Effect and correlation of LDL/HDL and apoB/apoA1 on lupus nephritis with different degrees of renal injury
-
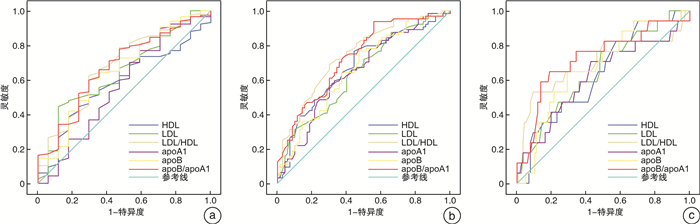
摘要: 目的 分析低密度脂蛋白/高密度脂蛋白比值(LDL/HDL)、载脂蛋白B/载脂蛋白A1比值(apoB/apoA1)对不同程度肾损伤狼疮肾炎(LN)的影响与相关性。方法 回顾性分析我院诊断和治疗的LN患者134例,根据肾小球滤过率(e-GFR)将患者分为肾功能不全组和肾功能正常组,通过单因素和多因素分析LDL/HDL、apoB/apoA1对肾功能不全LN的影响,通过多重线性回归和相关性分析探讨LDL/HDL、apoB/apoA1与不同e-GFR水平的关系与相关性。结果 单因素和二元logistic回归分析发现病程、LDL/HDL、apoB/apoA1、C3、抗-dsDNA阳性、SLEDAI均为LN的影响因素,OR值分别为1.084、5.669、31.738、0.490、3.427、1.351(均P < 0.05)。纠正混杂因素前后LDL/HDL、apoB/apoA1始终为e-GFR < 90 mL/min/1.73 m2、e-GFR < 60 mL/min/1.73 m2、e-GFR < 30 mL/min/1.73 m2的风险因素。LDL/HDL、apoB/apoA1均与不同分期e-GFR降低存在关联,其关联作用由强至弱分别为肾损伤3期、2期、4~5期、1期。Pearson相关型分析显示,LDL/HDL、apoB/apoA1均与不同肾损伤分期患者e-GFR呈负相关,在肾损伤1期、2期、3期相关性持续增强,在4~5期稍弱,呈“V”型变化趋势。LDL/HDL、apoB/apoA1e评估LN患者e-GFR < 90 mL/min/1.73 m2、e-GFR < 60 mL/min/1.73 m2、e-GFR < 30 mL/min/1.73 m2曲线下面积(AUC)分别为0.679、0.744、0.700、0.673、0.730、0.711,均高于LDL、HDL、apoB、apoA1(P < 0.05)。结论 LDL/HDL、apoB/apoA1均为LN肾损伤的风险因素,且在不同肾损伤阶段,LDL/HDL、apoB/apoA1与不同阶段肾损伤e-GFR下降关联性不同。Abstract: Objective To analyze the effects and correlations of low-density lipoprotein to high-density lipoprotein ratio(LDL/HDL) and apolipoprotein B to apolipoprotein A1 ratio(apoB/apoA1) on lupus nephritis(LN) with different degrees of renal injury.Methods A retrospective analysis was conducted on 134 LN patients diagnosed and treated in our hospital. Patients were divided into renal insufficiency group and normal renal function group based on glomerular filtration rate(e-GFR). The effects of LDL/HDL, apoB/apoA1 on renal insufficiency LN were analyzed by univariate and multivariate methods. The relationship and correlation between LDL/HDL, apoB/apoA1, and different e-GFR levels were explored through multiple linear regression and correlation analysis.Results Univariate and binary logistic regression analysis showed that disease course, LDL/HDL, apoB/apoA1, C3, anti-dsDNA positive, and SLEDAI were all influencing factors of LN, the OR values were 1.084, 5.669, 31.738, 0.490, 3.427 and 1.351, respectively(all P < 0.05). Before and after correcting for confounding factors, LDL/HDL and apoB/apoA1 were still risk factors for e-GFR < 90 mL/min/1.73 m2, e-GFR < 60 mL/min/1.73 m2 and e-GFR < 30 mL/min/1.73 m2. LDL/HDL, apoB/apoA1 were associated with a decrease in e-GFR at different stages, and the correlation from strong to weak were from stages 3, 2, 4-5 and 1. Pearson correlation analysis showed that LDL/HDL and apoB/apoA1 were negatively correlated with e-GFR in patients with different stages of kidney injury. The correlation continued to increase in stages 1, 2, and 3 of kidney injury, and slightly weakened in stages 4-5, showing a V-shaped trend. LDL/HDL and apoB/apoA1e assessed the area under the curve(AUC) of LN patients with e-GFR < 90 mL/min/1.73 m2, e-GFR < 60 mL/min/1.73 m2, and e-GFR < 30 mL/min/1.73 m2 were 0.679, 0.744, 0.700, 0.673, 0.730 and 0.711, respectively, and the AUC were higher than LDL, HDL, apoB and apoA1(P < 0.05).Conclusion LDL/HDL, apoB/apoA1 might be risk factors for LN renal injury, and the correlation between LDL/HDL, apoB/apoA1, and e-GFR reduction in renal injury varies at different stages of renal injury were different.
-

-
表 1 LN肾功能不全单因素分析
变量 单因素分析 U/t/χ2 P 肾功能不全组(n=63) 肾功能正常组(n=71) 年龄/岁 38.74±7.33 37.85±6.98 0.720 0.473 性别(男/女)/例 10/53 8/63 0.609 0.435 病程/月 34.51±8.72 30.62±7.54 2.769 0.007 TG/(mmol /L) 2.54±0.92 2.29±0.96 1.534 0.127 TC/(mmol /L) 5.03(4.16,6.75) 4.92(3.98,6.48) 1.538 0.127 LDL/(mmol /L) 2.80(2.02,3.58) 2.57(1.87,3.48) 2.195 0.029 HDL/(mmol /L) 1.35(0.61,1.62) 1.52(0.65,1.70) 2.025 0.046 LDL/HDL 2.78(2.12,3.24) 2.54(1.86,2.89) 2.860 0 apoB/(g/L) 1.32(0.72,1.73) 1.14(0.64,1.63) 2.342 0.020 apoA1/(g/L) 1.04(0.63,1.47) 1.31(0.78,1.71) 2.781 0.006 apoB/apoA1 1.32(0.84,1.83) 0.91(0.54,1.44) 3.120 0 C4/(g/L) 0.14(0.09,0.27) 0.17(0.11,0.26) 1.406 0.163 C3/(g/L) 0.52(0.33,0.79) 0.73(0.57,1.10) 2.531 0.013 抗-Sm阳性/例(%) 35(51.16) 30(42.25) 2.365 0.124 抗-ANA阳性/例(%) 63(100.00) 71(100.00) 0 1.000 抗-dsDNA阳性/例(%) 44(79.07) 31(37.29) 9.283 0.002 抗-SSA阳性/例(%) 23(44.19) 20(39.22) 1.065 0.302 抗-SSB阳性/例(%) 15(27.91) 12(19.61) 0.990 0.320 抗U1-snRNP阳性/例(%) 32(50.79) 29(40.85) 1.332 0.248 SLEDAI 15(9,22) 12(6,20) 2.314 0.028 表 2 LN肾功能不全的多因素分析
变量 β SE Wald P OR 95%CI 下限 上限 病程 0.080 0.022 12.772 0 1.084 1.037 1.132 LDL/HDL 1.735 0.657 6.984 0.008 5.669 1.566 20.528 apoB/apoA1 3.458 1.136 9.270 0.002 31.738 3.428 293.885 C3 -3.014 1.368 4.854 0.028 0.490 0.003 0.717 抗-dsDNA阳性 1.232 0.591 4.343 0.037 3.427 1.076 10.916 SLEDAI 0.301 0.067 20.469 0 1.351 1.186 1.539 常量 -14.175 3.174 19.942 0 0 表 3 血脂项目对不同程度肾损伤LN的影响
OR(95%CI) 血脂 e-GFR < 90 mL/min/1.73 m2 e-GFR < 60 mL/min/1.73 m2 e-GFR < 30 mL/min/1.73 m2 模型1 模型2 模型1 模型2 模型1 模型2 LDL 6.14
(0.85,43.71)5.02
(0.79,45.17)4.62
(1.41,40.26)1)5.33
(2.26,39.17)1)4.23
(0.92,41.23)3.47
(0.89,42.47)HDL 0.84
(0.47,1.41)0.73
(0.48,1.21)0.75
(0.23,0.89)1)0.74
(0.22,0.85)1)0.81
(0.54,1.42)0.76
(0.52,1.32)LDL/HDL 5.62
(1.09,18.62)1)6.24
(2.41,18.52)1)6.75
(1.01,22.84)1)6.98
(1.16,17.59)1)5.78
(2.27,22.62)1)6.47
(3.14,22.62)1)apoB 22.56
(0.93,43.65)20.17
(0.91,41.11)23.17
(2.14,45.32)1)22.75
(2.85,43.62)1)20.16
(0.96,39.66)18.69
(0.89,41.33)apoA1 0.74
(0.46,1.23)0.72
(0.49,1.18)0.68
(0.32,0.89)1)0.65
(0.29,0.82)1)0.78
(0.47,1.25)0.81
(0.50,1.33)apoB/apoA1 21.14
(2.56,52.47)1)20.19
(2.47,50.36)1)26.17
(2.98,42.17)1)29.67
(3.52,47.67)1)22.35
(1.14,46.62)1)24.62
(1.07,47.26)1)注:1)P < 0.05;模型1为未纠正混杂因素二元logistic回归分析;模型2为纠正混杂因素后二元logistic回归分析。 表 4 LDL/HDL、apoB/apoA1与肾损伤分期患者e-GFR的关系
β(95%CI) 血脂 CKD 1期 CKD 2期 CKD 3期 CKD 4~5期 LDL 模型1 -0.36(-1.13,0.41) -2.52(-4.97,-0.08)1) -2.85(-4.89,-0.81)1) -2.42(-4.22,-0.62)1) 模型2 -0.66(-1.55,0.23)1) -3.12(-5.49,-0.75)1) -3.21(-5.45,-0.97)1) -2.19(-3.86,-0.52)1) HDL 模型1 0.44(-0.07,0.95) 1.58(0.07,3.09)1) 1.62(0.14,3.10)1) 1.23(-0.16,2.82) 模型2 0.64(-0.12,1.41) 1.47(-0.11,3.06) 1.68(0.18,3.18)1) 0.98(-0.42,2.38) LDL/HDL 模型1 -1.21(-2.29,-0.13)1) -3.93(-7.75,-0.11)1) -5.03(-9.05,-1.01)1) -2.67(-4.36,-0.98)1) 模型2 -1.26(-2.35,-0.17)1) -3.98(-7.85,-0.11)1) -4.93(-8.91,-0.95)1) -2.59(-4.36,-0.82)1) apoB 模型1 -1.46(-3.04,0.12) -3.73(-7.24,-0.22)1) -3.52(6.19,-0.85)1) -3.17(-5.32,-1.02)1) 模型2 -1.32(-3.59,0.95) -3.47(-6.80,-0.14)1) -3.42(6.47,-0.37)1) -2.98(-5.02,-0.94)1) apoA1 模型1 0.68(-0.23,1.59) 1.33(0.14,2.52)1) 1.67(0.24,3.10)1) 1.04(2.27,-0.19) 模型2 0.85(-0.12,1.82) 1.25(-0.10,2.60) 1.58(0.13,3.03)1) 1.13(2.49,-0.23) apoB/apoA1 模型1 -2.32(-3.79,-0.85)1) -4.02(-7.01,-1.03)1) -4.62(-8.01,-1.24)1) -4.11(-7.48,-0.75)1) 模型2 -2.14(-3.59,-0.69)1) -3.95(-7.02,-0.89)1) -4.24(-7.39,-1.09)1) -3.82(-6.98,-0.66)1) 注:1)P < 0.05;模型1为未纠正混杂因素前的线性回归分析;模型2为纠正混杂因素后的多重线性回归分析。 -
[1] Itotagawa E, Tomofuji Y, Kato Y, et al. SLE stratification based on BAFF and IFN-I bioactivity for biologics and implications of BAFF produced by glomeruli in lupus nephritis[J]. Rheumatology, 2023, 62(5): 1988-1997. doi: 10.1093/rheumatology/keac528
[2] 郭大燕, 肖卫国. 系统性红斑狼疮中血脂异常相关因素分析[J]. 中华风湿病学杂志, 2019, 23(6): 428-432.
[3] Huang SS, Zhang ZY, Cui YY, et al. Dyslipidemia is associated with inflammation and organ involvement in systemic lupus erythematosus[J]. Clin Rheumatol, 2023, 42(6): 1565-1572. doi: 10.1007/s10067-023-06539-2
[4] 胡宏图, 丁国华, 陈星华. 血脂异常与狼疮性肾炎病情活动的相关性[J]. 临床肾脏病杂志, 2021, 21(6): 441-446.
[5] 邓心悦, 蒋磊英, 沈爱玲. 同型半胱氨酸、载脂蛋白B/载脂蛋白A比值及尿微量白蛋白/肌酐比值的变化与高血压早期肾损伤的关系研究[J]. 河北医药, 2022, 44(16): 2473-2476.
[6] Petri M, Orbai AM, Alarcón GS, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus[J]. Arthritis Rheum, 2012, 64(8): 2677-2686. doi: 10.1002/art.34473
[7] 王雨晨, 叶楠, 卞维静, 等. 不同心力衰竭类型对肾功能不全合并心力衰竭患者肾脏远期预后的影响[J]. 中华肾脏病杂志, 2023, 9(1): 1-7.
[8] Kidney Disease: Improving Global Outcomes Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases[J]. Kidney Int, 2021, 100(4S): S1-S276.
[9] Tao CY, Shang J, Chen T, et al. Impact of antimalarial(AM)on serum lipids in systemic lupus erythematosus(SLE)patients: a systematic review and meta-analysis[J]. Medicine, 2019, 98(14): e15030. doi: 10.1097/MD.0000000000015030
[10] Zhai Q, Dou JT, Wen J, et al. Association between changes in lipid indexes and early progression of kidney dysfunction in participants with normal estimated glomerular filtration rate: a prospective cohort study[J]. Endocrine, 2022, 76(2): 312-323. doi: 10.1007/s12020-022-03012-z
[11] Urrestarazú A, Otatti G, Silvariño R, et al. Lupus nephritis in males: clinical features, course, and prognostic factors for end-stage renal disease[J]. Kidney Int Rep, 2017, 2(5): 905-912. doi: 10.1016/j.ekir.2017.05.011
[12] Ruan XZ, Varghese Z, Moorhead JF. An update on the lipid nephrotoxicity hypothesis[J]. Nat Rev Nephrol, 2009, 5(12): 713-721. doi: 10.1038/nrneph.2009.184
[13] Wang XC, Wang HY, Li JS, et al. Combined effects of dyslipidemia and high adiposity on the estimated glomerular filtration rate in a middle-aged Chinese population[J]. Diabetes Metab Syndr Obes, 2021, 14: 4513-4522. doi: 10.2147/DMSO.S337190
[14] Wang YN, Qiu XL, Lv LS, et al. Correlation between serum lipid levels and measured glomerular filtration rate in Chinese patients with chronic kidney disease[J]. PLoS One, 2016, 11(10): e0163767. doi: 10.1371/journal.pone.0163767
[15] Opazo-Ríos L, Mas S, Marín-Royo G, et al. Lipotoxicity and diabetic nephropathy: novel mechanistic insights and therapeutic opportunities[J]. Int J Mol Sci, 2020, 21(7): 2632.
[16] 陈靖珊, 李黎, 赏石丽, 等. IgA肾病病理特征与血脂异常的相关性分析[J]. 昆明医科大学学报, 2023, 44(1): 47-53.
[17] Liu JJ, Song WQ, Cui DW. Relationship between blood lipid profiles and risk of lupus nephritis in children[J]. Int J Clin Pract, 2022, 2022: 6130774.
[18] Saland JM, Kupferman JC, Pierce CB, et al. Change in dyslipidemia with declining glomerular filtration rate and increasing proteinuria in children with CKD[J]. Clin J Am Soc Nephrol, 2019, 14(12): 1711-1718.
[19] 邹艺, 高强, 贺锋. 载脂蛋白B/载脂蛋白A1对脑出血预后预测价值的研究[J]. 临床血液学杂志, 2023, 36(4): 239-244, 248. doi: 10.13201/j.issn.1004-2806.2023.04.004
[20] 李子胜, 赵伟, 冯志刚, 等. apoB/apoA1对系统性红斑狼疮活动性和预后不良预测价值的研究[J]. 临床血液学杂志, 2023, 36(10): 716-722. doi: 10.13201/j.issn.1004-2806.2023.10.006
[21] Xu JL, Zhang HM, Che N, et al. FAR in systemic lupus erythematosus: a potential biomarker of disease activity and lupus nephritis[J]. Clin Exp Med, 2023, 23(8): 4779-4785.
[22] Zhao L, Zhang Q, Feng ZG, et al. Serum amyloid A-to-albumin ratio as a potential biomarker to predict the activity, severity, and poor prognosis of systemic lupus erythematosus[J]. J Clin Lab Anal, 2022, 36(3): e24282.
[23] 白玉兰. 血脂与肾小球滤过率的关联研究: 横断面研究和孟德尔随机化研究[D]. 南宁: 广西医科大学, 2021.
[24] 刘剑, 余戈平, 俞夏莲, 等. 血尿酸水平的变化对肾小球滤过率的影响[J]. 中国中西医结合肾病杂志, 2023, 24(10): 871-875, 942.
[25] 颜卫红, 侯兴华, 李彦勋. apoB/apoA1对系统性红斑狼疮活动性预测价值的研究[J]. 中国处方药, 2023, 21(7): 172-175.
-





 下载:
下载: