Primary immune thrombocytopenia treated by splenectomy: a retrospective analysis of 61 cases
-
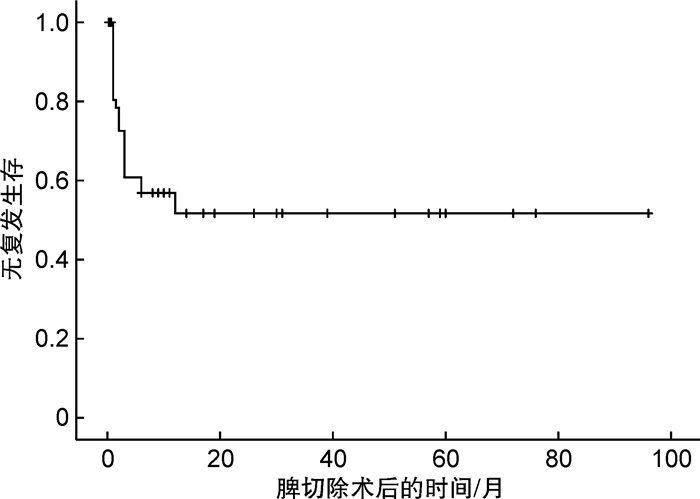
摘要: 目的 评估在血小板生成素受体激动剂等新药背景下脾切除术的疗效、安全性以及确定脾切除术后疗效的预测因素。方法 分析2014年1月—2021年12月进行脾切除术的61例原发性免疫性血小板减少症(primary immune thrombocytopenia,ITP)患者。结果 脾切除术后的PLT峰值中位数为393×109/L,达到PLT峰值的中位时间为5 d。54例(88.5%)患者达到了初始有效,7例(11.5%)患者疗效评定为无效。在进行随访后(中位随访时间为33个月),27例持续有效,24例出现ITP的复发,中位复发时间为2个月。脾切除术前最低PLT为脾切除术后疗效的重要预测因子(P=0.037)。未出现围手术期死亡患者,19例(31.1%)患者出现感染,2例(3.3%)患者出现血栓。结论 脾切除术是一种安全的治疗ITP的方式,能达到较高的持续有效率,切脾前最低的PLT显示出对切脾后疗效的预测价值。
-
关键词:
- 原发性免疫性血小板减少症 /
- 脾切除术 /
- 回顾性分析
Abstract: Objective To evaluate the current efficacy and safety of splenectomy in the context of new drugs such as thrombopoietin receptor agonists and to determine the predictors of efficacy after splenectomy.Methods A total of 61 patients with primary immune thrombocytopenia(ITP) who were admitted to our hospital from January 2014 to December 2021 and underwent splenectomy during this period were analyzed.Results The median platelet peak value after splenectomy was 393×109/L, and the median time to reach platelet peak value was 5 days. Among the 61 patients, 54 patients(88.5%) achieved initial response, and 7 patients(11.5%) were evaluated as NR. After follow-up(median follow-up, 33 months), 27 patients had sustained response, and 24 patients experienced relapse of ITP, with a median time of 2 months. The lowest platelet count before splenectomy was an important predictor of postoperative efficacy(P=0.037). There were no perioperative deaths, infection occurred in 19 patients(31.1%), and thrombosis occurred in 2 patients(3.3%).Conclusion Splenectomy is a safe method to treat ITP, which can achieve a high rate of sustained response. The lowest platelet count before splenectomy has predictive value of postoperative efficacy.-
Key words:
- primary immune thrombocytopenia /
- splenectomy /
- retrospective analysis
-

-
表 1 入组患者临床特征
指标 数值 切脾时年龄/岁 42(12~72) 男∶女/例 18∶43 从诊断ITP到切脾的时间/年 6.0(0.3~40.0) 疾病分期/例(%) 持续性 7(11.5) 慢性 54(88.5) 基线巨核细胞/个 168(7~1456) 血小板特异性抗体/例(%) (n=57) 血小板Ⅱb/Ⅲa抗体阳性 22(38.6) 血小板Ⅰb/Ⅸ抗体阳性 2(3.5) 血小板Ⅰa/Ⅱa抗体阳性 9(15.8) 免疫相关指标异常/例(%) (n=60) ANA阳性 43(71.7) 抗RO-52抗体阳性 19(31.7) 抗SS-A抗体阳性 15(25.0) 抗线粒体抗体阳性 6(10.0) 其他抗体阳性 9(15.0) 狼疮抗凝物阳性 8(13.3) 淋巴细胞亚群/% 淋巴细胞占有核细胞 21.8(4.4~48.2) CD3+T占淋巴细胞 74.5(40.0~88.2) CD3+CD4+T占淋巴细胞 37.8(15.3~79.7) CD3+CD8+T占淋巴细胞 31.1(18.0~60.8) CD3-CD16/CD56+NK细胞占淋巴细胞 7.1(0.9~31.0) CD3+CD16/CD56+NK样T细胞占淋巴细胞 4.3(0.4~12.5) CD19+B细胞占淋巴细胞 13.3(0.6~58.0) 脾切除术前最低PLT/(×109/L) 3(0~23) 切脾前1 d PLT/(×109/L) 57(1~397) 开腹手术∶微创手术(腹腔镜/机器人)/例 12∶49 表 2 脾切除术后的初始和长期疗效率
% 疗效 初始疗效 长期疗效 CR 83.6(51/61) 25.9(15/58) R 4.9(3/61) 20.7(12/58) NR 11.5(7/61) 12.1(7/58) 复发 — 47.1(24/51) 表 3 脾切除术后疗效不满意的单因素分析结果
指标 CR+R(n=27) NR+复发(n=31) OR(95%CI) P 切脾时的年龄/例(%) <40岁 11(40.7) 15(48.4) 1.364(0.481~3.865) 0.560 ≥40岁 16(59.3) 16(51.6) 性别/例(%) 女 22(81.5) 20(64.5) 0.413(0.122~1.397) 0.155 男 5(18.5) 11(35.5) 从诊断ITP到切脾的时间/例(%) <6年 13(48.1) 16(51.6) 1.149(0.409~3.226) 0.792 ≥6年 14(51.9) 15(48.4) 基线巨核细胞/例(%) <168个 15(55.6) 15(48.4) 0.750(0.266~2.113) 0.586 ≥168个 12(44.4) 16(51.6) 血小板特异性抗体/例(%) 血小板Ⅱb/Ⅲa抗体 阳性 10(41.7) 11(36.7) 0.811(0.270~2.435) 0.708 阴性 14(58.3) 19(63.3) 血小板Ⅰb/Ⅸ抗体/例(%) 阳性 0 2(6.7) - 1.000 阴性 24(100.0) 28(93.3) 血小板Ⅰa/Ⅱa抗体/例(%) 阳性 5(20.8) 3(10.0) 0.422(0.090~1.983) 0.275 阴性 19(79.2) 27(90.0) 免疫异常/例(%) 有 22(84.6) 24(77.4) 0.623(0.160~2.424) 0.495 无 4(15.4) 7(22.6) 淋巴细胞亚群/% 淋巴细胞占有核细胞 22.8±10.0 20.7±11.5 0.982(0.931~1.035) 0.496 CD3+T占淋巴细胞 73.5±11.5 76.4±8.0 1.019(0.964~1.076) 0.508 CD3+CD4+T占淋巴细胞 38.0±10.1 37.7±11.5 1.000(0.950~1.051) 0.985 CD3+CD8+T占淋巴细胞 28.0±9.7 31.5±8.2 1.053(0.986~1.125) 0.122 CD3-CD16/CD56+NK细胞占淋巴细胞 8.0±5.9 6.0±8.9 1.010(0.942~1.083) 0.784 CD3+CD16/CD56+NK样T细胞占淋巴细胞 3.9±3.0 4.4±3.4 1.059(0.857~1.309) 0.593 CD19+B细胞占淋巴细胞 13.2±13.4 13.1±8.3 0.976(0.927~1.026) 0.340 切脾前ITP相关治疗/例(%) 1~3种 4(14.8) 4(12.9) 0.852(0.191~3.792) 0.833 ≥3种 23(85.2) 27(87.1) 切脾前对糖皮质激素的反应/例(%) 激素无效 2(7.7) 8(26.7) 4.364(0.835~22.812) 0.081 激素依赖 24(92.3) 22(73.3) 切脾前对丙球的反应/例(%) NR 4(23.5) 8(29.6) 1.368(0.340~5.506) 0.659 CR+R 13(76.5) 19(70.4) 切脾前对TPORA的反应/例(%) NR 4(36.4) 6(66.7) 3.500(0.549~22.304) 0.185 CR+R 7(63.6) 3(33.3) 切脾前对利妥昔单抗的反应/例(%) NR 5(100.0) 5(100.0) - - CR+R 0 0 术前最低PLT/例(%) <3×109/L 8(29.6) 17(54.8) 2.884(0.972~8.556) 0.056 ≥3×109/L 19(70.4) 14(45.2) 术后PLT峰值/例(%) <300×109/L 8(29.6) 15(48.4) 2.227(0.752~6.593) 0.148 ≥300×109/L 19(70.4) 16(51.6) 表 4 开腹与腹腔镜/机器人进行脾切除术的疗效和并发症
例(%) 类型 开腹
(n=12)腹腔镜/机器人
(n=49)P 初始疗效 0.615 CR/R 10(83.3) 44(89.8) NR 2(16.7) 5(10.2) 长期疗效a 0.311 CR/R 3(30.0) 24(50.0) NR/复发 7(70.0) 24(50.0) 并发症 血栓 0 2(4.1) 1.000 感染 4(33.3) 15(30.6) 1.000 死亡 0 1(2.0) 1.000 a在开腹的12例患者和腹腔镜/机器人的49例患者中,分别有2例患者和1例患者因失访无法获得长期疗效的数据。 -
[1] Neunert C, Terrell DR, Arnold DM, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia[J]. Blood Adv, 2019, 3(23): 3829-3866. doi: 10.1182/bloodadvances.2019000966
[2] Wojcik I, Schmidt DE, de Neef LA, et al. A functional spleen contributes to afucosylated IgG in humans[J]. Sci Rep, 2021, 11(1): 24045. doi: 10.1038/s41598-021-03196-w
[3] Rodeghiero F. A critical appraisal of the evidence for the role of splenectomy in adults and children with ITP[J]. Br J Haematol, 2018, 181(2): 183-195. doi: 10.1111/bjh.15090
[4] 中华医学会血液学分会血栓与止血学组. 成人原发免疫性血小板减少症诊断与治疗中国指南(2020年版)[J]. 中华血液学杂志, 2020, 41(8): 617-623. https://www.cnki.com.cn/Article/CJFDTOTAL-LCLZ202106026.htm
[5] Ghanima W, Godeau B, Cines DB, et al. How I treat immune thrombocytopenia: the choice between splenectomy or a medical therapy as a second-line treatment[J]. Blood, 2012, 120(5): 960-969. doi: 10.1182/blood-2011-12-309153
[6] Finianos A, Mujadzic H, Peluso H, et al. Temporal trends and outcome of splenectomy in adults with immune thrombocytopenia in the USA[J]. Ann Hematol, 2021, 100(4): 941-952. doi: 10.1007/s00277-021-04449-4
[7] Avila ML, Amiri N, Pullenayegum E, et al. Long-term outcomes after splenectomy in children with immune thrombocytopenia: an update on the registry data from the Intercontinental Cooperative ITP Study Group[J]. Haematologica, 2020, 105(11): 2682-2685.
[8] Vibor M, Rogulj IM, Ostojic SK. Is there any Role for Splenectomy in Adulthood Onset Chronic Immun e Thrombocytopenia in the Era of TPO Receptors Agonists? A Critic al Overview[J]. Cardiovasc Hematol Disord Drug Targets, 2017, 17(1): 38-51.
[9] Caocci G, Efficace F, Mulas O, et al. Health-related quality of life profile of patients with immune thrombocytopenia in the real life is impaired by splenectomy[J]. Ann Hematol, 2022, 101(4): 749-754. doi: 10.1007/s00277-021-04750-2
[10] Boyle S, White RH, Brunson A, et al. Splenectomy and the incidence of venous thromboembolism and sepsis in patients with immune thrombocytopenia[J]. Blood, 2013, 121(23): 4782-4790. doi: 10.1182/blood-2012-12-467068
[11] Guan Y, Wang S, Xue F, et al. Long-term results of splenectomy in adult chronic immune thrombocytopenia[J]. Eur J Haematol, 2017, 98(3): 235-241. doi: 10.1111/ejh.12821
[12] Mageau A, Terriou L, Ebbo M, et al. Splenectomy for primary immune thrombocytopenia revisited in the era of thrombopoietin receptor agonists: New insights for an old treatment[J]. Am J Hematol, 2022, 97(1): 10-17. doi: 10.1002/ajh.26378
[13] Pincez T, Aladjidi N, Héritier S, et al. Determinants of long-term outcomes of splenectomy in pediatric autoimmune cytopenias[J]. Blood, 2022, 140(3): 253-261. doi: 10.1182/blood.2022015508
[14] Istl AC, McCreery G, Allen LJ, et al. Corticosteroid response predicts success of laparoscopic splenectomy in treating immune thrombocytopenia[J]. Surgery, 2018, 164(1): 71-76. doi: 10.1016/j.surg.2018.02.005
[15] Kumar S, Diehn FE, Gertz MA, et al. Splenectomy for immune thrombocytopenic purpura: long-term results and treatment of postsplenectomy relapses[J]. Ann Hematol, 2002, 81(6): 312-319. doi: 10.1007/s00277-002-0461-8
[16] Hammond WA, Vishnu P, Rodriguez EM, et al. Sequence of Splenectomy and Rituximab for the Treatment of Steroid-Refractory Immune Thrombocytopenia: Does It Matter?[J]. Mayo Clin Proc, 2019, 94(11): 2199-2208. doi: 10.1016/j.mayocp.2019.05.024
[17] Chaturvedi S, Arnold DM, McCrae KR. Splenectomy for immune thrombocytopenia: down but not out[J]. Blood, 2018, 131(11): 1172-1182. doi: 10.1182/blood-2017-09-742353
[18] Park YH, Yi HG, Kim CS, et al. Clinical Outcome and Predictive Factors in the Response to Splenectomy in Elderly Patients with Primary Immune Thrombocytopenia: A Multicenter Retrospective Study[J]. Acta Haematol, 2016, 135(3): 162-171. doi: 10.1159/000442703
[19] Kojouri K, Vesely SK, Terrell DR, et al. Splenectomy for adult patients with idiopathic thrombocytopenic purpura: a systematic review to assess long-term platelet count responses, prediction of response, and surgical complications[J]. Blood, 2004, 104(9): 2623-2634. doi: 10.1182/blood-2004-03-1168
[20] Navez J, Hubert C, Gigot JF, et al. Does the site of platelet sequestration predict the response to splenectomy in adult patients with immune thrombocytopenic purpura?[J]. Platelets, 2015, 26(6): 573-576. doi: 10.3109/09537104.2014.959915
[21] Amini SN, Nelson VS, Sobels A, et al. Autologous platelet scintigraphy and clinical outcome of splenectomy in immune thrombocytopenia: A systematic review and meta-analysis[J]. Crit Rev Oncol Hematol, 2020, 153: 103040. doi: 10.1016/j.critrevonc.2020.103040
[22] Ojima H, Kato T, Araki K, et al. Factors predicting long-term responses to splenectomy in patients with idiopathic thrombocytopenic purpura[J]. World J Surg, 2006, 30(4): 553-559. doi: 10.1007/s00268-005-7964-0
[23] Kim M, Park KM, Shin WY, et al. Platelet count evolution as a predictor of outcome after splenectomy for immune thrombocytopenic purpura[J]. Int J Hematol, 2017, 105(4): 433-439. doi: 10.1007/s12185-016-2121-0
[24] Canales-Herrerias P, Crickx E, Broketa M, et al. High-affinity autoreactive plasma cells disseminate through multiple organs in patients with immune thrombocytopenic purpura[J]. J Clin Invest, 2022, 132(12): e153580. doi: 10.1172/JCI153580
[25] Tastaldi L, Krpata DM, Prabhu AS, et al. Laparoscopic splenectomy for immune thrombocytopenia(ITP): long-term outcomes of a modern cohort[J]. Surg Endosc, 2019, 33(2): 475-485. doi: 10.1007/s00464-018-6321-y
[26] Tada K, Ohta M, Saga K, et al. Long-term outcomes of laparoscopic versus open splenectomy for immune thrombocytopenia[J]. Surg Today, 2018, 48(2): 180-185. doi: 10.1007/s00595-017-1570-2
[27] Thai LH, Mahévas M, Roudot-Thoraval F, et al. Long-term complications of splenectomy in adult immune thrombocytopenia[J]. Medicine, 2016, 95(48): e5098. doi: 10.1097/MD.0000000000005098
[28] Vianelli N, Palandri F, Polverelli N, et al. Splenectomy as a curative treatment for immune thrombocytopenia: a retrospective analysis of 233 patients with a minimum follow up of 10 years[J]. Haematologica, 2013, 98(6): 875-880. doi: 10.3324/haematol.2012.075648
[29] Kuchar E, Misśkiewicz K, Karlikowska M. A review of guidance on immunization in persons with defective or deficient splenic function[J]. Br J Haematol, 2015, 171(5): 683-694. doi: 10.1111/bjh.13660
[30] Di Sabatino A, Carsetti R, Corazza GR. Post-splenectomy and hyposplenic states[J]. Lancet, 2011, 378(9785): 86-97. doi: 10.1016/S0140-6736(10)61493-6
[31] 刘晓帆, 孙朝侠, 王志军, 等. 脾切除治疗74例成人原发免疫性血小板减少症的长期随访观察[J]. 临床血液学杂志, 2015, 28(9): 769-773. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ201509012.htm
-




 下载:
下载: