Clinical analysis of risk factors for early death in patients with hemophagocytic lymphohistiocytosis
-
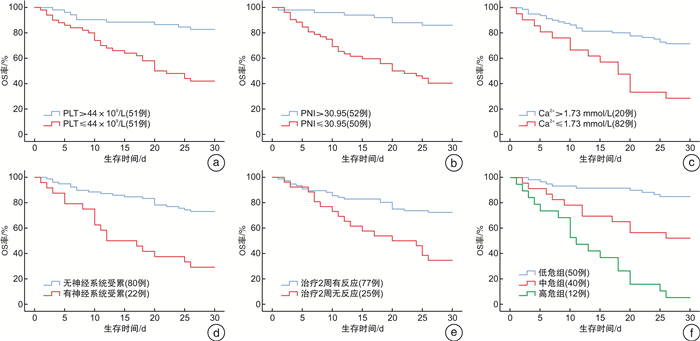
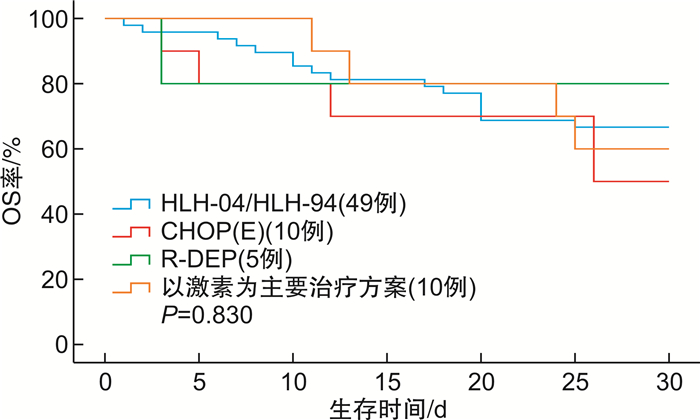
摘要: 目的 分析噬血细胞性淋巴组织细胞增生症(hemophagocytic lymphohistiocytosis,HLH)早期死亡患者的临床特征,探讨影响HLH患者早期死亡的可能危险因素,以期识别早期死亡风险高的患者。方法 回顾性分析2015年6月—2022年6月徐州医科大学附属医院收治的102例HLH患者的临床资料。根据是否于诊断后30 d内死亡,分为早期死亡组和早期存活组,比较2组患者的临床特征,应用Cox回归模型分析HLH患者早期死亡的独立危险因素。结果 102例HLH患者发生早期死亡38例,早期死亡率为37.3%,早期死亡患者的中位生存时间为11(2~30) d。对早期死亡患者与早期存活患者的临床特征进行分析,2组间在血小板计数(PLT)、白蛋白、预后营养指数、纤维蛋白原、乳酸脱氢酶、血钙(Ca2+)、是否发生深部器官出血、是否累及神经系统及治疗2周有无反应比较,差异有统计学意义(P < 0.05)。多因素Cox回归分析显示:PLT≤44×109/L(HR=0.346,95%CI 0.148~0.808,P=0.014)、预后营养指数≤30.95(HR=0.254,95%CI 0.083~0.774,P=0.016)、Ca2+≤1.73 mmol/L(HR=0.448,95%CI 0.225~0.891,P=0.022)、神经系统累及(HR=0.402,95%CI 0.177~0.915,P=0.030)及治疗2周无反应(HR=0.367,95%CI 0.140~0.958,P=0.041)是HLH患者早期死亡的独立危险因素。进一步按照危险因素的数量对HLH患者进行风险分层,低危组50例,中危组40例和高危组12例,3组患者30 d生存率分别为84.0%、47.5%和8.3%。与低危组患者比较,中危及高危组患者的早期死亡风险分别增加了14.8倍和48.1倍(P < 0.01)。结论 HLH早期死亡与多种因素相关,早期神经系统受累、PLT≤44×109/L、预后营养指数≤30.95、Ca2+≤1.73 mmol/L和治疗2周无反应是HLH患者早期死亡的独立危险因素;风险分层有助于识别高危患者,及时调整治疗策略从而降低早期死亡率。Abstract: Objective To analyze the clinical characteristics of early death patients with hemophagocytic lymphohistiocytosis(HLH), and to explore the possible risk factors affecting early death of HLH patients, in order to identify patients with high risk of early death.Methods The clinical data of 102 patients with HLH admitted to the Affiliated Hospital of Xuzhou Medical University from June 2015 to June 2022 were retrospectively analyzed. According to whether the patients died within 30 days after diagnosis, they were divided into early death group and early survival group. The clinical characteristics of the two groups were compared, and the independent risk factors of early death of HLH patients were analyzed by Cox regression model.Results Among 102 patients with HLH, 38 cases died early, the early mortality was 37.3%, and the median survival time of early death patients was 11(2-30) days. The clinical characteristics of early death patients and early survival patients were analyzed, and the differences between the two groups were statistically significant in platelet count, albumin, prognostic nutritional index, fibrinogen, lactate dehydrogenase, blood calcium, whether deep organ bleeding occurred, whether nervous system was involved, and whether there was reaction after 2 weeks of treatment(P < 0.05). Multi-factor Cox regression analysis showed that platelet ≤44×109/L(HR=0.346, 95%CI 0.148-0.808, P=0.014), prognostic nutrition index ≤30.95(HR=0.254, 95%CI 0.083-0.774, P=0.016), blood calcium ≤1.73 mmol/L(HR=0.448, 95%CI 0.225-0.891, P=0.022), nervous system involvement(HR=0.402, 95%CI 0.177-0.915, P=0.030) and no response after 2 weeks of treatment(HR=0.367, 95%CI 0.140-0.958, P=0.041) were independent risk factors for early death in patients with HLH. According to the number of risk factors, the patients with HLH were further risk stratified, with 50 patients in the low-risk group, 40 patients in the medium-risk group and 12 patients in the high-risk group. The 30-day survival rates of the three groups were 84.0%, 47.5% and 8.3%, respectively. Compared with the low-risk group, the risk of early death in the medium-risk and high-risk group was 14.8 and 48.1 times higher, respectively(P < 0.01).Conclusion The early death of HLH patients is related to various factors. Early neurological involvement, platelet ≤44×109/L, prognostic nutrient index≤30.95, blood calcium≤1.73 mmol/L and non-response for 2 weeks of treatment are independent risk factors for early death of HLH patients. Risk stratification is helpful to identify high-risk patients and timely adjust treatment strategies to reduce early mortality.
-
Key words:
- lymphohistiocytosis /
- hemophagocytic /
- early death /
- risk factors
-

-
表 1 HLH患者早期死亡组与早期存活组临床特征及实验室参数比较
特征 早期死亡组(38例) 早期存活组(64例) t/z/χ2 P 年龄/岁 54(15~82) 46(14~74) -1.904 0.057 性别(男/女)/例 22/16 33/31 0.385 0.535 发热持续时间/d 11(8~20) 10(6~18) 5.321 0.194 肝脾肿大/例(%) 21(55.3) 41(64.1) 0.774 0.379 淋巴结肿大/例(%) 15(39.5) 32(50.0) 1.063 0.302 浆膜腔积液/例(%) 14(36.8) 13(20.3) 3.347 0.067 深部器官出血/例(%) 11(28.9) 7(10.9) 5.321 0.021 DIC/例(%) 7(18.4) 5(18.4) 2.585 0.108 神经系统受累/例(%) 15(39.5) 7(10.9) 12.059 0.001 恶性肿瘤相关/例(%) 18(47.4) 21(32.8) 2.139 0.144 HLH-2004/HLH-1994治疗/例(%) 16(51.6) 33(32.4) 1.002 0.317 治疗2周反应/例(%) 10.134 0.001 CR或PR 22(57.9) 55(85.9) NR 16(42.1) 9(14.1) Hb/(g/L) 87(18~122) 93(37~136) 1.956 0.054 ALC/(×109/L) 0.4(0.1~1.9) 0.8(0.1~4.1) -1.764 0.078 ANC/(×109/L) 1.1(0~12.0) 1.6(0~13.2) -0.768 0.442 PLT/(×109/L) 28.5(3.0~133.0) 55(10~221) -4.168 <0.001 铁蛋白/(μg/L) 3 048(362~163 885) 2 256(667~147 680) -1.028 0.304 TG/(mmol/L) 2.4(0.6~30.5) 2.6(0.9~21.2) -0.071 0.943 ALB/(g/L) 24.9(18.7~32.9) 29.3(17.7~44.7) 4.469 0.003 PNI 29.8(20.2~41.8) 33.4(22.7~49.9) -3.060 0.002 ALT/(U/L) 99(12~1174) 69(8~931) -1.886 0.059 AST/(U/L) 155.5(12.0~4 900.0) 87(6~1 297) -1.903 0.057 AKP/(U/L) 188(55~3 998) 153.2(39.0~4 012.0) -1.550 0.121 γ-GT/(U/L) 144.5(19~4 306) 99(10~3 745) -1.236 0.217 TBIL/(mmol/L) 36.2(4.7~315.7) 19.6(5.6~221.6) -1.855 0.064 DBIL/(mmol/L) 24.0(2.5~245.5) 13.3(0.4~173.7) -1.883 0.060 LDH/(U/L) 1 570.5(175.0~10 245.0) 797(119~20 538) -2.069 0.039 Scr/(μmol/L) 67(28~235) 61.5(29.0~223.0) -1.686 0.092 FIB/(g/L) 1.2(0.3~5.1) 1.8(0.4~6.1) -2.194 0.028 PT/s 13.8(10.5~21.4) 13.2(9.0~72.3) -1.880 0.060 APTT/s 37.3(22.8~110.3) 36.7(19.4~100.3) -0.478 0.633 Ca2+/(mmol/L) 1.9(1.1~2.6) 2.0(1.6~2.8) -3.152 0.002 K/(mmol/L) 3.6(2.3~4.9) 3.7(2.1~5.8) 1.253 0.213 CRP/(mg/L) 64.5(10.2~237.9) 55.0(5.2~198.0) -0.651 0.515 NT-proBNP/(ng/L) 394(108~28 413) 332(66~16 678) -0.890 0.373 EBV感染/例(%) 13(34.2) 12(18.8) 3.080 0.079 噬血现象/例(%) 34(89.5) 50(78.1) 2.113 0.146 表 2 HLH患者早期死亡危险因素的单因素与多因素分析
影响因素 单因素分析 多因素分析 HR(95%CI) P HR(95%CI) P PLT≤44×109/L 0.201(0.092~0.440) < 0.001 0.346(0.148~0.808) 0.014 ALB≤26.9 g/L 0.389(0.204~0.742) 0.004 1.034(0.452~2.383) 0.930 PNI≤30.95 0.196(0.089~0.428) < 0.001 0.254(0.083~0.774) 0.016 FIB≤1.38 g/L 0.410(0.209~0.802) 0.009 0.563(0.244~1.298) 0.177 Ca2+≤1.73 mmol/L 0.317(0.163~0.615) 0.001 0.448(0.225~0.891) 0.022 神经系统受累 0.324(0.157~0.670) 0.002 0.402(0.177~0.915) 0.030 治疗2周无反应 0.341(0.180~0.649) 0.001 0.367(0.140~0.958) 0.041 深部器官出血 0.433(0.215~0.875) 0.020 1.278(0.417~3.914) 0.667 LDH≥1 200 U/L 1.854(0.967~3.554) 0.063 -
[1] 曹富娇, 郭洁, 姜中兴. 成人继发性噬血细胞综合征的临床特征及预后分析[J]. 临床血液学杂志, 2022, 35(9): 668-673. doi: 10.13201/j.issn.1004-2806.2022.09.012
[2] 曹靖伟, 贺华文, 陈蕾蕾等. 11例黑热病相关噬血细胞综合征的临床特点分析[J]. 临床血液学杂志, 2022, 35(11): 801-804. doi: 10.13201/j.issn.1004-2806.2022.11.009
[3] Yildiz H, Bailly S, van Den Neste E, et al. Clinical management of relapsed/refractory hemophagocytic lymphohistiocytosis in adult patients: a review of current strategies and emerging therapies[J]. Ther Clin Risk Manag, 2021, 17: 293-304. doi: 10.2147/TCRM.S195538
[4] Ponnatt TS, Lilley CM, Mirza KM. Hemophagocytic lymphohistiocytosis[J]. Arch Pathol Lab Med, 2022, 146(4): 507-519. doi: 10.5858/arpa.2020-0802-RA
[5] Henter JI, Horne A, Aricó M, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis[J]. Pediatr Blood Cancer, 2007, 48(2): 124-131. doi: 10.1002/pbc.21039
[6] 中国医师协会血液科医师分会, 中华医学会儿科学分会血液学组, 噬血细胞综合征中国专家联盟, 等. 中国噬血细胞综合征诊断与治疗指南(2022年版)[J]. 中华医学杂志, 2022, 102(20): 1492-1499. doi: 10.3760/cma.j.cn112137-20220310-00488
[7] Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients[J]. Nihon Geka Gakkai Zasshi, 1984, 85(9): 1001-1005.
[8] Yoon SE, Eun Y, Huh K, et al. A comprehensive analysis of adult patients with secondary hemophagocytic lymphohistiocytosis: a prospective cohort study[J]. Ann Hematol, 2020, 99(9): 2095-2104. doi: 10.1007/s00277-020-04083-6
[9] Li X, Yan HP, Zhang XP, et al. Clinical profiles and risk factors of 7-day and 30-day mortality among 160 pediatric patients with hemophagocytic lymphohistiocytosis[J]. Orphanet J Rare Dis, 2020, 15(1): 229. doi: 10.1186/s13023-020-01515-4
[10] Apodaca E, Rodríguez-Rodríguez S, Tuna-Aguilar EJ, et al. Prognostic factors and outcomes in adults with secondary hemophagocytic lymphohistiocytosis: a single-center experience[J]. Clin Lymphoma Myeloma Leuk, 2018, 18(10): e373-e380. doi: 10.1016/j.clml.2018.06.014
[11] Wang YN, Huang WQ, Hu LD, et al. Multicenter study of combination DEP regimen as a salvage therapy for adult refractory hemophagocytic lymphohistiocytosis[J]. Blood, 2015, 126(19): 2186-2192. doi: 10.1182/blood-2015-05-644914
[12] Yoon JH, Park SS, Jeon YW, et al. Treatment outcomes and prognostic factors in adult patients with secondary hemophagocytic lymphohistiocytosis not associated with malignancy[J]. Haematologica, 2019, 104(2): 269-276. doi: 10.3324/haematol.2018.198655
[13] Zhou J, Wu ZQ, Qiao TF. Development of Laboratory Parameters-Based Formulas in Predicting Short Outcomes for Adult Hemophagocytic Lymph-ohistiocytosis Patients with Different Underlying Diseases[J]. J Clin Immunol, 2022, 42(5): 1000-1008. doi: 10.1007/s10875-022-01263-z
[14] Valade S, Mariotte E, Azoulay E. Coagulation disorders in hemophagocytic lymphohistiocytosis/macrophage activation syndrome[J]. Crit Care Clin, 2020, 36(2): 415-426. doi: 10.1016/j.ccc.2019.12.004
[15] 高欣, 仇红霞, 王菊娟, 等. 血清钙离子浓度及白蛋白水平在继发性噬血细胞性淋巴组织细胞增多症中的临床意义[J]. 中华血液学杂志, 2017, 38(12): 1031-1035. doi: 10.3760/cma.j.issn.0253-2727.2017.12.005
[16] Klein GL. The role of calcium in inflammation-associated bone resorption[J]. Biomolecules, 2018, 8(3): 69. doi: 10.3390/biom8030069
[17] Kelly A, Levine MA. Hypocalcemia in the critically ill patient[J]. J Intensive Care Med, 2013, 28(3): 166-177. doi: 10.1177/0885066611411543
[18] Luan CY, Wang F, Wei N, et al. Prognostic nutritional index and the prognosis of diffuse large b-cell lymphoma: a meta-analysis[J]. Cancer Cell Int, 2020, 20(1): 1-8. doi: 10.1186/s12935-019-1086-5
[19] Correa-Rodríguez M, Pocovi-Gerardino G, Callejas-Rubio JL, et al. The prognostic nutritional index and nutritional risk index are associated with disease activity in patients with systemic lupus erythematosus[J]. Nutrients, 2019, 11(3): 638. doi: 10.3390/nu11030638
[20] Kahraman S. Prognostic nutritional index predicts mortality in infective endocarditis[J]. Arch Turk Soc Cardiol, 2020, 48(4): 392-402.
[21] Peters SJ, Vanhaecke T, Papeleu P, et al. Co-culture of primary rat hepatocytes with rat liver epithelial cells enhances interleukin-6-induced acute-phase protein response[J]. Cell Tissue Res, 2010, 340(3): 451-457. doi: 10.1007/s00441-010-0955-y
[22] 董宁, 周军, 谢梦晓, 等. 外周血淋巴细胞计数对成人噬血细胞综合征患者死亡风险的预测价值[J]. 重庆医学, 2022, 51(4): 574-578, 583. https://www.cnki.com.cn/Article/CJFDTOTAL-CQYX202204007.htm
[23] Gratton SM, Powell TR, Theeler BJ, et al. Neurological involvement and characterization in acquired hemophagocytic lymphohistiocytosis in adulthood[J]. J Neurol Sci, 2015, 357(1-2): 136-142. doi: 10.1016/j.jns.2015.07.017
[24] Huang ZZ, Jia YP, Zuo YX, et al. Malignancy-associated hemophagocytic lymphohistiocytosis in children: a 10-year experience of a single pediatric hematology center[J]. Hematology, 2020, 25(1): 389-399. doi: 10.1080/16078454.2020.1833505
[25] Zhao YZ, Zhang Q, Li ZG, et al. Central nervous system involvement in 179 Chinese children with hemophagocytic lymphohistiocytosis[J]. Chin Med J(Engl), 2018, 131(15): 1786-1792.
[26] Blincoe A, Heeg M, Campbell PK, et al. Neuroinflammatory disease as an isolated manifestation of hemophagocytic lymphohistiocytosis[J]. J Clin Immunol, 2020, 40(6): 901-916. doi: 10.1007/s10875-020-00814-6
[27] Benson LA, Li H, Henderson LA, et al. Pediatric CNS-isolated hemophagocytic lymphohistiocytosis[J]. Neurol Neuroimmunol Neuroinflamm, 2019, 6(3): e560. doi: 10.1212/NXI.0000000000000560
-




 下载:
下载: