Analysis of influencing factors and establish of nomogram model of disseminated intravascular coagulation in patients with acute promyelocytic leukemia
-
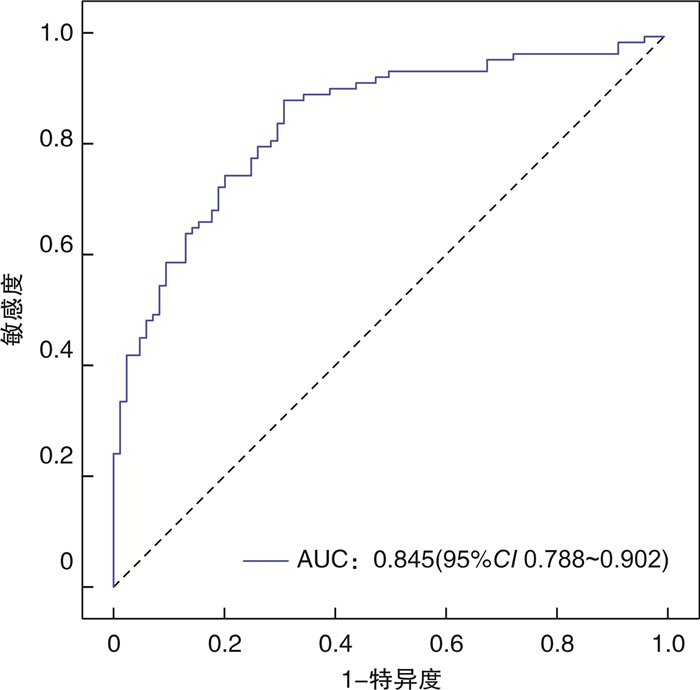
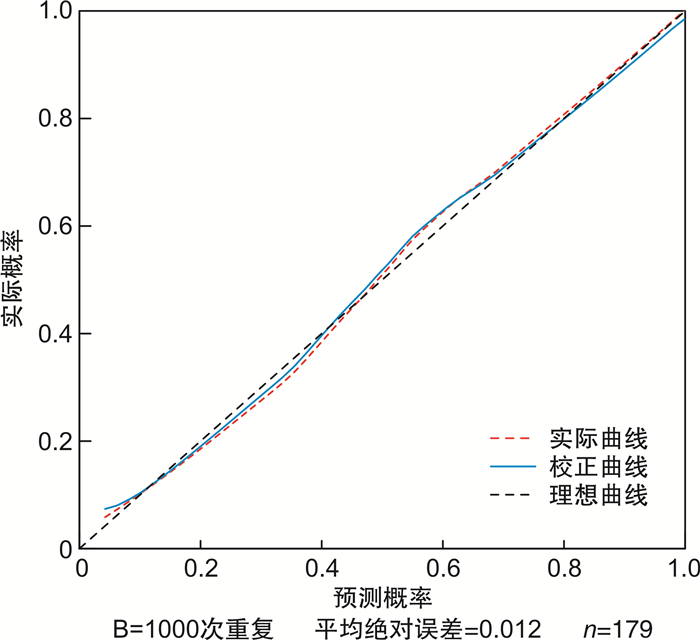
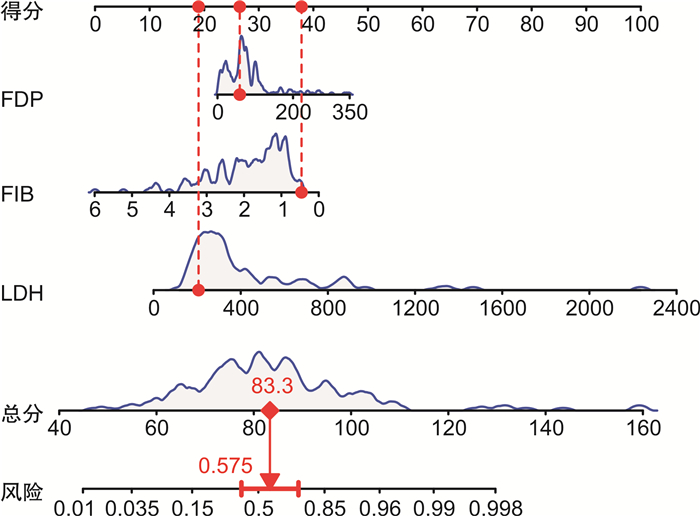
摘要: 目的 探讨急性早幼粒细胞白血病(APL)合并弥散性血管内凝血(DIC)的影响因素,建立初诊APL患者发生DIC风险的预测模型,为临床诊治提供参考。方法 回顾性分析单中心179例初诊APL患者的临床资料,根据有无DIC进行分组,采用单因素及多因素回归分析,探讨APL合并DIC的影响因素,构建列线图预测模型,采用校正曲线、受试者工作特征曲线下的面积(AUC)及一致性指数(CI)评价模型的预测价值。结果 179例初诊APL患者平均年龄41.77岁,根据临床和实验室指标分为DIC组(95例,53.07%),非DIC组(84例,46.93%)。单因素分析显示:预后分层、骨髓早幼粒细胞比例、初诊时白细胞计数、中性粒细胞绝对值、凝血酶原时间、凝血酶时间、纤维蛋白原(FIB)、纤维蛋白降解产物(FDP)、D-二聚体、乳酸脱氢酶(LDH)水平在2组中比较,差异有统计学意义(均P<0.05)。多因素分析显示,初诊时FIB、FDP及LDH水平为APL合并DIC的独立影响因素(OR=0.418、1.009、1.005,P<0.05)。列线图模型预测APL合并DIC的AUC为0.845,CI为0.840,模型的校正曲线与理想曲线贴合良好。结论 初诊APL合并DIC的独立影响因素为FIB、FDP及LDH,基于上述因素构建列线图模型可以预测APL患者发生DIC的风险,可有效进行疾病的评估,具有良好的预测价值。
-
关键词:
- 急性早幼粒细胞白血病 /
- 弥散性血管内凝血 /
- 影响因素 /
- 列线图模型
Abstract: Objective To investigate the clinical features and risk factors of acute promyelocytic leukemia(APL) complicated with disseminated intravascular coagulation(DIC), and to establish a predictive model for the risk of DIC in patients with newly diagnosed APL to provide reference for clinical diagnosis and treatment.Methods Clinical data of 179 patients with newly diagnosed APL in a single center were retrospectively analyzed. All patients were grouped according to whether DIC occurred. Univariate and multivariate regression analysis were used to explore the influencing factors of APL merged DIC. We constructed a nomogram model and evaluated the predictive value of the model by using correction curve, area under the curve(AUC) of receiver operator characteristic and consistency index(CI).Results The average age of the 179 APL patients was 41.77 years. According to clinical and laboratory indicators, 95 case (53.07%) were in the DIC group and 84 cases (46.93%) were in the non-DIC group. Univariate analysis showed that the prognostic stratification, bone marrow promyelocytes percentage and the white blood cell count at initial diagnosis, absolute neutrophil count, prothrombin time, thrombin time, fibrinogen degradation products(FDP), D-Dimer, lactate dehydrogenase level(LDH) and fibrinogen(FIB) significantly different between the two groups(P < 0.05). Multivariate analysis showed that FIB, FDP and LDH at the initial diagnosis were independent influencing factors for APL combined with DIC(OR= 0.418, 1.009 and 1.005, P < 0.05). The nomogram model predicted that the AUC of APL merged with DIC was 0.845, the CI was 0.840, and the calibration curve of the model fit well with the ideal curve.Conclusion The independent influencing factors of initial diagnosed APL combined with DIC are FIB, FDP and LDH, based on the above factors, the nomogram model could predict the risk of DIC in APL patients, and this model can effectively evaluate the disease and has good predictive value. -

-
表 1 APL患者非DIC组与DIC组临床特征比较
例(%) 症状及体征 非DIC组(n=84) DIC组(n=95) 乏力 47(55.95) 53(55.79) 发热 33(39.29) 45(47.37) 皮肤出血 38(45.24) 42(44.21) 黏膜出血 36(42.86) 47(49.47) 头晕恶心 25(29.76) 29(30.53) 月经增多 11(13.10) 9(9.47) 脾肿大 16(19.05) 22(23.16) 淋巴结肿大 2(2.38) 8(8.42) 肝肿大 4(4.76) 4(4.21) 表 2 APL患者非DIC组和DIC组临床资料比较
临床资料 非DIC组(n=84) DIC组(n=95) t/χ2 P 年龄/岁 42.00±15.21 41.57±18.25 0.171 0.864 性别/例(%) 1.521 0.218 男 40(47.62) 54(56.84) 女 44(52.38) 41(43.16) 既往史/例(%) 糖尿病 <0.001 0.991 是 8(9.52) 9(9.47) 否 76(90.48) 86(90.53) 高血压 0.013 0.908 是 11(13.10) 13(13.68) 否 73(86.90) 82(86.32) 银屑病 0.048 0.826 是 3(3.57) 4(4.21) 否 81(96.43) 91(95.79) 手术 <0.001 0.955 是 15(17.86) 17(17.89) 否 69(82.14) 78(82.11) 心脏病 1.099 0.294 是 4(4.76) 1(1.05) 否 80(95.24) 94(98.95) 吸烟 0.694 0.405 是 12(14.29) 18(18.95) 否 72(85.71) 77(81.05) 饮酒 0.284 0.594 是 11(13.10) 10(10.53) 否 73(86.90) 85(89.47) 预后分层/例(%) 7.983 0.018 低危 19(22.62) 13(13.68) 中危 48(57.14) 45(47.37) 高危 17(20.24) 37(38.95) 表 3 APL患者非DIC组与DIC组实验室指标比较
实验室指标 非DIC组(n=84) DIC组(n=95) t/χ2 P 骨髓增生程度a/例(%) 3.505 0.324 极度活跃 29(34.52) 45(47.37) 明显活跃 34(40.48) 32(33.68) 活跃 14(16.67) 11(11.58) 低下 4(4.76) 3(3.16) PML-RARα基因表型b/例(%) 0.289 1.000 L 46(54.76) 53(55.79) S 22(26.19) 24(25.26) V 1(1.19) 1(1.05) 染色体核型c/例(%) 2.452 0.296 正常核型 5(5.95) 2(2.11) t(15;17) 62(73.81) 76(80.00) 其他核型异常 1(1.19) 3(3.16) 骨髓早幼粒细胞比例/% 79.77(69.13,88.38) 85.50(77.50,90.50) -2.878 0.005 WBC/(×109·L-1) 1.93(0.86,6.65) 5.98(1.90,22.54) -4.317 <0.001 Hb/(g·L-1) 77.00(66.00,92.50) 78.00(68.00,95.00) -1.088 0.276 PLT/(×109·L-1) 34.10±3.75 27.91±1.83 1.486 0.140 ANC/(×109·L-1) 0.47(0.18,2.04) 2.66(0.52,11.70) -4.672 <0.001 PT/s 16.85(15.83,18.40) 19.20(17.90,21.80) -5.114 <0.001 TT/s 17.10(15.33,19.11) 18.40(16.80,19.90) -3.154 0.002 FIB/(g·L-1) 2.25(1.46,3.03) 1.27(1.03,1.90) -5.629 <0.001 FDP/(μg·mL-1) 62.59(31.64,73.80) 81.72(43.80,107.97) -3.451 0.001 D-二聚体/(ng·mL-1) 6 688.50(2 265.50,11 993.17) 9 390.00(4 000.00,15 800.00) -2.831 0.005 TP/(g·L-1) 65.32±6.40 65.55±6.33 -0.233 0.816 ALB/(g·L-1) 38.84±4.82 38.99±5.03 -0.208 0.835 GLO/(g·L-1) 26.38(24.43,29.08) 25.64(22.90,29.40) -1.107 0.268 UREA/(mol·L-1) 5.10(4.10,6.00) 4.90(4.30,6.59) -0.491 0.623 Cr/(μmol·L-1) 58.50(51.19,67.84) 63.00(53.00,71.00) -1.031 0.303 LDH/(U·L-1) 271.29(224.00,334.99) 418.00(286.00,718.00) -5.427 <0.001 注:a、b、c:指标数据存在缺失。 表 4 APL患者并发DIC影响因素的logistic回归分析结果
因素 β SE Wald χ2 P OR 95%CI FIB -0.872 0.228 14.680 <0.001 0.418 0.268~0.653 FDP 0.009 0.003 6.650 0.010 1.009 1.002~1.016 LDH 0.005 0.001 19.597 <0.001 1.005 1.003~1.007 -
[1] 马军. 中国急性早幼粒细胞白血病诊疗指南(2018年版)[J]. 中华血液学杂志, 2018, 39(3): 179-183.
[2] Huang Q, Wang T, Xiong Y, et al. Safety and efficacy of Compound Huangdai Tablets combined with all-trans retinoic acid for treatment of acute promyelocytic leukemia: Clinical evidence and potential mechanisms[J]. Chin Herb Med, 2022, 14(1): 154-165. doi: 10.1016/j.chmed.2021.09.004
[3] 金春香, 韩晓雁, 蔡真. 呈现急性早幼粒细胞白血病表现的特殊亚型白血病[J]. 临床血液学杂志, 2020, 33(11): 811-816. http://lcxz.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=fde561fa-7a4f-47bc-9049-d4f6db8611cd
[4] 胡豫, 梅恒. 《中国弥散性血管内凝血诊断积分系统》解读[J]. 临床血液学杂志, 2017, 30(7): 495-498. http://lcxz.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=cee4cbfd-30cb-44dd-a76c-ac6343e7e041
[5] 田梦瑶, 赵艳秋, 李丹丹, 等. 急性早幼粒细胞白血病早期出凝血异常研究进展[J]. 中国临床研究, 2020, 33(11): 1578-1581. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK202011033.htm
[6] Ten Cate H, Leader A. Management of Disseminated Intravascular Coagulation in Acute Leukemias[J]. Hamostaseologie, 2021, 41(2): 120-126. doi: 10.1055/a-1393-8302
[7] Mantha S, Goldman DA, Devlin SM, et al. Determinants of fatal bleeding during induction therapy for acute promyelocytic leukemia in the ATRA era[J]. Blood, 2017, 129(13): 1763-1767. doi: 10.1182/blood-2016-10-747170
[8] Teng-Fei S, Diyaer A, Hong-Ming Z, et al. Evolving of treatment paradigms and challenges in acute promyelocytic leukaemia: A real-world analysis of 1105 patients over the last three decades[J]. Transl Oncol, 2022, 25: 101522. doi: 10.1016/j.tranon.2022.101522
[9] Gill H, Yung Y, Chu HT, et al. Characteristics and predictors of early hospital deaths in newly diagnosed APL: a 13-year population-wide study[J]. Blood Adv, 2021, 5(14): 2829-2838. doi: 10.1182/bloodadvances.2021004789
[10] 顾树江, 张春铭, 樊俊华. 妊娠早期先兆流产患者凝血7项和血小板检测结果分析[J]. 临床血液学杂志, 2022, 35(2): 138-141. http://lcxz.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=0ef7a16e-ca88-4f20-9a14-dc39c48e2d9e
[11] Song YH, Peng P, Qiao C, et al. Low platelet count is potentially the most important contributor to severe bleeding in patients newly diagnosed with acute promyelocytic leukemia[J]. Onco Targets Ther, 2017, 10: 4917-4924. doi: 10.2147/OTT.S144438
[12] 裴艳茹, 宋娟娟, 牛晓娜, 等. 外周血白血病细胞绝对数与急性早幼粒细胞白血病早期严重出血事件相关性分析[J]. 中华实用诊断与治疗杂志, 2021, 35(5): 461-464. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202105007.htm
[13] Baysal M, Gürsoy V, Hunutlu FC, et al. The evaluation of risk factors leading to early deaths in patients with acute promyelocytic leukemia: a retrospective study[J]. Ann Hematol, 2022, 101(5): 1049-1057. doi: 10.1007/s00277-022-04798-8
[14] Ciftciler R, Haznedaroglu IC, Aksu S, et al. The Factors Affecting Early Death in Newly Diagnosed APL Patients[J]. Open Med(Wars), 2019, 14: 647-652. doi: 10.1515/med-2019-0074
[15] 黄月婷, 刘晓帆, 付荣凤, 等. 2017年版中国DIC诊断积分系统在急性早幼粒细胞白血病中的应用[J]. 中华血液学杂志, 2018, 39(6): 480-484.
[16] Pei Y, Shi M, Song J, et al. Absolute Circulating Leukemic Cells as a Risk Factor for Early Bleeding Events in Patients with Non-High-Risk Acute Promyelocytic Leukemia[J]. Cancer Manag Res, 2021, 13: 4135-4146. doi: 10.2147/CMAR.S309138
[17] Bai Y, Shi M, Yang X, et al. The value of FDP/FIB and D-dimer/FIB ratios in predicting high-risk APL-related thrombosis[J]. Leuk Res, 2019, 79: 34-37. doi: 10.1016/j.leukres.2019.02.007
[18] Pang M, Zhao F, Yu P, et al. The significance of coagulation and fibrinolysis-related parameters in predicting postoperative venous thrombosis in patients with breast cancer[J]. Gland Surg, 2021, 10(4): 1439-1446. doi: 10.21037/gs-21-117
[19] 张笑芸, 牛真珍. 外周血涂片镜检联合纤维蛋白(原)降解产物、D-二聚体检测在急性早幼粒细胞白血病早期诊断中的应用[J]. 中国卫生检验杂志, 2019, 29(17): 2104-2106. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ201917016.htm
[20] Luo L, Wu Y, Niu T, et al. A multicenter, prospective evaluation of the Chinese Society of Thrombosis and Hemostasis Scoring System for disseminated intravascular coagulation[J]. Thromb Res, 2019, 173: 131-140. doi: 10.1016/j.thromres.2018.11.022
[21] Zhou W, Zhou W, Bai J, et al. TEG in the monitoring of coagulation changes in patients with sepsis and the clinical significance[J]. Exp Ther Med, 2019, 17(5): 3373-3382.
[22] He YY, Wu XJ, Zhou DH, et al. A Nomogram for Predicting Event-Free Survival in Childhood Acute Lymphoblastic Leukemia: A Multicenter Retrospective Study[J]. Front Oncol, 2022, 12: 854798. doi: 10.3389/fonc.2022.854798
[23] Gui Q, Yang Y, Wang L, et al. A nomogram to predict preterm birth in twin pregnancies[J]. Am J Transl Res, 2022, 14(10): 7119-7127.
[24] Bai Z, Cao X, Yang Y, et al. Establishment and Validation of a Predictive Nomogram for Hallux Valgus with Pain Under the Second Metatarsal[J]. J Pain Res, 2022, 15: 3523-3536. doi: 10.2147/JPR.S386315
[25] Han Y, Shi Y, Chen B, et al. An ion-channel-gene-based prediction model for head and neck squamous cell carcinoma: Prognostic assessment and treatment guidance[J]. Front Immunol, 2022, 13: 961695. doi: 10.3389/fimmu.2022.961695
-




 下载:
下载: