Effect of preoperative anemia on intraoperative blood transfusion in patients with acute craniocerebral injury
-
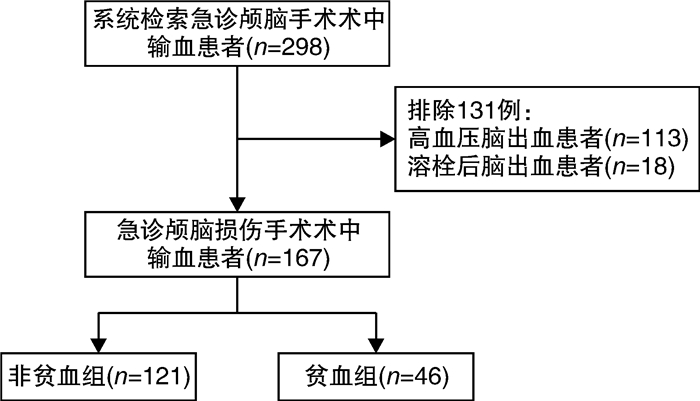
摘要: 目的 观察术前贫血对急性颅脑手术术中输血患者术后转归的影响。方法 回顾性分析2019年1月—2021年9月颅脑手术术中输血患者298例,其中167例纳入研究,按术前是否贫血[男性血红蛋白(Hb)≤120 g/L,女性Hb≤110 g/L]分为非贫血组(n=121例)和贫血组(n=46例),收集2组的临床资料、术中出血量、术中输血、术前和术后24 h实验室检查结果、术后住院天数、术后ICU停留时间及住院死亡率等数据进行统计分析。结果 ① 298例急性颅脑手术术前贫血发生率15.4%;②贫血组与非贫血组比较:术中出血量(1 110.22±619.39) mL vs (1 001.65±407.02) mL、术中输红细胞量(4.68±3.02) U vs (3.72±2.33) U,术后24 h Hb水平(87.59±13.49) g/L vs (107.11±16.84) g/L、术后24 h血小板计数(136.15±71.12)×109/L vs (146.95±50.18)×109/L,2组差异有统计学意义(P<0.05)。2组术中输冰冻血浆量、术后24 h红细胞分布宽度、术后住院天数、术后ICU停留时间差异无统计学意义(P>0.05);③贫血组住院死亡率(41.3%)明显高于非贫血组(18.2%),差异有统计学意义(P<0.05),2组术后ICU入住率差异无统计学意义;④logistic回归分析结果表明,术前贫血、术中输红细胞量和术前脑疝是住院死亡率的影响因素(P<0.05)。结论 术前贫血、术中输注红细胞量及术前并发脑疝是急性颅脑手术术中输血患者住院死亡率的独立影响因素;术前贫血能增加术中出血量、术中输红细胞量,而对术后住院天数及术后ICU停留时间无明显影响。Abstract: Objective To observe the effect of preoperative anemia on the postoperative outcome of patients with blood transfusion during acute craniocerebral surgery.Methods A total of 298 patients with intraoperative blood transfusion during craniocerebral surgery from January 2019 to September 2021 were searched by blood transfusion information management system, of which 167 were included in the study. They were divided into non anemia group(n=121 cases) and anemia group(n=46 cases) according to whether they were anaemic before surgery(male Hb ≤120 g/L, female Hb≤110 g/L). The clinical data, intraoperative bleeding amount, intraoperative blood transfusion, preoperative and postoperative 24 h laboratory examination results, postoperative hospital stay, postoperative ICU stay time and in-hospital mortality were measured by independent sample t-test. The rate was compared by chi square test. The in-hospital mortality was analyzed by logistic regression. The difference was statistically significant with P < 0.05.Results ① The incidence of anemia before acute craniocerebral surgery in 298 cases was 15.48%; ②Compared with the non anemia group, the amount of intraoperative bleeding(1 110.22±619.39) mL vs (1 001.65±407.02) mL, the amount of intraoperative red blood cell transfusion(4.68±3.02) U vs (3.72±2.33) U, the level of Hb at 24 h after operation(87.59±13.49) g/L vs (107.11±16.84) g/L, and the platelet count at 24 h after operation(136.15±71.12)×109/L vs (146.95±50.18)×109/L were significantly different between the two groups(P < 0.05). There was no significant differencein the amount of frozen plasma transfusion during operation, 24 h RDW after operation, postoperative hospital stay, and postoperative ICU stay time between the two groups (P>0.05); ③The mortality of anemia group(41.3%) was significantly higher than that of non anemia group(18.2%)(P < 0.05); There was no significant difference in ICU occupancy between the two groups. ④Logistic regression analysis showed that preoperative anemia, intraoperative red blood cell transfusion and preoperative cerebral hernia were the influencing factors of in-hospital mortality(P < 0.05).Conclusion Preoperative anemia, intraoperative transfusion of red blood cells and preoperative cerebral hernia were independent factors affecting the mortality of patients with intraoperative blood transfusion in acute craniocerebral surgery; Preoperative anemia could increase intraoperative bleeding and intraoperative red blood cell transfusion, but might have no significant effect on postoperative hospital stay and postoperative ICU stay.
-

-
表 1 贫血组和非贫血组患者基本临床资料比较
临床资料 贫血组(n=46) 非贫血组(n=121) F/χ2 P 年龄/岁 54.00±15.59 54.11±14.66 0.046 >0.05 不同年龄段/例(%) 0.214 >0.05 16~45岁 11(23.91) 33(27.27) 46~64岁 20(43.48) 54(44.63) ≥65岁 15(32.61) 34(28.10) 男/例(%) 35(76.09) 107(88.43) 2.728 >0.05 ABO血型分布/例(%) 5.281 >0.05 A型 22(47.83) 38(31.40) B型 13(28.26) 46(38.02) O型 10(21.74) 27(22.31) AB型 1(2.17) 10(8.26) 术前Hb/(g·L-1) 100.57±17.48 137.08±12.84 7.498 <0.05 脑损伤类型/例(%) 3.086 >0.05 开放性颅脑损伤 24(52.17) 45(37.19) 闭合性颅脑损伤 22(47.83) 76(62.81) 术前并发症/例(%) >0.05 脑疝 7(15.22) 27(22.31) 1.035 肺炎 13(28.26) 48(39.67) 1.871 糖尿病 1(2.17) 4(3.31) < 0.001 高血压 2(4.35) 5(4.13) 0.029 表 2 贫血组和非贫血组术中输血、术后24 h实验室指标及患者转归比较
指标 贫血组 非贫血组 F P 术中出血量/mL 1 110.22±619.39 1 001.65±407.02 9.193 0.003 术中输红细胞量/U 4.68±3.02 3.72±2.33 4.951 0.027 术中输冰冻血浆/mL 326.09±255.70 275.62±217.54 3.545 0.061 术后24 h Hb水平/(g·L-1) 87.59±13.49 107.11±16.84 5.254 0.023 术后24 h红细胞计数/(×1012·L-1) 3.32±0.93 2.59±1.09 2.141 0.145 术后24 h RDW 50.18±6.59 45.06±5.31 0.952 0.388 术后24 h血小板计数/(×109·L-1) 136.15±71.12 146.95±50.18 6.856 0.010 术后ICU停留时间/d 9.84±16.99 7.48±9.63 0.765 0.383 术后住院天数/d 31.57±30.83 33.07±32.77 1.137 0.288 表 3 贫血组和非贫血组间ICU入住率和住院死亡率比较
例(%) 指标 贫血组(n=46) 非贫血组(n=121) χ2 P ICU入住数 36(78.26) 103(85.12) 1.125 0.289 住院死亡数 19(41.30) 22(18.18) 9.620 0.002 表 4 术前贫血、术中输红细胞量、术前脑疝影响住院死亡率的logistic回归分析
指标 OR(95%CI) P 术前贫血 3.249(1.424~7.413) 0.005 术中输红细胞量 0.216(0.077~0.607) 0.004 术前脑疝 3.871(1.583~9.467) 0.003 -
[1] Abdullah HR, Sim YE, Sim YTM, et al. Preoperative ANemiA among the elderly undergoing major abdominal surgery(PANAMA) study: Protocol for a single-center observational cohort study of preoperative anemia management and the impact on healthcare outcomes[J]. Medicine(Baltimore), 2018, 97(21): e10838.
[2] Farshad M, Bauer DE, Wechsler C, et al. Risk factors for perioperative morbidity in spine surgeries of different complexities: a multivariate analysis of 1, 009 consecutive patients[J]. Spine J, 2018, 18(9): 1625-1631. doi: 10.1016/j.spinee.2018.02.003
[3] Mirchi N, Bissonnette V, Yilmaz R, et al. The Virtual Operative Assistant: an explainable artificial intelligence tool for simulation-based training in surgery and medicine[J]. PLoS One, 2020, 15(2): e0229596. doi: 10.1371/journal.pone.0229596
[4] Mosieri C, Chandler D, Reed DS, et al. Managing preoperative anemia: evolving concepts and strategies for improving patient outcomes[J]. Best Pract Res Clin Anaesthesiol, 2020, 34(2): 183-197. doi: 10.1016/j.bpa.2020.04.005
[5] Delaforce A, Galeel L, Poon E, et al. Preoperative Anemia screening and treatment practices in patients having total joint replacement surgery: a retrospective, observational audit[J]. J Blood Med, 2020, 11: 259-265. doi: 10.2147/JBM.S254116
[6] Agathis AZ, Khetan P, Bitner D, et al. Is preoperative anemia a significant risk factor for splenectomy patients? A NSQIP analysis[J]. Surg Open Sci, 2020, 2(3): 101-106. doi: 10.1016/j.sopen.2020.04.002
[7] Neef V, Choorapoikayil S, Piekarski F, et al. Current concepts in the evaluation and management of preoperative anemia[J]. Curr Opin Anaesthesiol, 2021, 34(3): 352-356. doi: 10.1097/ACO.0000000000000979
[8] 刘俊婷, 林洁, 周玲玲, 等. 某三甲医院神经外科患者术前贫血状况调查[J]. 中国输血杂志, 2020, 33(3): 201-205. https://www.cnki.com.cn/Article/CJFDTOTAL-BLOO202003007.htm
[9] Fowler AJ, Ahmad T, Phull MK, et al. Meta-analysis of the association between preoperative anaemia and mortality after surgery[J]. Br J Surg, 2015, 102(11): 1314-1324. doi: 10.1002/bjs.9861
[10] Ranucci M, Pavesi M, Pistuddi V, et al. Preoperative Anemia correction in cardiac surgery: a propensity-matched study[J]. J Cardiothorac Vasc Anesth, 2021, 35(3): 874-881. doi: 10.1053/j.jvca.2020.07.015
[11] Alan NM, Seicean A, Seicean S, et al. Impact of preoperative anemia on outcomes in patients undergoing elective cranial surgery[J]. J Neurosurg, 2014, 120(3): 764-772. doi: 10.3171/2013.10.JNS131028
[12] Kim BD, Edelstein AI, Patel AA, et al. Preoperative anemia does not predict complications after single-level lumbar fusion: a propensity score-matched multicenter study[J]. Spine, 2014, 39(23): 1981-1989. doi: 10.1097/BRS.0000000000000568
[13] 杨菲菲, 苑可欣, 任伟. 神经外科手术患者备血与用血特点分析与探讨[J]. 国际检验医学杂志, 2021, 42(14): 1675-1678. doi: 10.3969/j.issn.1673-4130.2021.14.003
[14] 陈铮立, 李建荣, 王树超, 等. 神经外科手术出血量的统计分析和输血策略[J]. 中国输血杂志, 2014, 27(4): 400-402. https://www.cnki.com.cn/Article/CJFDTOTAL-BLOO201404024.htm
[15] 刘丽萍, 胡燕, 何霞, 等. 红细胞输血在晚期肿瘤中的影响及预后价值[J]. 临床血液学杂志, 2022, 35(4): 252-255, 259. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2022.04.004
[16] Kellert L, Schrader F, Ringleb P, et al. The impact of low hemoglobin levels and transfusion on critical care patients with severe ischemic stroke[J]. J Crit Care, 2014, 29(2): 236-240. doi: 10.1016/j.jcrc.2013.11.008
[17] 张荣, 任天红, 杨鑫. 大量输血对急诊外伤患者T淋巴细胞亚群、凝血功能和炎症因子水平的影响[J]. 临床血液学杂志, 2022, 35(2): 96-99. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2022.02.003
[18] 杨文明, 丛明, 张振兴. 微创与开颅手术在脑出血治疗中的疗效及安全性比较[J]. 中华神经外科疾病研究杂志, 2014, 13(4): 360-361. https://www.cnki.com.cn/Article/CJFDTOTAL-SJWK201404027.htm
-




 下载:
下载: