-
摘要: 嗜酸性粒细胞增多症是一组高度异质性疾病,主要包括非血液学(反应性)和血液学(肿瘤性)两类。既往的诊治手段不断优化,新兴的诊治方法层出不穷,改善了嗜酸性粒细胞增多症的诊疗及预后。这些进展在血液系统,尤其是恶性髓或淋系肿瘤伴嗜酸性粒细胞增多领域尤为显著。该文主要对此类疾病的定义、分类、诊断、治疗及预后的研究进展进行综述。Abstract: Eosinophilia is a group of highly heterogeneous diseases, mainly including non-hematologic(reactive) and hematologic(neoplastic) categories. The previous diagnosis and treatment methods are constantly optimized, and new diagnosis and treatment methods emerge in endlessly, which greatly improve the diagnosis, treatment and prognosis of eosinophilia. These advances are particularly significant in the hematological system, especially in the area of malignant myeloid or lymphoid neoplasms with eosinophilia. The article reviews progresses in the definition, classification, diagnosis, treatment and prognosis of this kind of disease.
-
Key words:
- eosinophilia /
- myeloid neoplasms /
- lymphoid neoplasms
-

-
[1] Shomali W, Gotlib J. World Health Organization-defined eosinophilic disorders: 2022 update on diagnosis, risk stratification, and management[J]. Am J Hematol, 2022, 97(1): 129-148. doi: 10.1002/ajh.26352
[2] Yao J, Xu L, Aypar U, et al. Myeloid/lymphoid neoplasms with eosinophilia/basophilia and ETV6-ABL1 fusion: cell-of-origin and response to tyrosine kinase inhibition[J]. Haematologica, 2021, 106(2): 614-618.
[3] 中华医学会血液学分会白血病淋巴瘤学组. 嗜酸粒细胞增多症诊断与治疗中国专家共识(2017年版)[J]. 中华血液学杂志, 2017, 38(7): 561-565.
[4] Barraco D, Carobolante F, Candoni A, et al. Complete and long-lasting cytologic and molecular remission of FIP1L1-PDGFRA-positive acute eosinophil myeloid leukaemia, treated with low-dose imatinib monotherapy[J]. Eur J Haematol, 2014, 92(6): 541-545. doi: 10.1111/ejh.12272
[5] Rohmer J, Couteau-Chardon A, Trichereau J, et al. Epidemiology, clinical picture and long-term outcomes of FIP1L1-PDGFRA-positive myeloid neoplasm with eosinophilia: Data from 151 patients[J]. Am J Hematol, 2020, 95(11): 1314-1323. doi: 10.1002/ajh.25945
[6] Grunewald S, Klug LR, Mühlenberg T, et al. Resistance to Avapritinib in PDGFRA-Driven GIST Is Caused by Secondary Mutations in the PDGFRA Kinase Domain[J]. Cancer Discov, 2021, 11(1): 108-125. doi: 10.1158/2159-8290.CD-20-0487
[7] Zhang Y, Gao Y, Zhang H, et al. PDGFRB mutation and tyrosine kinase inhibitor resistance in Ph-like acute lymphoblastic leukemia[J]. Blood, 2018, 131(20): 2256-2261. doi: 10.1182/blood-2017-11-817510
[8] Cowell JK, Hu T. Mechanisms of resistance to FGFR1 inhibitors in FGFR1-driven leukemias and lymphomas: implications for optimized treatment[J]. Cancer Drug Resist, 2021, 4: 607-619.
[9] Chase A, Bryant C, Score J, et al. Ponatinib as targeted therapy for FGFR1 fusions associated with the 8p11 myeloproliferative syndrome[J]. Haematologica, 2013, 98(1): 103-106. doi: 10.3324/haematol.2012.066407
[10] Khodadoust MS, Luo B, Medeiros BC, et al. Clinical activity of ponatinib in a patient with FGFR1-rearranged mixed-phenotype acute leukemia[J]. Leukemia, 2016, 30(4): 947-950. doi: 10.1038/leu.2015.136
[11] Schwaab J, Naumann N, Luebke J, et al. Response to tyrosine kinase inhibitors in myeloid neoplasms associated with PCM1-JAK2, BCR-JAK2 and ETV6-ABL1 fusion genes[J]. Am J Hematol, 2020, 95(7): 824-833. doi: 10.1002/ajh.25825
[12] Khoury P, Abiodun AO, Holland-Thomas N, et al. Hypereosinophilic Syndrome Subtype Predicts Responsiveness to Glucocorticoids[J]. J Allergy Clin Immunol Pract, 2018, 6(1): 190-195. doi: 10.1016/j.jaip.2017.06.006
[13] Ogbogu PU, Bochner BS, Butterfield JH, et al. Hypereosinophilic syndrome: a multicenter, retrospective analysis of clinical characteristics and response to therapy[J]. J Allergy Clin Immunol, 2009, 124(6): 1319-1325.e3. doi: 10.1016/j.jaci.2009.09.022
[14] Dahabreh IJ, Giannouli S, Zoi C, et al. Management of hypereosinophilic syndrome: a prospective study in the era of molecular genetics[J]. Medicine(Baltimore), 2007, 86(6): 344-354.
[15] Helbig G, Klion AD. Hypereosinophilic syndromes-An enigmatic group of disorders with an intriguing clinical spectrum and challenging treatment[J]. Blood Rev, 2021, 49: 100809. doi: 10.1016/j.blre.2021.100809
[16] Luciano L, Catalano L, Sarrantonio C, et al. AlphaIFN-induced hematologic and cytogenetic remission in chronic eosinophilic leukemia with t(1;5)[J]. Haematologica, 1999, 84(7): 651-653.
[17] Naymagon L, Marcellino B, Mascarenhas J. Eosinophilia in acute myeloid leukemia: Overlooked and underexamined[J]. Blood Rev, 2019, 36: 23-31. doi: 10.1016/j.blre.2019.03.007
[18] Choi C, Moller D, Tan J, et al. Pegylated interferon alpha 2a is an effective and well-tolerated treatment option for lymphocyte-variant hypereosinophilic syndrome[J]. Br J Haematol, 2020, 188(5): e68-e72.
[19] Carpentier C, Verbanck S, Schandené L, et al. Eosinophilia Associated With CD3-CD4+T Cells: Characterization and Outcome of a Single-Center Cohort of 26 Patients[J]. Front Immunol, 2020, 11: 1765. doi: 10.3389/fimmu.2020.01765
[20] Gleich GJ, Roufosse F, Chupp G, et al. Safety and Efficacy of Mepolizumab in Hypereosinophilic Syndrome: An Open-Label Extension Study[J]. J Allergy Clin Immunol Pract, 2021, 9(12): 4431-4440.e1. doi: 10.1016/j.jaip.2021.07.050
[21] Kuang FL, Legrand F, Makiya M, et al. Benralizumab for PDGFRA-Negative Hypereosinophilic Syndrome[J]. N Engl J Med, 2019, 380(14): 1336-1346. doi: 10.1056/NEJMoa1812185
[22] Strati P, Cortes J, Faderl S, et al. Long-term follow-up of patients with hypereosinophilic syndrome treated with Alemtuzumab, an anti-CD52 antibody[J]. Clin Lymphoma Myeloma Leuk, 2013, 13(3): 287-291. doi: 10.1016/j.clml.2012.09.018
[23] 王健民, 龚胜蓝. 原发性嗜酸粒细胞增多症的诊断与治疗[J]. 临床血液学杂志, 2021, 34(11): 753-757. http://lcxz.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=1628f80d-377e-4320-8913-b54db1cae157
[24] 邵鲜芳, 魏巍, 韩薇, 等. 61例伴血栓形成的高嗜酸粒细胞综合征患者临床特征及预后因素分析[J]. 中国实验诊断学, 2019, 23(4): 646-648. doi: 10.3969/j.issn.1007-4287.2019.04.025
[25] Jia Q, Qin D, He F, et al. Peripheral eosinophil counts predict efficacy of anti-CD19 CAR-T cell therapy against B-lineage non-Hodgkin lymphoma[J]. Theranostics, 2021, 11(10): 4699-4709. doi: 10.7150/thno.54546
[26] Kluin-Nelemans HC, Reiter A, Illerhaus A, et al. Prognostic impact of eosinophils in mastocytosis: analysis of 2350 patients collected in the ECNM Registry[J]. Leukemia, 2020, 34(4): 1090-1101. doi: 10.1038/s41375-019-0632-4
[27] Wimazal F, Germing U, Kundi M, et al. Evaluation of the prognostic significance of eosinophilia and basophilia in a larger cohort of patients with myelodysplastic syndromes[J]. Cancer, 2010, 116(10): 2372-2381.
[28] Takafumi M, Hiroshi H, Akihiko Y, et al. Prevalence and clinical characteristics of myelodysplastic syndrome with bone marrow eosinophilia or basophilia[J]. Blood, 2003, 101(9): 3386-3390. doi: 10.1182/blood-2002-03-0947
[29] Rai S, Espinoza JL, Morita Y, et al. Severe Eosinophilia in Myelodysplastic Syndrome With a Defined and Rare Cytogenetic Abnormality[J]. Front Immunol, 2019, 9: 3031. doi: 10.3389/fimmu.2018.03031
-

| 引用本文: | 王倩, 周卢琨, 陈宝安. 血液疾病相关嗜酸性粒细胞增多症的研究进展[J]. 临床血液学杂志, 2023, 36(1): 71-75. doi: 10.13201/j.issn.1004-2806.2023.01.015 |
| Citation: | WANG Qian, ZHOU Lukun, CHEN Bao'an. Progress in hematologic diseases with eosinophilia[J]. J Clin Hematol, 2023, 36(1): 71-75. doi: 10.13201/j.issn.1004-2806.2023.01.015 |
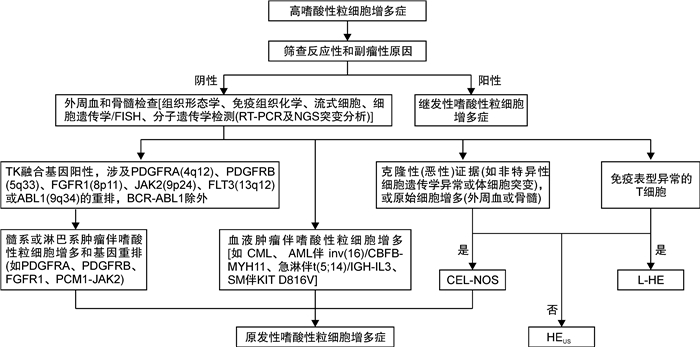
- Figure 1.



 下载:
下载: