Construction and validation of a risk prediction model for PDAP caused by gram-negative or gram-positive bacteria
-
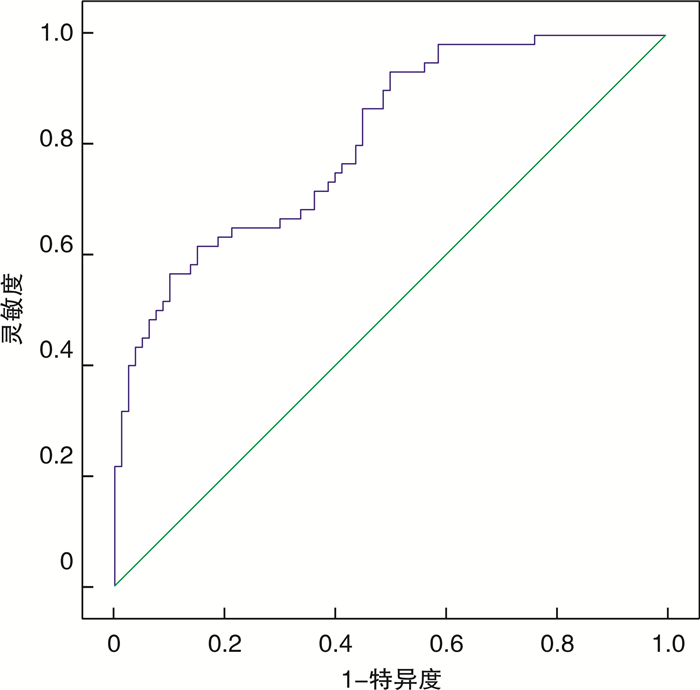
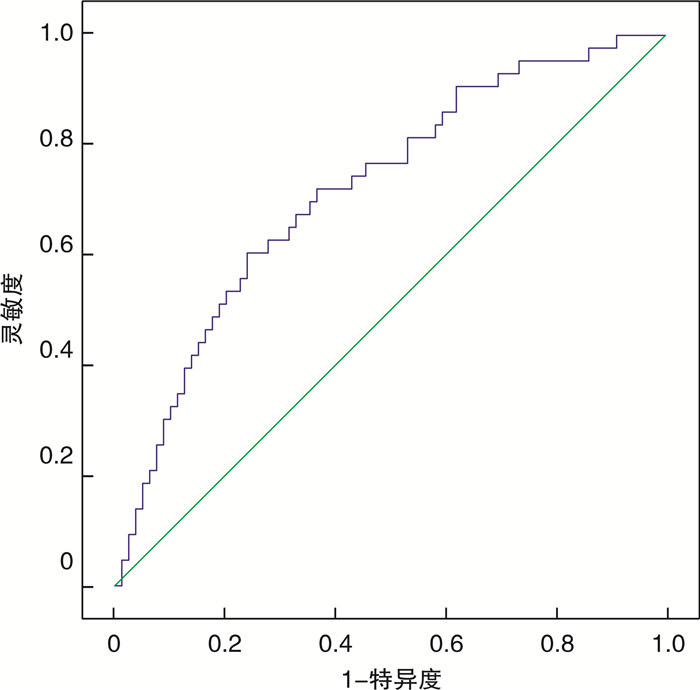
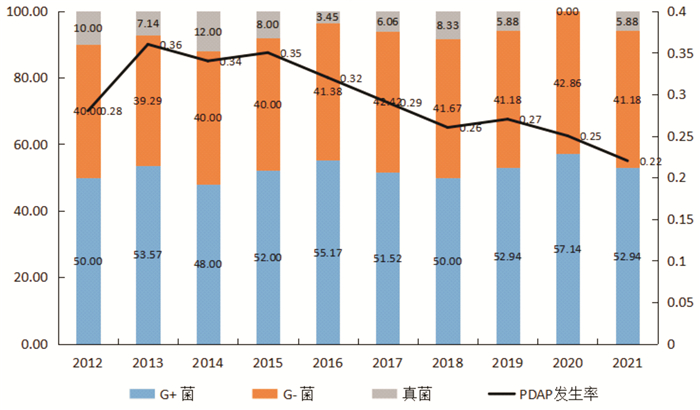
摘要: 目的 了解腹膜透析相关性腹膜炎(peritoneal dialysis associated peritonitis,PDAP)病原菌特征,构建并验证革兰氏阳性(G+)菌或革兰氏阴性(G-)菌引起PDAP风险预测模型。方法 收集2012—2021年发生PDAP的临床资料,分析病原菌特征,根据病原菌革兰氏染色结果分为G+菌和G-菌感染,分别按7︰3的比例随机纳入建模组和验证组,通过二元logistic回归分析确认G-菌引起PDAP影响因素后构建预测模型,并分别在建模组、验证组对模型预测效能进行评估。结果 325例次PDAP患者共检出病原菌232株,其中G+菌121株(52.16%),G-菌95株(40.95%),真菌16株(6.90%)。PDAP患者平均发病率为0.29次/年,自2013年开始,发病率呈下降趋势。建模组(包含G+菌80例次,G-菌60例次)证实腹痛、年龄、中性粒细胞/淋巴细胞比值(NLR)、降钙素原(PCT)均为G-菌性PDAP的影响因素,而血钾(K+)则为保护因素,OR值分别为3.729、1.128、3.968、6.618、0.502。构建G-菌性PDAP预测模型:P=1/{1+EXP[-(-16.605+1.316×腹痛+0.112×年龄+1.378×NLR-2.304×K++1.859×PCT)]}。预测模型对建模组曲线下面积(AUC)为0.793(0.716~0.853),当最佳截断值为0.534时,模型预测灵敏度为76.67%,特异度为75.00%,Hosmer-Lemeshow(H-L)检验结果为P=0.632。预测模型对验证组(包含G+菌34例次,G-菌26例次)AUC为0.759(0.704~0.823),当选择0.534作为截断值时,模型在验证组预测灵敏度为73.08%,特异度为64.71%。K折交叉验证显示,10组训练准确性为0.778±0.032,预测准确性为0.793±0.047。结论 PDAP病原菌以G+为主,发病率呈降低趋势,构建的风险预测模型可以较好地区分G-菌或G+菌性的PDAP。
-
关键词:
- 腹膜透析相关性腹膜炎 /
- 革兰氏阴性菌 /
- 革兰氏阳性菌 /
- 影响因素 /
- 预测模型
Abstract: Objective To analyzed the pathogenic characteristics of peritoneal dialysis associated peritonitis(PDAP), and construct and validate the risk prediction model of gram positive or negative bacteria in PDAP.Methods The clinical data of PDAP and characteristics of pathogenic bacteria the in our hospital from 2012 to 2021 were collected and analyzed, all of them were divided into gram-negative(G-) and gram-positive(G+) bacteria groups according to the results of gram staining of pathogenic bacteria. All patients were randomly divided into the modeling and the validation groups at a ratio of 7︰3 respectively. The prediction model for PDAP caused by gram-negative or gram-positive bacteria were established according to the results of the binary logistic regression analysis and the prediction efficiency of the model were tested both in the modeling and validation groups respectively.Results A total of 232 strains of pathogenic bacteria were detected in 325 cases of PDAP, including 121 strains of G+bacteria(52.16%), 95 strains of G-bacteria(40.95%) and 16 strains of fungi(6.90%). The average incidence rate of PDAP was 0.29 times /patient year, and the incidence rate showed a downward trend from 2013. The modeling group(including 80 cases of G+bacteria and 60 cases of G-bacteria) confirmed that abdominal pain, age, NLR and PCT were the influencing factors of PDAP cased by G-bacteria, while K+was the protective factor, and the OR values were 3.729, 1.128, 3.968, 6.618 and 0.502 respectively. The prediction model of G-bacterial PDAP: P=1/{1+EXP[-(-16.605+1.316×abdominal pain +0.112×age+1.378×NLR-2.304×K++ 1.859×PCT)]}. The area under the curve(AUC), optimal cut-off value, prediction sensitivity and specificity of the prediction model for the modeling group were 0.793(0.716-0.853), 0.534, 76.67% and 75.00% respectively, and the result of the Hosmer Lemeshow(H-L) test was P=0.632. The AUC of the prediction model in the validation group(including 34 cases of G+bacteria and 26 cases of G-bacteria) was 0.759(0.704-0.823). When 0.534 was selected as the cut point, the prediction sensitivity of the model in the validation group was 73.08%, and the specificity was 64.71%. K-fold cross validation showed that the training accuracy of 10 groups was 0.778±0.032, and the prediction accuracy was 0.793±0.047.Conclusion The main pathogenic bacteria of PDAP were G+bacteria, and the incidence rate tended to decrease. The risk prediction model could effectively distinguish PDAP caused by G-or G+bacteria. -

-
表 1 细菌培养结果
病原菌 例次(n=232) 百分率/% G+菌 121 52.16 表皮葡萄球菌 28 12.07 金黄色葡萄球菌 30 12.93 溶血葡萄球菌 15 6.47 棒状杆菌 12 5.17 链球菌 20 8.62 肠球菌 5 2.16 其他葡萄球菌 5 2.16 其他 6 2.59 G-菌 95 40.95 大肠杆菌 36 15.52 克雷伯菌 12 5.17 阴沟肠杆菌 13 5.60 假单胞菌 10 4.31 鲍曼不动杆菌 8 3.45 李斯特菌 12 5.17 其他 4 1.72 真菌 16 6.90 白色念珠菌 8 3.45 近平滑念珠菌 4 1.72 其他 4 1.72 合计 232 100.00 表 2 G-菌、G+菌性PDAP患者临床资料差异比较
临床资料 G+菌(n=80) G-菌(n=60) U/t/χ2 P 年龄/岁 56.33±8.34 59.62±7.12 2.457 0.015 BMI/(kg·m-2) 21.47±1.79 21.52±1.96 0.157 0.876 高血压/例(%) 31(38.75) 19(31.67) 0.749 0.387 糖尿病/例(%) 52(65.00) 37(61.67) 0.165 0.686 心血管疾病/例(%) 29(36.25) 19(31.66) 0.320 0.572 腹痛/例(%) 56(70.00) 51(85.00) 4.282 0.039 透析时间/月 17.66±7.21 19.56±6.32 1.626 0.126 WBC/(×109·L-1) 12.51(7.56,16.52) 13.92(7.62,17.11) 1.952 0.120 N/(×109·L-1) 9.94(7.52,14.86) 10.92(7.61,15.33) 1.685 0.202 L/(×109·L-1) 1.96(1.02,4.51) 2.03(1.10,4.72) 0.873 0.387 NLR 7.32±3.12 8.59±3.96 2.122 0.036 PLT/(×109·L-1) 192.34±23.52 197.55±29.11 0.626 0.434 BUN/(μmol·L-1) 17.63±4.12 18.01±4.75 0.506 0.614 Cr/(μmol·L-1) 819.14±65.74 837.17±78.33 1.475 0.142 K+/(mmol·L-1) 4.24±0.87 3.92±0.81 2.218 0.028 Ca2+/(mmol·L-1) 2.15±0.46 2.02±0.51 1.579 0.116 P/(mmol·L-1) 1.67±0.65 1.59±0.71 0.693 0.490 PCT/(μg·L-1) 6.32±2.97 8.75±3.22 4.621 < 0.001 ALB/(g·L-1) 26.52±9.53 25.97±8.11 0.360 0.720 表 3 G-菌性PDAP患者二元logistic回归分析
因素 β SE Wald χ2 P OR 95%CI 腹痛 1.316 0.901 2.134 0.044 3.729 1.021~21.807 年龄 0.112 0.069 3.068 0.040 1.128 1.014~1.326 NLR 1.378 0.530 6.728 0.009 3.968 1.400~11.243 K+ -2.304 0.675 11.643 0.001 0.502 0.314~0.963 PCT 1.859 0.373 25.699 < 0.001 6.618 3.187~13.743 常数项 -16.605 4.475 13.767 < 0.001 表 4 影响因素在建模组和验证组中的一致性检验
影响因素 KS P 腹痛 0.025 0.863 年龄 0.024 0.871 NLR 0.051 0.412 K+ 0.042 0.647 PCT 0.059 0.331 表 5 K折交叉验证
组号 预测准确性 训练准确性 1 0.712 0.746 2 0.801 0.723 3 0.769 0.826 4 0.744 0.742 5 0.789 0.769 6 0.810 0.811 7 0.796 0.853 8 0.794 0.842 9 0.754 0.781 10 0.809 0.834 X±S 0.778±0.032 0.793±0.047 -
[1] Dzekova-Vidimliski P, Nikolov IG, Gjorgjievski N, et al. Peritoneal Dialysis-Related Peritonitis: Rate, Clinical Outcomes and Patient Survival[J]. Pril(Makedon Akad Nauk Umet Odd Med Nauki), 2021, 42(3): 47-55.
[2] Banno T, Shima H, Kawahara K, et al. Risk factors for peritoneal dialysis withdrawal due to peritoneal dialysis-related peritonitis[J]. Nephrol Ther, 2021, 17(2): 108-113. doi: 10.1016/j.nephro.2020.10.007
[3] 杨开洪, 曾庆栈, 冯斌. 尿常规结果对革兰氏阳性菌或阴性菌引起尿路感染评分预测模型的建立和验证[J]. 中国当代医药, 2022, 29(10): 24-28. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGUD202210004.htm
[4] 严月华, 杨春慧, 纪天蓉, 等. 探讨腹膜透析相关性腹膜炎不同转归患者的临床特点[J]. 中国血液净化, 2020, 19(2): 77-80. doi: 10.3969/j.issn.1671-4091.2020.02.002
[5] Gadola L, Poggi C, Dominguez P, et al. Risk Factors And Prevention of Peritoneal Dialysis-Related Peritonitis[J]. Perit Dial Int, 2019, 39(2): 119-125. doi: 10.3747/pdi.2017.00287
[6] Li KT, Szeto CC, Piraino B, et al. International Society for Peritoneal D: peritoneal dialysis-related infections recommendation: 2010 update[J]. Perit Dial Int, 2010, 30(4): 393-423. doi: 10.3747/pdi.2010.00049
[7] 尚红, 王毓三, 申子瑜. 全国临床检验操作规程[M]. 4版. 北京: 人民卫生出版社, 2015: 569-570.
[8] 宋洁, 王栖栖, 沈源, 等. 腹膜透析病人退出原因分析[J]. 安徽医药, 2022, 26(5): 955-958. doi: 10.3969/j.issn.1009-6469.2022.05.025
[9] 李飞, 陈文, 李晓娃, 等. 腹膜透析相关性腹膜炎病原菌分布及耐药性[J]. 中华医院感染学杂志, 2020, 30(8): 1196-1200. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY202008017.htm
[10] Li PK, Szeto CC, Piraino B, et al. ISPD Peritonitis Recommendations: 2016 Update on Prevention and Treatment[J]. Perit Dial Int, 2016, 36(5): 481-508. doi: 10.3747/pdi.2016.00078
[11] 孟令飞, 朱学研, 杨立明, 等. 腹膜透析相关腹膜炎患者治疗失败预测模型的构建和验证: 一项多中心临床研究[J]. 南方医科大学学报, 2022, 42(4): 546-553. https://www.cnki.com.cn/Article/CJFDTOTAL-DYJD202204017.htm
[12] Sakurada T, Fujishima R, Yamada S, et al. Seasonality of peritoneal dialysis-related peritonitis in Japan: a single-center, 10-year study[J]. Clin Exp Nephrol, 2021, 25(1): 52-57. doi: 10.1007/s10157-020-01953-1
[13] 胡静, 易斌, 张浩. 气候因素对单中心腹膜透析相关腹膜炎的影响[J]. 中南大学学报(医学版), 2022, 47(5): 639-649. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYD202205012.htm
[14] 赵丽娟, 柏明, 何丽洁, 等. 腹膜透析相关性腹膜炎致病菌谱及危险因素分析[J]. 疑难病杂志, 2019, 18(11): 1108-1112. doi: 10.3969/j.issn.1671-6450.2019.11.007
[15] 滕兰波, 刘书馨, 王胜男, 等. 维持性腹膜透析患者血清半乳糖凝集素3水平与心血管疾病的相关性研究[J]. 哈尔滨医科大学学报, 2020, 54(5): 498-502. doi: 10.3969/j.issn.1000-1905.2020.05.010
[16] 李飞, 陈文, 李晓娃, 等. 腹膜透析相关性腹膜炎病原菌分布及耐药性[J]. 中华医院感染学杂志, 2020, 30(8): 1196-1200. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY202008017.htm
[17] Zeng Y, Jiang L, Lu Y, et al. Peritoneal dialysis-related peritonitis caused by gram-negative organisms: ten-years experience in a single center[J]. Ren Fail, 2021, 43(1): 993-1003.
[18] Zurowska A, Feneberg R, Warady BA, et al. Gram-negative peritonitis in children undergoing long-term peritoneal dialysis[J]. Am J Kidney Dis, 2008, 51(3): 455-462.
[19] Chuang YW, Shu KH, Yu TM, et al. Hypokalaemia: an independent risk factor of Enterobacteriaceae peritonitis in CAPD patients[J]. Nephrol Dial Transplant, 2009, 24(5): 1603-1608.
[20] 苏晓平, 陈伯莉, 邓丽, 等. 手术前后NLR对口腔癌患者预后预测价值的研究[J]. 现代医学, 2022, 50(5): 561-567. https://www.cnki.com.cn/Article/CJFDTOTAL-TDYX202205006.htm
[21] 刘洋, 曹慧玲, 赵苏瑛, 等. 降钙素原联合中性粒细胞/淋巴细胞比值在不同类型血流感染中的应用价值[J]. 国际检验医学杂志, 2020, 41(13): 1542-1547. https://www.cnki.com.cn/Article/CJFDTOTAL-GWSQ202013003.htm
[22] 朱成斌, 蔡春莲. 血常规指标对初诊多发性骨髓瘤临床分期和预后预测价值的研究[J]. 临床血液学杂志, 2021, 34(10): 723-727. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202110010.htm
[23] 栗萍, 袁晓英, 肖英. 腹膜透析相关性腹膜炎致病菌特点与血清降钙素原的相关性分析[J]. 临床肾脏病杂志, 2018, 18(8): 493-496. https://www.cnki.com.cn/Article/CJFDTOTAL-LCSB201808010.htm
-




 下载:
下载: