Diagnosis and treatment of hemophagocytic syndrome associated with connective tissue disease
-
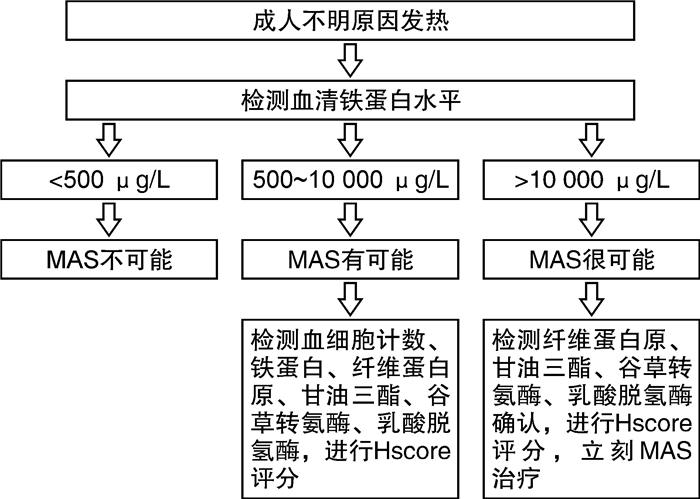
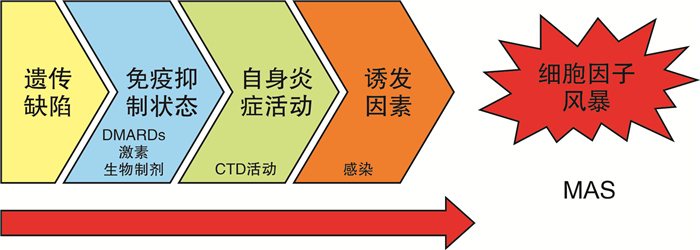
摘要: 巨噬细胞活化综合征(MAS)是一种严重的、可能危及生命的风湿性疾病并发症,早期识别、早期诊断和及时恰当的治疗是改善预后的关键。目前MAS尚无公认的诊断标准,几种临床常用的诊断标准需要更多的研究进一步验证。应重视血清铁蛋白滴度、血清铁蛋白/ESR比例等血清标志物的监测,以提高对MAS的警觉。MAS治疗应该考虑到原发病及诱发因素(尤其是感染),进行个体化治疗。MAS的传统治疗方案为大剂量激素联合免疫抑制剂,对于难治性MAS可尝试新型靶向药物治疗。Abstract: Macrophage activation syndrome (MAS) is a severe, possibly life-threatening complication of rheumatic diseases. Early identification and diagnosis, as well as timely and appropriate treatment are essential to improve prognosis. At present, there are no unified diagnostic criteria for MAS. Most clinical diagnostic criteria commonly used now are needed to be further verified by more studies. It should pay attention to the monitoring of serum markers such as ferritin titer and ferritin/ESR ratio to be alert to MAS. Treatment of MAS should be individualized, taking into account the activity of rheumatic disease and predisposing factors (especially infection). The traditional treatment of MAS is high-dose glucocorticoid combined with immunosuppressive agents, and novel targeted drugs can be tried for refractory MAS.
-

-
表 1 常用的HLH/MAS分类标准
HLH-2004 HScore 2016 sJIA-MAS MScore (1)分子诊断符合HLH;
或
(2)符合以下8条指标中的5条或以上:
①发热:体温>38.5 ℃,持续>7 d;
②脾大;
③血细胞减少(累及外周血两系或三系):血红蛋白<90 g/L(<4周婴儿,血红蛋白<100 g/L),血小板<100×109/L,中性粒细胞<1.0×109/L且非骨髓造血功能减低所致;
④高甘油三酯血症和(或)低纤维蛋白原血症:甘油三酯>3 mmol/L或高于同年龄的3个标准差,纤维蛋白原<1.5 g/L或低于同年龄的3个标准差;
⑤在骨髓、脾脏、肝脏或淋巴结中发现噬血现象;
⑥NK细胞活性降低或缺如;
⑦血清铁蛋白升高:血清铁蛋白≥500 μg/L;
⑧sCD25(可溶性白细胞介素-2受体)升高评分≥169分;
①免疫低下
0分(不)18分(是)
②体温/℃
0分(<38.4)
33分(38.4~39.4)
49分(>39.4)
③肝脾肿大
23分(肝或脾)
38分(肝和脾)
④血细胞减少
24分(2系)
34分(3系)
⑤血清铁蛋白/(ng·mL-1)
35分(2000~6000)
50分(>6000)
⑥甘油三酯/(mmol·L-1)
44分(1.5~4)
64分(>4)
⑦纤维蛋白原/(mg·dL-1)
30分(<2.5)
⑧谷丙转氨酶/(IU·L-1)
19分(>30)
⑨骨髓中发现嗜血细胞
35分(有)(1)sJIA的发热患者;
和
(2)血清铁蛋白>684 ng/mL;
(3)符合以下4条指标中的2条或以上:
①血小板计数≤ 181×109/L;
②谷草转氨酶>48 IU/L;
③甘油三酯>156 mg/dL;
④纤维蛋白原≤360 mg/dL评分≥-2.1分
①中枢神经系统功能障碍(有1无0)
β系数2.44
②出血表现(有1无0)
β系数1.54
③活动性关节炎(有1无0)
β系数-1.30
④血小板/(109·L-1)
β系数-0.003
⑤乳酸脱氢酶/(U·L-1)
β系数0.001
⑥纤维蛋白原/(mg·dL-1)
β系数-0.004
⑦血清铁蛋白/(ng·mL-1)
β系数0.000 1
MS评分=中枢神经系统受累×2.44+出血表现×1.54+活动性关节炎×(-1.30)+血小板计数×(-0.003)+乳酸脱氢酶×0.001+纤维蛋白原×(-0.004)+血清铁蛋白×0.000 1敏感性79% 敏感性93% 敏感性73% 敏感性85% 特异性75% 特异性86% 特异性99% 特异性95% -
[1] La Rosée P, Horne A, Hines M, et al. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults[J]. Blood, 2019, 133(23): 2465-2477. doi: 10.1182/blood.2018894618
[2] Hadchouel M, Prieur AM, Griscelli C. Acute hemorrhagic, hepatic, and neurologic manifestations in juvenile rheumatoid arthritis: possible relationship to drugs or infection[J]. J Pediatr, 1985, 106(4): 561-566. doi: 10.1016/S0022-3476(85)80072-X
[3] Stéphan JL, Zeller J, Hubert P, et al. Macrophage activation syndrome and rheumatic disease in childhood: a report of four new cases[J]. Clin Exp Rheumatol, 1993, 11(4): 451-456.
[4] Kumakura S, Ishikura H, Kondo M, et al. Autoimmune associated hemophagocytic syndrome[J]. Mod Rheumatol, 2004, 14(3): 205-215. doi: 10.3109/s10165-004-0293-6
[5] He L, Yao S, Zhang R, et al. Macrophage activation syndrome in adults: Characteristics, outcomes, and therapeutic effectiveness of etoposide-based regimen[J]. Front Immunol, 2022, 15(13): 955523.
[6] Ke Y, Lv C, Xuan W, et al. Clinical analysis of macrophage activation syndrome in adult rheumatic disease: A multicenter retrospective study[J]. Int J Rheum Dis, 2020, 23(11): 1488-1496. doi: 10.1111/1756-185X.13955
[7] Schulert GS, Cron RQ. The genetics of macrophage activation syndrome[J]. Genes Immun, 2020, 21(3): 169-181. doi: 10.1038/s41435-020-0098-4
[8] Minoia F, Davì S, Horne A, et al. Clinical features, treatment, and outcome of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a multinational, multicenter study of 362 patients[J]. Arthritis Rheumatol, 2014, 66(11): 3160-3169. doi: 10.1002/art.38802
[9] Lehmberg K, Pink I, Eulenburg C, et al. Differentiating macrophage activation syndrome in systemic juvenile idiopathic arthritis from other forms of hemophagocytic lymphohistiocytosis[J]. J Pediatr, 2013, 162(6): 1245-1251. doi: 10.1016/j.jpeds.2012.11.081
[10] Stéphan JL, Koné-Paut I, Galambrun C, et al. Reactive haemophagocytic syndrome in children with inflammatory disorders. A retrospective study of 24 patients[J]. Rheumatology(Oxford), 2001, 40(11): 1285-1292. doi: 10.1093/rheumatology/40.11.1285
[11] Carter SJ, Tattersall RS, Ramanan AV. Macrophage activation syndrome in adults: recent advances in pathophysiology, diagnosis and treatment[J]. Rheumatology(Oxford), 2019, 58(1): 5-17. doi: 10.1093/rheumatology/key006
[12] Gorelik M, Fall N, Altaye M, et al. Follistatin-like protein 1 and the ferritin/erythrocyte sedimentation rate ratio are potential biomarkers for dysregulated gene expression and macrophage activation syndrome in systemic juvenile idiopathic arthritis[J]. J Rheumatol, 2013, 40(7): 1191-1199. doi: 10.3899/jrheum.121131
[13] Eloseily EMA, Minoia F, Crayne CB, et al. Ferritin to Erythrocyte Sedimentation Rate Ratio: Simple Measure to Identify Macrophage Activation Syndrome in Systemic Juvenile Idiopathic Arthritis[J]. ACR Open Rheumatol, 2019, 1(6): 345-349. doi: 10.1002/acr2.11048
[14] Weiss ES, Girard-Guyonvarc'h C, Holzinger D, et al. Interleukin-18 diagnostically distinguishes and pathogenically promotes human and murine macrophage activation syndrome[J]. Blood, 2018, 131(13): 1442-1455. doi: 10.1182/blood-2017-12-820852
[15] Henter JI, Horne A, Aricó M, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis[J]. Pediatr Blood Cancer, 2007, 48(2): 124-131. doi: 10.1002/pbc.21039
[16] Fardet L, Galicier L, Lambotte O, et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome[J]. Arthritis Rheumatol, 2014, 66(9): 2613-2620. doi: 10.1002/art.38690
[17] 柯瑶, 吕成银, 宣文华, 等. HScore评分在结缔组织病合并巨噬细胞活化综合征诊断中的应用价值[J]. 中华风湿病学杂志, 2020, 24(12): 826-829. doi: 10.3760/cma.j.c141217-20200310-00091
[18] Ravelli A, Minoia F, Davì S, et al. 2016 Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative[J]. Arthritis Rheumatol, 2016, 68(3): 566-576. doi: 10.1002/art.39332
[19] Minoia F, Bovis F, Davì S, et al. Development and initial validation of the MS score for diagnosis of macrophage activation syndrome in systemic juvenile idiopathic arthritis[J]. Ann Rheum Dis, 2019, 78(10): 1357-1362. doi: 10.1136/annrheumdis-2019-215211
[20] Mehta P, Cron RQ, Hartwell J, et al. Silencing the cytokine storm: the use of intravenous anakinra in haemophagocytic lymphohistiocytosis or macrophage activation syndrome[J]. Lancet Rheumatol, 2020, 2(6): e358-e367. doi: 10.1016/S2665-9913(20)30096-5
[21] 孙利. 儿童风湿病国际相关诊治指南系列解读之四——儿童风湿病合并巨噬细胞活化综合征诊治指南解读[J]. 中国实用儿科杂志, 2020, 35(4): 259-262. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSEK202004005.htm
[22] 中国医师协会血液科医师分会, 中华医学会儿科学分会血液学组, 噬血细胞综合征中国专家联盟. 中国噬血细胞综合征诊断与治疗指南(2022年版)[J]. 中华医学杂志, 2022, 102(20): 1492-1499. doi: 10.3760/cma.j.cn112137-20220310-00488
[23] Ahmed A, Merrill SA, Alsawah F, et al. Ruxolitinib in adult patients with secondary haemophagocytic lymphohistiocytosis: an open-label, single-centre, pilot trial[J]. Lancet Haematol, 2019, 6(12): e630-e637. doi: 10.1016/S2352-3026(19)30156-5
[24] Locatelli F, Jordan MB, Allen C, et al. Emapalumab in Children with Primary Hemophagocytic Lymphohistiocytosis[J]. N Engl J Med, 2020, 382(19): 1811-1822. doi: 10.1056/NEJMoa1911326
[25] Chiossone L, Audonnet S, Chetaille B, et al. Protection from inflammatory organ damage in a murine model of hemophagocytic lymphohistiocytosis using treatment with IL-18 binding protein[J]. Front Immunol, 2012, 8(3): 239.
[26] Henter JI, Elinder G, Söder O, et al. Incidence in Sweden and clinical features of familial hemophagocytic lymphohistiocytosis[J]. Acta Paediatr Scand, 1991, 80(4): 428-435. doi: 10.1111/j.1651-2227.1991.tb11878.x
[27] Janka GE. Familial hemophagocytic lymphohistiocytosis[J]. Eur J Pediatr, 1983, 140(3): 221-230. doi: 10.1007/BF00443367
[28] Wafa A, Hicham H, Naoufal R, et al. Clinical spectrum and therapeutic management of systemic lupus erythematosus-associated macrophage activation syndrome: a study of 20 Moroccan adult patients[J]. Clin Rheumatol, 2022, 41(7): 2021-2033. doi: 10.1007/s10067-022-06055-9
[29] Borgia RE, Gerstein M, Levy DM, et al. Features, Treatment, and Outcomes of Macrophage Activation Syndrome in Childhood-Onset Systemic Lupus Erythematosus[J]. Arthritis Rheumatol, 2018, 70(4): 616-624. doi: 10.1002/art.40417
-




 下载:
下载: