Study on relationship between serum gastrin-17 and platinum resistance recurrence after platinum chemotherapy in ovarian cancer
-
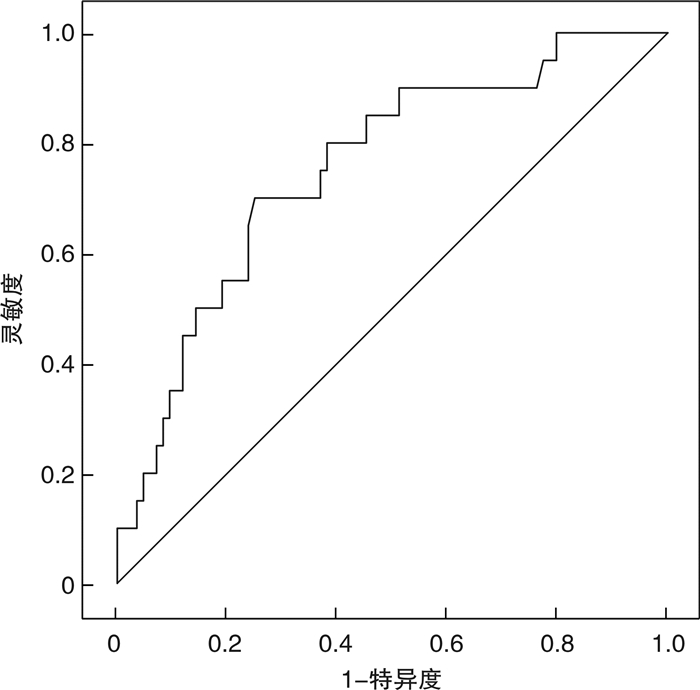
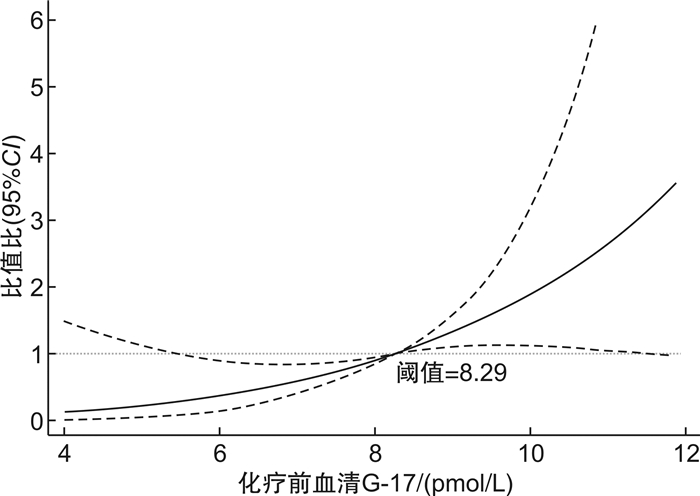
摘要: 目的 探讨血清胃泌素-17(G-17)与卵巢癌铂类药物化疗后铂耐药复发的关系。方法 回顾性收集医院2017年1月至2023年6月收治的104例卵巢癌铂类药物化疗后复发的患者资料,根据复发类型分为铂耐药复发组(20例)与铂敏感复发组(84例)。比较2组患者临床资料及入院时血清G-17水平,重点分析血清G-17与卵巢癌铂类药物化疗后铂耐药复发的关系。结果 2组患者年龄、病理分级等一般资料比较,差异无统计学意义(P>0.05);铂耐药复发组国际妇产科联盟(FIGO)分期Ⅲ~Ⅳ期患者占比、Fagotti评分、人附睾蛋白4(HE4)水平均高于铂敏感复发组(P < 0.05);铂耐药复发组化疗前及化疗后血清G-17水平均高于铂敏感复发组(P < 0.05);经多因素logistic回归分析显示,Fagotti评分、HE4、化疗前及化疗后血清G-17与卵巢癌铂类药物化疗后铂耐药复发有关(P < 0.05);经限制性立方样条模型分析显示,化疗前血清G-17水平与卵巢癌铂类药物化疗后铂耐药复发的关联呈非线性曲线型剂量反应关系(P < 0.05),当化疗前血清G-17>8.29 pmol/L时,患者铂耐药复发风险随指标水平升高而增加;以化疗前血清G-17水平为预测指标,绘制受试者工作特征曲线,结果显示,卵巢癌患者化疗前血清G-17预测卵巢癌铂类药物化疗后铂耐药复发的曲线下面积为0.755(95%CI 0.640~0.870),灵敏度、特异度分别为70.0%、75.0%。结论 卵巢癌患者铂类药物化疗后铂耐药复发可能与化疗前血清G-17水平异常表达有关,血清G-17水平异常升高或提示患者铂耐药复发高风险,对铂耐药复发有一定预测价值。Abstract: Objective To explore the relationship between serum gastrin-17(G-17) and platinum resistance recurrence in ovarian cancer after platinum based chemotherapy.Methods A retrospective collection of data was conducted on 104 patients with recurrent ovarian cancer after platinum chemotherapy treated at Hospital from January 2017 to June 2023. According to the type of recurrence, they were divided into platinum resistant recurrence group(20 cases) and platinum sensitive recurrence group(84 cases). The clinical data and serum G-17 level at admission were compared between the two groups, and the relationship between serum G-17 and the recurrence of platinum-resistant ovarian cancer after platinum chemotherapy was analyzed.Results There was no statistical significant difference in general information such as age and pathological grade between the two groups(P>0.05). The proportion of International Federation of Gynecology and Obstetrics(FIGO) stage Ⅲ-Ⅳ patients, Fagotti score, and human epididymal protein 4(HE4) levels in the platinum resistant recurrence group were higher than those in the platinum sensitive recurrence group(P < 0.05). The serum G-17 levels in the platinum resistant recurrence group before and after chemotherapy were higher than those in the platinum sensitive recurrence group(P < 0.05). Multiple logistic regression analysis showed that Fagotti score, HE4, serum G-17 levels before and after chemotherapy were associated with platinum resistance recurrence in ovarian cancer after platinum based chemotherapy(P < 0.05). According to the Restricted Cubic Spline Model analysis, there was a non-linear dose-response relationship between pre chemotherapy serum G-17 levels and platinum resistance recurrence in ovarian cancer after platinum drug chemotherapy(P < 0.05). When pre chemotherapy serum G-17>8.29 pmol/L, the risk of platinum resistance recurrence in patients increased with the increase of indicator levels. Pre chemotherapy serum G-17 levels were used as a predictive indicator, a receiver operating characteristic curve was plotted. The results showed that the area under the curve of pre chemotherapy serum G-17 in ovarian cancer patients predicting platinum resistance recurrence after platinum chemotherapy was 0.755(95%CI 0.640-0.870), with sensitivity and specificity of 70.0% and 75.0%, respectively.Conclusion The recurrence of platinum resistance in ovarian cancer patients after platinum based chemotherapy may be related to abnormal expression of serum G-17 levels before chemotherapy. Abnormal elevation of serum G-17 levels may indicate a high risk of platinum resistance recurrence in patients, and have certain predictive value for platinum resistance recurrence.
-
Key words:
- ovarian cancer /
- chemotherapy /
- platinum resistance /
- recurrence /
- serum gastrin-17
-

-
表 1 不同复发类型患者临床资料比较
组别 铂耐药复发组(n=20) 铂敏感复发组(n=84) t/χ2 P 年龄/岁 57.65±4.85 56.86±5.00 0.639 0.525 既往史/例(%) 糖尿病 9(45.00) 32(38.10) 0.322 0.570 高血压 13(65.00) 51(60.71) 0.125 0.723 FIGO分期/例(%) 5.349 0.021 Ⅰ~Ⅱ期 9(45.00) 57(67.86) Ⅲ~Ⅳ期 11(55.00) 27(32.14) 病理类型/例(%) 3.499 0.167 浆液性卵巢癌 17(85.00) 80(95.24) 黏液性卵巢癌 2(10.00) 2(2.38) 透明细胞癌 1(5.00) 2(2.38) 病理分级/例(%) 1.162 0.281 高级别 14(70.00) 68(80.95) 低级别 6(30.00) 16(19.05) Fagotti评分/分 6.00(6.00,6.00) 4.00(4.00,6.00) 3.001 0.003 CA125/(U/mL) 470.39±186.12 462.48±179.05 0.176 0.860 CA199/(U/mL) 134.64±13.19 130.14±15.25 1.215 0.227 HE4/(pmol/L) 416.29±81.77 348.83±79.98 3.376 0.001 表 2 不同复发类型患者血清G-17比较
pmol/L,X±S 组别 例数 化疗前 化疗后 t P 铂耐药复发组 20 9.24±2.36 13.34±2.58 5.030 < 0.001 铂敏感复发组 84 7.01±2.28 11.85±3.01 10.489 < 0.001 t 3.912 2.025 P < 0.001 0.046 表 3 变量赋值情况
变量 赋值 因变量 复发类型 铂耐药复发=1,铂敏感复发=0 化疗前血清G-17 实测值 化疗后血清G-17 实测值 自变量 FIGO分期 Ⅲ~Ⅳ期=1,Ⅰ~Ⅱ期=0 Fagotti评分 实测值 HE4 实测值 表 4 卵巢癌铂类药物化疗后铂耐药复发与主要指标关系的回归分析
项目 B SE Wald P OR 95%CI FIGO分期 0.888 0.659 1.816 0.178 2.430 0.668~8.839 Fagotti评分 0.451 0.217 4.343 0.037 1.570 1.027~2.401 HE4 0.012 0.005 5.955 0.015 1.012 1.002~1.021 化疗前血清G-17 0.451 0.157 8.297 0.004 1.571 1.155~2.135 化疗后血清G-17 0.297 0.121 6.001 0.014 1.346 1.061~1.708 常量 -17.051 3.903 19.085 < 0.001 - - -
[1] 王雅菲, 王健, 刘军华. 肿瘤细胞减灭术后行腹腔热灌注5-FU+卡铂化疗联合静脉化疗治疗晚期卵巢癌的效果观察[J]. 中国妇产科临床杂志, 2022, 23(5): 452-454. doi: 10.13390/j.issn.1672-1861.2022.05.002
[2] 马建新, 严丽花, 甘志忠, 等. 卵巢癌患者NSE、CYFRA21-1、Fer表达及与淋巴结转移的关系分析[J]. 临床血液学杂志, 2023, 36(2): 98-103. doi: 10.13201/j.issn.1004-2806.2023.02.005
[3] Kus F, Guven DC, Yildirim HC, et al. KELIM score predicts outcome in patients with platinum-resistant/refractory recurrent ovarian cancer[J]. Biomark Med, 2023, 17(7): 379-389. doi: 10.2217/bmm-2022-0923
[4] 王涛, 宋飞雪. 铂耐药卵巢癌的免疫治疗进展[J]. 实用医学杂志, 2021, 37(20): 2575-2579.
[5] Li YJ, Zhao Y, Li Y, et al. Gastrin-17 induces gastric cancer cell epithelial-mesenchymal transition via the Wnt/β-catenin signaling pathway[J]. J Physiol Biochem, 2021, 77(1): 93-104. doi: 10.1007/s13105-020-00780-y
[6] 李梅, 许佳, 刘玉萍. 血清胃蛋白酶原、胃泌素-17及幽门螺杆菌检测在健康体检人群胃癌筛查中的应用价值[J]. 现代肿瘤医学, 2023, 31(16): 3041-3045. doi: 10.3969/j.issn.1672-4992.2023.16.018
[7] Gašenko E, Bogdanova I, Sjomina O, et al. Assessing the utility of pepsinogens and gastrin-17 in gastric cancer detection[J]. Eur J Cancer Prev, 2023, 32(5): 478-484. doi: 10.1097/CEJ.0000000000000791
[8] 中国抗癌协会妇科肿瘤专业委员会. 卵巢恶性肿瘤诊断与治疗指南(2021年版)[J]. 中国癌症杂志, 2021, 31(6): 490-500.
[9] 中国抗癌协会妇科肿瘤专业委员会. 阴道恶性肿瘤诊断与治疗指南(第四版)[J]. 中国实用妇科与产科杂志, 2018, 34(11): 1227-1229. doi: 10.19538/j.fk2018110111
[10] 林仲秋. FIGO/IGCS妇科恶性肿瘤分期及临床实践指南(六): 卵巢癌[J]. 国际妇产科学杂志, 2008, 35(6): 459-461.
[11] Fagotti A, Ferrandina G, Fanfani F, et al. A laparoscopy-based score to predict surgical outcome in patients with advanced ovarian carcinoma: a pilot study[J]. Ann Surg Oncol, 2006, 13(8): 1156-1161.
[12] 牛星燕, 张冬萍, 彭芸花. 卵巢癌铂耐药机制及相关靶向治疗研究进展[J]. 中国妇产科临床杂志, 2020, 21(6): 661-663.
[13] 蒋琴, 徐杰, 严科. 卵巢癌铂耐药复发相关临床因素研究[J]. 中国临床医生杂志, 2021, 49(11): 1287-1290.
[14] Zhang CY, Xu C, Gao XY, et al. Platinum-based drugs for cancer therapy and anti-tumor strategies[J]. Theranostics, 2022, 12(5): 2115-2132.
[15] 陈霁晖, 顾芬芬, 李超, 等. ABC跨膜转运蛋白基因表达与乳腺癌铂类药物灵敏度的相关性研究[J]. 药学与临床研究, 2019, 27(2): 93-97.
[16] 陈树添, 黄泽洧, 林明河, 等. PGR、G-17、miR-27b-3p对慢性胃炎患者预后不良和癌变的预测价值[J]. 山东医药, 2022, 62(25): 73-76.
[17] Zeng JC, Shen Y, Xu SP, et al. Analysis of gastrin-17 and its related influencing factors in physical examination results[J]. Immun Inflamm Dis, 2023, 11(10): e993.
[18] 胡维林, 邓元河, 尹小兵, 等. 血清PGⅠ、PGⅡ及胃泌素17水平的变化与老年胃癌患病的关系分析[J]. 中国实验诊断学, 2021, 25(11): 1649-1652. doi: 10.3969/j.issn.1007-4287.2021.11.017
[19] Liu WJ, Sun YX, Yuan YL. Analysis of serum gastrin-17 and Helicobacter pylori antibody in healthy Chinese population[J]. J Clin Lab Anal, 2020, 34(12): e23518.
[20] 蒋东葵, 陈兆亚, 马冬梅, 等. 血清胃泌素释放肽前体、甲胎蛋白和糖类抗原199单项及联合检测在卵巢癌诊断中的价值[J]. 诊断学理论与实践, 2019, 18(2): 209-214.
[21] 梁永琴, 赵宏伟. 卵巢上皮性癌铂耐药复发影响因素分析[J]. 肿瘤研究与临床, 2022, 34(10): 783-785. doi: 10.3760/cma.j.cn115355-20220416-00234
[22] 徐翔, 刘慧, 周红辉, 等. 高级别浆液性卵巢癌铂类耐药的相关因素分析[J]. 解放军医学院学报, 2019, 40(12): 1118-1121. doi: 10.3969/j.issn.2095-5227.2019.12.003
[23] 胡丽花, 袁明, 赵嫦娥, 等. 上皮性卵巢癌患者血清CA125、IGF1、Annexin A3、HE4与卡铂耐药和预后的关系研究[J]. 现代生物医学进展, 2022, 22(18): 3494-3498.
[24] 卢洁芳, 陈迪文, 应夏青. 上皮性卵巢癌患者血清上皮型钙黏蛋白、人附睾蛋白4水平表达及与术后复发的关系[J]. 中国卫生检验杂志, 2022, 32(23): 2904-2907.
-




 下载:
下载: