-
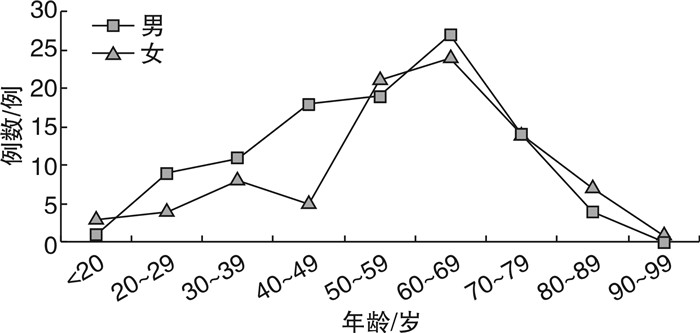
摘要: 目的 了解静脉血栓栓塞症(venous thromboembolism,VTE),包括深静脉血栓形成(deep vein thrombosis,DVT)和肺血栓栓塞症(pulmonary thromboembolism,PTE)的临床资料,为VTE的防治工作提供临床参考。方法 回顾性分析华中科技大学同济医学院附属协和医院血管外科自2021年12月—2023年10月收治的190例VTE住院患者的临床资料。结果 190例VTE患者中男103例,女87例,男女比例为1.18∶1;发病年龄13~90岁,VTE发病率随年龄的增加而上升;排名前3的危险因素分别为肥胖、下肢静脉功能不全和损伤或骨折;170例(98.84%,170/172)下肢DVT患者由下肢静脉超声确诊,65例(100.00%, 65/65)PTE患者由CT肺动脉造影确诊,188例(98.95%, 188/190)VTE患者接受了抗凝治疗。结论 VTE是由多种危险因素导致的,静脉超声和CT肺动脉造影在VTE的诊断中具有重要价值,抗凝治疗是最基础、最广泛应用的VTE治疗方法。Abstract: Objective To understand the clinical data of venous thromboembolism(VTE), including deep vein thrombosis(DVT) and pulmonary thromboembolism(PTE), and provide clinical reference to the prevention and treatment of VTE.Methods The clinical data of 190 VTE inpatients admitted to the Department of Vascular Surgery of Union Hospital from December 2021 to October 2023 were retrospectively analyzed.Results Among 190 VTE patients, there were 103 males and 87 females, with a male to female ratio of 1.18 : 1. The age ranged from 13 to 90 years old and the incidence of VTE increased with age. The top three risk factors were obesity, venous insufficiency of the lower limbs, and injury or fracture. 170(98.84%, 170/172) lower limbs DVT patients were diagnosed by venous ultrasound, 65(100.00%, 65/65) PTE patients were diagnosed by CT pulmonary angiography, and 188(98.95%, 188/190) VTE patients received anticoagulant therapy.Conclusion VTE is caused by a variety of risk factors. Venous ultrasound and CT pulmonary angiography are of great value in the diagnosis of VTE. Anticoagulant therapy is the most basic and widely used treatment for VTE.
-
Key words:
- venous thromboembolism /
- deep vein thrombosis /
- pulmonary thromboembolism
-

-
表 1 VTE住院患者的危险因素
危险因素 例数(%) 肥胖 24(12.63) 下肢静脉功能不全 22(11.58) 损伤/骨折 21(11.05) 手术与制动 20(10.53) VTE病史 18(9.47) 恶性肿瘤、化疗患者 13(6.84) 妊娠/产后 4(2.11) 脑卒中、瘫痪或长期卧床 3(1.58) 抗磷脂抗体 3(1.58) 肾病综合征 2(1.05) 人工血管或血管腔内移植物 2(1.05) -
[1] ISTH Steering Committee for World Thrombosis Day. Thrombosis: a major contributor to the global disease burden[J]. J Thromb Haemost, 2014, 12(10): 1580-1590. doi: 10.1111/jth.12698
[2] Wendelboe AM, Raskob GE. Global burden of thrombosis: epidemiologic aspects[J]. Circ Res, 2016, 118(9): 1340-1347. doi: 10.1161/CIRCRESAHA.115.306841
[3] 《中国血栓性疾病防治指南》专家委员会. 中国血栓性疾病防治指南[J]. 中华医学杂志, 2018, 98(36): 2861-2888. https://www.cnki.com.cn/Article/CJFDTOTAL-LZBJ201903006.htm
[4] Bell WR, Simon TL. Current status of pulmonary thromboembolic disease: pathophysiology, diagnosis, prevention, and treatment[J]. Am Heart J, 1982, 103(2): 239-262. doi: 10.1016/0002-8703(82)90498-7
[5] Knudson MM, Gomez D, Haas B, et al. Three thousand seven hundred thirty-eight posttraumatic pulmonary emboli: a new look at an old disease[J]. Ann Surg, 2011, 254(4): 625-632. doi: 10.1097/SLA.0b013e3182300209
[6] Wenger N, Sebastian T, Engelberger RP, et al. Pulmonary embolism and deep vein thrombosis: Similar but different[J]. Thromb Res, 2021, 206: 88-98. doi: 10.1016/j.thromres.2021.08.015
[7] Lutsey PL, Zakai NA. Epidemiology and prevention of venous thromboembolism[J]. Nat Rev Cardiol, 2023, 20(4): 248-262. doi: 10.1038/s41569-022-00787-6
[8] Chen F, Huang JG, Liu X, et al. Left iliac vein involvement is a protective factor against symptomatic pulmonary embolism in lower left extremity deep vein thrombosis[J]. J Vasc Surg Venous Lymphat Disord, 2022, 10(6): 1272-1278. doi: 10.1016/j.jvsv.2022.05.015
[9] Stein PD, Matta F, Keyes DC, et al. Impact of vena cava filters on in-hospital case fatality rate from pulmonary embolism[J]. Am J Med, 2012, 125(5): 478-484. doi: 10.1016/j.amjmed.2011.05.025
[10] Decousus H, Leizorovicz A, Parent F, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group[J]. N Engl J Med, 1998, 338(7): 409-415. doi: 10.1056/NEJM199802123380701
[11] Kesselman A, Oo TH, Johnson M, et al. Current controversies in inferior vena Cava filter placement: AJR expert panel narrative review[J]. AJR Am J Roentgenol, 2021, 216(3): 563-569. doi: 10.2214/AJR.20.24817
[12] Ahmed O, Sheikh S, Tran P, et al. Inferior vena Cava filter evaluation and management for the diagnostic radiologist: a comprehensive review including inferior vena Cava filter-related complications and PRESERVE trial filters[J]. Can Assoc Radiol J, 2019, 70(4): 367-382. doi: 10.1016/j.carj.2019.06.003
[13] Jia ZZ, Wu A, Tam M, et al. Caval penetration by inferior vena Cava filters: a systematic literature review of clinical significance and management[J]. Circulation, 2015, 132(10): 944-952. doi: 10.1161/CIRCULATIONAHA.115.016468
[14] Dinglasan LAV, Oh JC, Schmitt JE, et al. Complicated inferior vena cava filter retrievals: associated factors identified at preretrieval CT[J]. Radiology, 2013, 266(1): 347-354. doi: 10.1148/radiol.12120372
[15] Sarosiek S, Crowther M, Sloan JM. Indications, complications, and management of inferior vena cava filters: the experience in 952 patients at an academic hospital with a level Ⅰ trauma center[J]. JAMA Intern Med, 2013, 173(7): 513-517. doi: 10.1001/jamainternmed.2013.343
[16] Bikdeli B, Chatterjee S, Desai NR, et al. Inferior vena Cava filters to prevent pulmonary embolism: systematic review and meta-analysis[J]. J Am Coll Cardiol, 2017, 70(13): 1587-1597. doi: 10.1016/j.jacc.2017.07.775
[17] Tsui B, An TZ, Moon E, et al. Retrospective review of 516 implantations of option inferior vena Cava filters at a single health care system[J]. J Vasc Interv Radiol, 2016, 27(3): 345-353. doi: 10.1016/j.jvir.2015.11.055
[18] Young T, Sriram KB. Vena caval filters for the prevention of pulmonary embolism[J]. Cochrane Database Syst Rev, 2020, 10(10): CD006212.
[19] Patel G, Panikkath R, Fenire M, et al. Indications and appropriateness of inferior vena cava filter placement[J]. Am J Med Sci, 2015, 349(3): 212-216. doi: 10.1097/MAJ.0000000000000386
[20] Bikdeli B, Wang Y, Minges KE, et al. Vena caval filter utilization and outcomes in pulmonary embolism: medicare hospitalizations from 1999 to 2010[J]. J Am Coll Cardiol, 2016, 67(9): 1027-1035. doi: 10.1016/j.jacc.2015.12.028
[21] 中国医师协会介入医师分会, 中华医学会放射学分会介入专业委员会, 中国静脉介入联盟. 下腔静脉滤器置入术和取出术规范的专家共识(第2版)[J]. 中华医学杂志, 2020, 100(27): 2092-2101.
-

| 引用本文: | 崔藏月, 王宏飞, 唐亮, 等. 190例静脉血栓栓塞症住院患者临床资料分析[J]. 临床血液学杂志, 2024, 37(7): 474-476. doi: 10.13201/j.issn.1004-2806.2024.07.007 |
| Citation: | CUI Cangyue, WANG Hongfei, TANG Liang, et al. Clinical data analyses of 190 hospitalized patients with venous thromboembolism[J]. J Clin Hematol, 2024, 37(7): 474-476. doi: 10.13201/j.issn.1004-2806.2024.07.007 |
- Figure 1.



 下载:
下载: