-
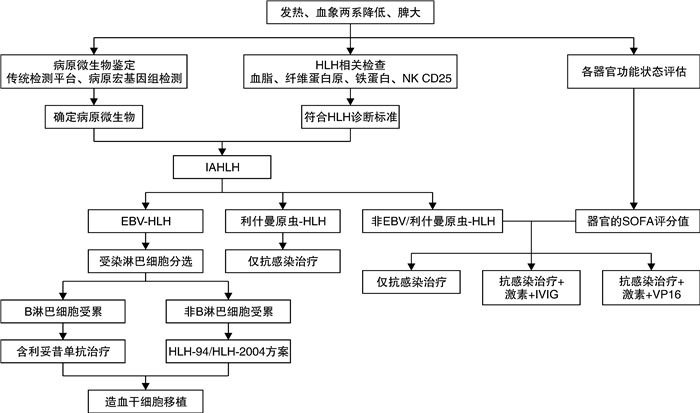
摘要: 继发性噬血细胞综合征中,32.8%~50.4%的诱因为感染。病毒,尤其是人类疱疹病毒,是最常见的病原类型。传统检测技术联合病原宏基因组检测有助于提高病原微生物的检出率,但需结合病情判定检出病原微生物和疾病间的因果关系。发热、外周血两系降低伴无其他原因的脾大、肝损伤,需警惕感染相关噬血细胞综合征。抗感染治疗是感染相关噬血细胞综合征的基础治疗。需根据病情和病原学特点制订“个体化”综合治疗方案。该文综述感染相关噬血细胞综合征的常见病原微生物种类、治疗及预后,以期提高临床救治率。
-
关键词:
- 感染相关噬血细胞综合征 /
- 诊断 /
- 治疗
Abstract: Infection accounts for 32.8%-50.4% of secondary hemophagocytic syndrome. Viruses, especially human herpesvirus, are the most common pathogenic type. Traditional techniques combined metagenomic next-generation sequencing is helpful to find the pathogens, but it is necessary to determine the causal relationship between pathogens and infection-associated hemophagocytic lymphohistiocytosis(IAHLH). Awareness of IAHLH is crucial when patients with infection have unknown splenomegaly and/or liver dysfunction, fever and cytopenia. Anti-infection therapy is the basic treatment of IAHLH. "Tailored" therapy regime is based on the severity of the individual and the characteristics of the pathogen. It reviews the common pathogenic, therapy regime and prognosis of IAHLH, for the improvement of early diagnosis and survival rate. -

-
[1] La Rosée P, Horne A, Hines M, et al. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults[J]. Blood, 2019, 133(23): 2465-2477. doi: 10.1182/blood.2018894618
[2] Ramos-Casals M, Brito-Zerón P, López-Guillermo A, et al. Adult haemophagocytic syndrome[J]. Lancet, 2014, 383(9927): 1503-1516. doi: 10.1016/S0140-6736(13)61048-X
[3] 裴瑞君, 王昭, 王旖旎, 等. 全国多中心噬血细胞性淋巴组织细胞增多症601例病因分析[J]. 中华内科杂志, 2015, 54 (12): 1018-1022. doi: 10.3760/cma.j.issn.0578-1426.2015.12.006
[4] Rouphael NG, Talati NJ, Vaughan C, et al. Infections associated with haemophagocytic syndrome[J]. Lancet Infect Dis, 2007, 7(12): 814-822. doi: 10.1016/S1473-3099(07)70290-6
[5] Maakaroun NR, Moanna A, Jacob JT, et al. Viral infections associated with haemophagocytic syndrome[J]. Rev Med Virol, 2010, 20(2): 93-105. doi: 10.1002/rmv.638
[6] Chevalier K, Schmidt J, Coppo P, et al. Hemophagocytic lymphohistiocytosis associated with cytomegalovirus infection: five cases and a systematic review of the literature[J]. Clin Infect Dis, 2022: ciac649. doi: 10.1093/cid/ciac649
[7] Kan FK, Tan CC, Von Bahr Greenwood T, et al. Dengue Infection Complicated by Hemophagocytic Lymphohistiocytosis: Experiences From 180 Patients With Severe Dengue[J]. Clin Infect Dis, 2020, 70(11): 2247-2255.
[8] 许汪斌, 钱冉, 代冬梅, 等. 成人感染相关性噬血细胞综合征32例临床分析[J]. 中华危重病急救医学, 2020, 32 (7): 797-802. doi: 10.3760/cma.j.cn121430-20200623-00484
[9] Brito-Zerón P, Bosch X, Pérez-de-Lis M, et al. Infection is the major trigger of hemophagocytic syndrome in adult patients treated with biological therapies[J]. Semin Arthritis Rheum, 2016, 45(4): 391-399. doi: 10.1016/j.semarthrit.2015.07.004
[10] Muller WJ, Chaudhury S. Utility of Metagenomic Next-generation Sequencing of Plasma for Infectious Pathogens[J]. Clin Infect Dis, 2020, 71(10): 2775.
[11] Miao Q, Ma Y, Wang Q, et al. Microbiological Diagnostic Performance of Metagenomic Next-generation Sequencing When Applied to Clinical Practice[J]. Clin Infect Dis, 2018, 67(suppl_2): S231-S240. doi: 10.1093/cid/ciy693
[12] Wang S, Ai J, Cui P, et al. Diagnostic value and clinical application of next-generation sequencing for infections in immunosuppressed patients with corticosteroid therapy[J]. Ann Transl Med, 2020, 8(5): 227. doi: 10.21037/atm.2020.01.30
[13] Miller S, Chiu C. The Role of Metagenomics and Next-Generation Sequencing in Infectious Disease Diagnosis[J]. Clin Chem, 2021, 68(1): 115-124. doi: 10.1093/clinchem/hvab173
[14] Casto AM, Fredricks DN, Hill JA. Diagnosis of infectious diseases in immunocompromised hosts using metagenomic next generation sequencing-based diagnostics[J]. Blood Rev, 2022, 53: 100906. doi: 10.1016/j.blre.2021.100906
[15] Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021[J]. Crit Care Med, 2021, 49(11): e1063-e1143. doi: 10.1097/CCM.0000000000005337
[16] Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study[J]. Lancet, 2020, 395(10219): 200-211. doi: 10.1016/S0140-6736(19)32989-7
[17] 尤亚红, 王晶石, 王昭. 非EB病毒病原体所致感染相关噬血细胞综合征的临床特征及预后[J]. 中华血液学杂志, 2022, 43(2): 128-133.
[18] Croden J, Bilston L, Taparia M, et al. Practice patterns and outcomes of hemophagocytic lymphohistiocytosis in adults: a 2-decade provincial retrospective review[J]. Ann Hematol, 2022, 101(10): 2297-2306. doi: 10.1007/s00277-022-04960-2
[19] Hines MR, von Bahr Greenwood T, Beutel G, et al. Consensus-Based Guidelines for the Recognition, Diagnosis and Management of Hemophagocytic Lymphohistiocytosis in Critically Ill Children and Adults[J]. Crit Care Med, 2022, 50(5): 860-872. doi: 10.1097/CCM.0000000000005361
[20] Meng GQ, Wang JS, Wang YN, et al. Rituximab-containing immuno-chemotherapy regimens are effective for the elimination of EBV for EBV-HLH with only and mainly B lymphocytes of EBV infection[J]. Int Immunopharmacol, 2021, 96: 107606. doi: 10.1016/j.intimp.2021.107606
[21] 中国医师协会血液科医师分会, 中华医学会儿科学分会, 血液学组噬血细胞综合征中国专家联盟. 中国噬血细胞综合征诊断与治疗指南(2022年版)[J]. 中华医学杂志, 2022, 102(20): 1492-1499. doi: 10.3760/cma.j.cn112137-20220310-00488
[22] Ehl S, Astigarraga I, von Bahr Greenwood T, et al. Recommendations for the Use of Etoposide-Based Therapy and Bone Marrow Transplantation for the Treatment of HLH: Consensus Statements by the HLH Steering Committee of the Histiocyte Society[J]. J Allergy Clin Immunol Pract, 2018, 6(5): 1508-1517. doi: 10.1016/j.jaip.2018.05.031
[23] Naymagon L, Tremblay D, Mascarenhas J. The Efficacy of Etoposide-Based Therapy in Adult Secondary Hemophagocytic Lymphohistiocytosis[J]. Acta Haematol, 2021, 144(5): 560-568. doi: 10.1159/000514920
[24] Mehta P, Cron RQ, Hartwell J, et al. Silencing the cytokine storm: the use of intravenous anakinra in haemophagocytic lymphohistiocytosis or macrophage activation syndrome[J]. Lancet Rheumatol, 2020, 2(6): e358-e367. doi: 10.1016/S2665-9913(20)30096-5
[25] Dufranc E, Del Bello A, Belliere J, et al. IL6-R blocking with tocilizumab in critically ill patients with hemophagocytic syndrome[J]. Crit Care, 2020, 24(1): 166. doi: 10.1186/s13054-020-02878-7
[26] Locatelli F, Jordan MB, Allen C, et al. Emapalumab in Children with Primary Hemophagocytic Lymphohistiocytosis[J]. N Engl J Med, 2020, 382(19): 1811-1822. doi: 10.1056/NEJMoa1911326
[27] Ahmed A, Merrill SA, Alsawah F, et al. Ruxolitinib in adult patients with secondary haemophagocytic lymphohistiocytosis: an open-label, single-centre, pilot trial[J]. Lancet Haematol, 2019, 6(12): e630-e637. doi: 10.1016/S2352-3026(19)30156-5
[28] Lai W, Wang Y, Wang J, et al. Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in adults and adolescents-a life-threatening disease: analysis of 133 cases from a single center[J]. Hematology, 2018, 23(10): 810-816. doi: 10.1080/10245332.2018.1491093
[29] Giang H, Banno K, Minh L, et al. Dengue hemophagocytic syndrome: A systematic review and meta-analysis on epidemiology, clinical signs, outcomes, and risk factors[J]. Rev Med Virol, 2018, 28(6): e2005.
-

| 引用本文: | 赵鸿, 霍娜, 李俊. 感染相关噬血细胞综合征的诊治现状[J]. 临床血液学杂志, 2023, 36(1): 5-9. doi: 10.13201/j.issn.1004-2806.2023.01.002 |
| Citation: | ZHAO Hong, HUO Na, LI Jun. Diagnosis and treatment of infection-associated hemophagocytic lymphohistiocytosis[J]. J Clin Hematol, 2023, 36(1): 5-9. doi: 10.13201/j.issn.1004-2806.2023.01.002 |
- Figure 1.



 下载:
下载: