0.040 0.69(0.20,0.87) <0.001 5.15(2.02,14.72) <0.001 mRS 4~6分 模型1 1.64(0.89,6.31) 0.142 0.63(0.34,0.97) 0.036 2.15(1.47,11.21) 0.042 模型2 1.79(0.95,7.26) 0.102 0.69(0.21,0.84) 0.032 3.52(1.93,8.99) 0.017 模型3 3.17(1.21,14.32) 0.026 0.47(0.11,0.62) <0.001 4.41(2.17,10.79) 0.003 全因死亡 模型1 1.21(0.75,8.32) 0.321 0.64(0.21,0.81) 0.015 2.75(1.23,8.14) 0.035 模型2 1.75(0.81,10.33) 0.240 0.59(0.32,0.78) <0.001 2.54(1.37,7.95) 0.029 模型3 2.03(0.64,20.51) 0.374 0.71(0.22,0.86) 0.024 3.46(1.89,16.55) 0.037 模型1:未校正混杂因素;模型2:校正年龄、性别、BMI、基础疾病、用药史;模型3:校正HDL、LDL、TC、TG、PT、APTT、FIB、D-D。 表 4 ICH患者预后不佳的单因素、多因素分析
临床资料 单因素分析 t/χ2 P 多因素分析 P 预后不佳(n=82) 预后良好(n=90) OR 95%CI 男/例(%) 63(76.83) 64(71.11) 0.726 0.394 年龄/岁 64.52±8.52 61.09±9.14 2.539 0.012 1.879 1.104~6.792 0.040 BMI/(kg·m-2) 26.51(23.46,28.42) 25.19(23.02,27.55) 2.120 0.035 疾病史/例(%) 卒中 10(12.20) 8(8.89) 0.501 0.479 糖尿病 18(21.95) 14(15.56) 1.159 0.282 高血压 66(80.49) 65(72.22) 1.615 0.214 用药史/例(%) 抗血小板药物 12(14.63) 9(10.00) 0.860 0.354 糖尿病药物 13(15.85) 15(16.67) 0.021 0.885 降压药物 37(45.12) 44(48.89) 0.244 0.621 降脂药物 15(18.29) 19(21.11) 0.215 0.643 出血部位/例(%) 基底节 51(62.20) 33(36.67) 11.191 0.001 2.842 1.530~5.277 0.025 额叶 6(7.32) 7(7.78) 0.013 0.909 顶叶 16(19.51) 10(11.11) 2.360 0.124 枕页 9(10.98) 6(6.67) 1.001 0.317 丘脑 13(15.85) 17(18.89) 0.275 0.600 颞叶 11(13.41) 4(4.44) 4.337 0.037 出血量≥30 mL/例(%) 43(52.44) 29(32.22) 7.206 0.007 2.319 1.309~4.642 0.028 实验室指标 TG/(mmol·L-1) 1.63(1.17,2.18) 1.31(0.62,1.91) 2.096 0.038 TC/(mmol·L-1) 4.91(4.14,5.19) 4.30(3.85,5.01) 4.512 < 0.001 HDL/(mmol·L-1) 1.10(0.79,1.51) 1.37(0.89,2.01) 4.261 < 0.001 LDL/(mmol·L-1) 3.29(2.52,4.11) 3.01(2.14,4.02) 2.427 0.023 apoA1/(g·L-1) 1.06±0.34 1.57±0.41 8.832 < 0.001 apoB/(g·L-1) 1.09±0.36 0.97±0.31 2.348 0.020 apoB/apoA1≥0.85/例(%) 59(71.95) 23(25.56) 37.024 < 0.001 6.520 2.981~13.626 0.007 PT/s 11.50±2.31 11.44±2.14 0.177 0.860 APTT/s 31.17±4.74 29.90±4.51 1.800 0.074 FIB/(g·L-1) 2.79±0.89 2.74±0.76 0.397 0.692 NLR 5.86±1.32 5.38±1.26 2.439 0.016 2.742 1.120~8.547 0.035 RDW/% 13.02±1.44 12.55±1.62 2.033 0.047 D-D/(mg·L-1) 3.86±1.16 3.46±0.97 2.461 0.015 3.026 1.152~8.958 0.029 -
[1] 张亮, 张凤岐, 郑贵超, 等. 血清miRNA的表达对急性脑出血患者神经功能重建的指导价值[J]. 临床血液学杂志, 2020, 33(12): 835-839. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202012006.htm
[2] Krishnan K, Beishon L, Berge E, et al. Relationship between race and outcome in Asian, Black, and Caucasian patients with spontaneous intracerebral hemorrhage: Data from the Virtual International Stroke Trials Archive and Efficacy of Nitric Oxide in Stroke trial[J]. Int J Stroke, 2018, 13(4): 362-373. doi: 10.1177/1747493017744463
[3] Deng F, Li D, Lei L, et al. Association between apolipoprotein B/A1 ratio and coronary plaque vulnerability in patients with atherosclerotic cardiovascular disease: an intravascular optical coherence tomography study[J]. Cardiovasc Diabetol, 2021, 20(1): 1-13. doi: 10.1186/s12933-020-01183-5
[4] Lamprea-Montealegre JA, Staplin N, Herrington WG, et al. Apolipoprotein B, Triglyceride-Rich Lipoproteins, and Risk of Cardiovascular Events in Persons with CKD[J]. Clin J Am Soc Nephrol, 2020, 15(1): 47-60. doi: 10.2215/CJN.07320619
[5] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国脑出血诊治指南(2019)[J]. 中华神经科杂志, 2019, 52(12): 994-1005. doi: 10.3760/cma.j.issn.1006-7876.2019.12.003
[6] 张磊, 刘建民. 改良Rankin量表[J]. 中华神经外科杂志, 2012, 28(5): 512-512. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYZ201212056.htm
[7] 胡正涛, 张勇, 王俊, 等. 急性非创伤性脑出血患者肌钙蛋白Ⅰ升高的影响因素及临床意义[J]. 临床急诊杂志, 2021, 22(7): 453-457. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202107003.htm
[8] Kostapanos MS, Christogiannis LG, Bika E, et al. Apolipoprotein B-to-A1 ratio as a predictor of acute ischemic nonembolic stroke in elderly subjects[J]. J Stroke Cerebrovasc Dis, 2010, 19(6): 497-502. doi: 10.1016/j.jstrokecerebrovasdis.2009.09.010
[9] Bodde MC, Hermans M, Jukema JW, et al. Apolipoproteins A1, B, and apoB/apoA1 ratio are associated with first ST-segment elevation myocardial infarction but not with recurrent events during long-term follow-up[J]. Clin Res Cardiol, 2019, 108(5): 520-538. doi: 10.1007/s00392-018-1381-5
[10] 陈忠容, 秦家骏, 沈照立, 等. 高血压脑出血预后不良风险预测模型的构建与验证[J]. 同济大学学报(医学版), 2022, 43(2): 181-187. https://www.cnki.com.cn/Article/CJFDTOTAL-TJIY202202005.htm
[11] 杨帆, 杨国军, 杨哲. 北京地区3 139例首发脑出血患者流行特征及预后情况分析[J]. 华南预防医学, 2022, 48(1): 46-49, 54. https://www.cnki.com.cn/Article/CJFDTOTAL-GDWF202201011.htm
[12] Wang X, Wang Z, Li B, et al. Prognosis evaluation of universal acute coronary syndrome: the interplay between SYNTAX score and ApoB/ApoA1[J]. BMC Cardiovasc Disord, 2020, 20(1): 293. doi: 10.1186/s12872-020-01562-6
[13] 王宏宇, 付茜, 苏福祥. 载脂蛋白B/载脂蛋白A1比值与急性冠脉综合征患者冠状动脉多支病变及斑块易损性的相关性[J]. 中国医科大学学报, 2022, 51(7): 577-582. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGYK202207001.htm
[14] 张丽娟, 胡莉华, 靳志涛, 等. 载脂蛋白B与载脂蛋白A1比值与急性冠状动脉综合征患者冠状动脉病变程度及预后的相关性[J]. 中国心血管病研究, 2020, 18(8): 747-751. doi: 10.3969/j.issn.1672-5301.2020.08.016
[15] 郭清保, 杨彦龙, 史正华, 等. 血浆D-二聚体、HBP表达与高血压脑出血术后颅内感染及预后的关系[J]. 中西医结合心脑血管病杂志, 2022, 20(10): 1901-1903. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYY202210043.htm
[16] 钱程行, 方欢, 崔明, 等. 老年高血压基底节区脑出血患者微创术后短期预后的危险因素分析[J]. 国际外科学杂志, 2022, 49(4): 262-266.
[17] Reynoso-Villalpando GL, Sevillano-Collantes C, Valle Y, et al. ApoB/ApoA1 ratio and non-HDL-cholesterol/HDL-cholesterol ratio are associated to metabolic syndrome in patients with type 2 diabetes mellitus subjects and to ischemic cardiomyopathy in diabetic women[J]. Endocrinol Diabetes Nutr(Engl Ed), 2019, 66(8): 502-511.
[18] Alsamani R, Limin Z, Jianwei W, et al. Predictive value of the apolipoprotein B/A1 ratio in intracerebral hemorrhage outcomes[J]. J Clin Lab Anal, 2022, 36(7): e24562.
[19] Feng H, Wang X, Wang W, et al. Association Between Non-high-density Lipoprotein Cholesterol and 3-Month Prognosis in Patients With Spontaneous Intracerebral Hemorrhage[J]. Front Neurol, 2020, 11: 920.
-

| 引用本文: | 邹艺, 高强, 贺锋. 载脂蛋白B/载脂蛋白A1对脑出血预后预测价值的研究[J]. 临床血液学杂志, 2023, 36(4): 239-244. doi: 10.13201/j.issn.1004-2806.2023.04.004 |
| Citation: | ZOU Yi, GAO Qiang, HE Feng. Prognostic value of apolipoprotein B/apolipoprotein A1 in intracerebral hemorrhage[J]. J Clin Hematol, 2023, 36(4): 239-244. doi: 10.13201/j.issn.1004-2806.2023.04.004 |
- Figure 1.
- Figure 2.
- Figure 3.



 下载:
下载: