Clinical significance and prognostic analysis of CD56 antigen expression in acute promyelocytic leukemia
-
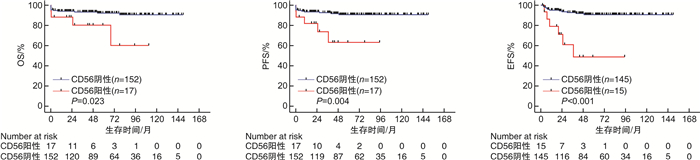
摘要: 目的 分析CD56抗原在初诊急性早幼粒细胞白血病(acute promyelocytic leukemia,APL)中的表达及其与临床参数之间的相关性,探究该抗原的临床意义及对预后的影响。方法 回顾性分析169例初诊APL患者的临床数据,按照CD56抗原表达状况,将其分为CD56阳性和CD56阴性组,比较2组患者性别、年龄、体能状态(ECOG)、血细胞计数、生化指标、凝血功能、骨髓及外周血早幼粒细胞比例、免疫分型、危险分层、FLT3突变、染色体核型、PML/RAR α异聚体类型及融合率、FAB分型(M3a/M3b/M3v)、弥散性血管内凝血(disseminated intravascular coagulation,DIC)积分等参数有无差异。以达分子学缓解(molecular complete remission,mCR)的时间为界,将临床事件分为早期事件(分化综合征、QT间期延长、出血、栓塞、死亡)和晚期事件(继发第二肿瘤、QT间期延长、出血、疾病复发、死亡),比较2组早晚期事件发生率的差异。探索CD56阳性表达对总生存期(OS)、无进展生存期(PFS)及无事件生存期(EFS)的影响。结果 169例APL患者中,17例患者CD56阳性,该抗原的阳性表达率为10.1%。CD56阳性和阴性患者在D-二聚体水平和共表达CD64抗原方面比较,差异有统计学意义(P=0.016,0.017)。CD56阳性组患者达mCR时间更长(P=0.023),2组患者的早期事件发生率差异无统计学意义,2组患者的疾病复发事件差异有统计学意义(P=0.014)。中位随访63.0个月,CD56阳性患者具有更差的OS、PFS和EFS(P=0.023,0.004,< 0.001)。多因素分析显示CD56阳性是PFS、EFS的独立不良因素(P=0.018,< 0.001)。结论 CD56阳性是APL的预后不良因素,临床医师需根据该抗原的表达与否决定APL患者的全程管理策略。
-
关键词:
- 急性早幼粒细胞白血病 /
- CD56抗原表达 /
- 临床特征 /
- 预后分析
Abstract: Objective To analyze the expression of CD56 antigen in newly diagnosed acute promyelocytic leukemia(acute promyelocytic leukemia, APL) and its correlation with clinical parameters, and to explore the clinical significance of this antigen and its influence on the prognosis.Methods Clinical data from 169 patients with new diagnosis APL in our hospital were retrospectively analyzed. According to the expression of CD56 antigen, patients were divided into CD56 positive group and CD56 negative group. The gender, age, ECOG, blood cell count, biochemical criterion, coagulation function, bone marrow and peripheral blood promyelocytic proportions, immunophenotype, risk stratification, FLT3 mutation, chromosome karyotype, PML/RAR α heteromer type and fusion rate, FAB type(M3a/M3b/M3v), disseminated intravascular coagulation(DIC) score were compared between the two groups. Based on the time to molecular complete remission(mCR), clinical events were divided into early events(differentiation syndrome, QT prolongation, bleeding, embolism, death) and late events(secondary tumor, QT prolongation, bleeding, disease recurrence, death), and the difference in the incidence of early and late events was compared. To explore the effects of CD56 positive expression on overall survival(OS), progression-free survival(PFS) and event-free survival(EFS).Results Among 169 patients with APL, 17 patients were positive for CD56, and the positive expression rate was 10.1%. There were significant differences in D-dimer level(P=0.016) and expression of CD64 antigen(P=0.017). CD56 positive group had longer time to reach mCR(P=0.023), and no significant difference was observed in the incidence of early events, while the incidence of disease recurrence event was distinctly different between the two groups(P=0.014). With a median follow-up period of 63.0 months, CD56 positive patients had worse OS, PFS, and EFS(P=0.023, 0.004, < 0.001). Multivariate analysis suggested that the expression of CD56 was an independent adverse factor of PFS and EFS(P=0.018, < 0.001).Conclusion CD56 positive expression is a poor prognostic factor of APL, and clinicians should determine the long-term management strategy of APL patients according to the expression of this antigen. -

-
表 1 CD56阳性和CD56阴性APL患者的基线特征
特征 CD56阳性(n=17) CD56阴性(n=152) P 男/例(%) 7(41.2) 67(44.1) 1.000 年龄/岁 34.0(23.0~64.0) 43.0(16.0~75.0) 0.987 ECOG评分≥2分/例(%) 7(41.2) 68(44.7) 0.804 白细胞计数/(×109/L) 3.0(1.5,18.0) 2.4(1.1,13.5) 0.384 贫血 < 60 g/L/例(%) 1(5.9) 24(15.8) 0.465a 血小板计数/(×109/L) 37.0(26.0,54.0) 27.0(14.3,49.0) 0.162 LDH/(U/L) 252.0(185.0,488.0) 285.0(195.0,475.0) 0.800 低白蛋白血症 < 35 g/L/例(%) 0 15(9.9) 0.368b 甘油三酯/(mmol/L) 1.8(1.3,2.4) 1.7(1.1,2.5) 0.638 胆固醇/(mmol/L) 4.5(4.0,5.2) 4.2(3.5,4.9) 0.101 APTT/s 28.2(24.2,33.6) 26.7(24.7,29.8) 0.270 PT/s 15.0(12.6,15.5) 13.5(12.5,15.0) 0.249 纤维蛋白原/(g/L) 0.9(0.8,1.7) 1.3(0.8,1.8) 0.177 D-二聚体/(mg/L) 20.9(4.2,32.3) 6.4(2.8,16.3) 0.016 骨髓早幼粒细胞比例/% 85.5(76.6,91.3) 84.0(74.8,90.5) 0.826 外周血早幼粒细胞比例/% 65.0(20.5,91.5) 39.0(2.3,74.8) 0.124 CD2阳性/例(%) 3(17.6) 12(7.9) 0.373a CD7阳性/例(%) 1(5.9) 9(5.9) 1.000a CD11b阳性/例(%) 1(5.9) 18(11.8) 0.739a CD15阳性/例(%) 2(11.8) 20(13.2) 1.000a CD19阳性/例(%) 2(11.8) 3(2.0) 0.135a CD34阳性/例(%) 5(29.4) 21(13.8) 0.182a CD64阳性/例(%) 13(76.5) 65(42.8) 0.017a CD117阳性/例(%) 15(88.2) 141(92.8) 0.854a HLA-DR阳性/例(%) 1(5.9) 15(9.9) 0.924a 危险分层/例(%) 0.578 低中危 11(64.7) 109(71.7) 高危 6(35.3) 43(28.3) FLT3突变/例(%) 1.000a 无 13(76.5) 118(77.6) 有 4(23.5) 34(22.4) 染色体核型/例(%) 0.854a 良好+正常 13(76.5) 124(81.6) 异常+复杂 4(23.5) 28(18.4) 类型/例(%) 0.062 1型+2型 7(41.2) 100(65.8) 3型 10(58.8) 52(34.2) 融合率/% 86.0(75.0,93.8) 79.5(64.1,91.9) 0.115 FAB分型/例(%) 1.000b 3a+3b 17(100.0) 147(96.7) 3v 0 5(3.3) DIC积分/例(%) 0.994a < 5分 1(5.9) 14(9.2) ≥5分 16(94.1) 138(90.8) a连续校正的χ2检验;bFisher's检验。 表 2 单因素Cox回归分析
因素 OS PFS EFS P HR(95%CI) P HR(95%CI) P HR(95%CI) 女性 0.035 0.321(0.111~0.924) 0.033 0.345(0.129~0.920) 0.976 0.986(0.375~2.590) 年龄>60岁 0.145 2.545(0.725~8.934) 0.215 2.191(0.634~7.569) 0.663 1.388(0.317~6.072) ECOG评分≥2分 0.019 3.874(1.249~12.018) 0.017 3.501(1.248~9.822) 0.625 1.268(0.489~3.287) 白细胞计数>10×109/L 0.047 2.695(1.011~7.185) 0.026 2.857(1.133~7.204) 0.316 1.664(0.615~4.501) 贫血 < 60 g/L 0.741 1.236(0.352~4.342) 0.871 1.108(0.321~3.830) 0.783 1.192(0.342~4.150) 血小板计数 < 40×109/L 0.446 1.644(0.458~5.898) 0.197 2.261(0.654~7.813) 0.498 1.473(0.480~4.519) CD2阳性 0.081 3.094(0.870~10.999) 0.153 2.477(0.714~8.591) 0.471 1.725(0.392~7.584) CD7阳性 0.134 3.139(0.703~14.021) 0.230 2.465(0.565~10.756) 0.795 1.308(0.173~9.891) CD11b阳性 0.632 1.442(0.322~6.454) 0.885 1.114(0.255~4.864) 0.214 2.216(0.633~7.764) CD15阳性 0.389 0.411(0.054~3.113) 0.314 0.355(0.047~2.669) 0.302 0.345(0.046~2.601) CD19阳性 0.663 0.048(0~41 871.343) 0.643 0.048(0~18 512.361) 0.399 2.396(0.315~18.228) CD56阳性 0.033 3.458(1.109~10.785) 0.008 4.051(1.434~11.446) < 0.001 7.059(2.573~19.366) CD34阳性 0.020 3.320(1.206~9.139) 0.007 3.712(1.436~9.593) 0.024 3.158(1.166~8.551) CD64阳性 0.436 0.654(0.224~1.907) 0.436 0.676(0.252~1.811) 0.279 1.700(0.651~4.442) CD117阳性 0.001 0.174(0.060~0.501) 0.002 0.190(0.067~0.533) 0.334 0.483(0.110~2.113) HLA-DR阳性 0.525 1.622(0.366~7.194) 0.725 1.303(0.299~5.678) 0.410 0.043(0~76.287) 危险分层,高危 0.055 2.607(0.978~6.948) 0.033 2.732(1.084~6.887) 0.365 1.584(0.585~4.284) FLT基因突变 0.018 3.307(1.227~8.914) 0.046 2.628(1.017~6.790) 0.947 0.959(0.275~3.339) 类型,3型 0.035 2.972(1.080~8.180) 0.027 2.917(1.130~7.532) 0.281 1.690(0.652~4.381) 染色体状态,异常+复杂 0.232 1.908(0.668~5.500) 0.122 2.168(0.813~5.779) 0.021 3.129(1.191~8.220) 形态学,3v 0.323 2.782(0.366~21.124) 0.422 2.284(0.304~17.189) 0.655 0.048(0~29 174.387) 低白蛋白血症 < 35 g/L 0.703 0.675(0.089~5.111) 0.614 0.595(0.079~4.474) 0.630 0.609(0.081~4.591) LDH升高>245 U/L 0.024 5.480(1.245~24.118) 0.013 6.480(1.489~28.197) 0.402 1.531(0.566~4.139) 低胆固醇 < 2.90 mmol/L 0.876 0.851(0.112~6.442) 0.762 0.732(0.097~5.5023) 0.433 0.044(0~109.041) 高甘油三酯>1.70 mmol/L 0.275 1.758(0.639~4.839) 0.545 1.333(0.526~3.378) 0.433 1.333(0.526~3.378) 低纤维蛋白原 < 1.0 g/L 0.051 2.683(0.998~7.213) 0.047 2.562(1.011~6.494) 0.729 1.183(0.456~3.068) D-二聚体升高>正常值5倍 0.127 4.854(0.639~36.879) 0.106 5.285(0.702~39.773) 0.145 31.969(0.301~3 391.894) PT时间延长≥3 s 0.002 7.261(2.066~25.522) 0.002 7.162(2.069~24.784) 0.392 2.417(0.320~18.235) 表 3 多因素Cox回归分析
因素 OS PFS EFS P HR(95%CI) P HR(95%CI) P HR(95%CI) 女性 0.038 0.264(0.075~0.930) 0.036 0.288(0.090~0.920) - - ECOG评分≥2分 0.157 2.515(0.701~9.028) 0.142 2.389(0.747~7.638) - - 白细胞计数>10×109/L 0.774 0.832(0.237~2.923) 0.951 657.495(0~+∞) - - CD56阳性 0.057 3.567(0.964~13.206) 0.018 4.503(1.294~15.670) < 0.001 7.376(2.644~20.572) CD34阳性 0.316 1.944(0.530~7.135) 0.275 1.974(0.582~6.700) 0.059 2.617(0.965~7.101) CD117阳性 0.039 0.225(0.055~0.925) 0.029 0.205(0.049~0.853) - - 危险分层,高危 - - 0.950 0.001(0~+∞) - - FLT基因突变 0.217 2.162(0.636~7.350) 0.599 1.370(0.423~4.439) - - 类型,3型 0.916 0.934(0.264~3.307) 0.968 1.024(0.319~3.290) - - 染色体状态,异常+复杂 - - - - 0.019 3.214(1.209~8.545) LDH升高>245 U/L 0.146 3.545(0.645~19.491) 0.062 4.939(0.921~26.494) - - 低纤维蛋白原 < 1.0 g/L - - 0.718 1.223(0.410~3.652) - - PT时间延长≥3 s 0.866 1.167(0.194~7.023) 0.846 1.189(0.207~6.823) - - -
[1] Thomas X. Acute promyelocytic leukemia: a history over 60 years-from the most malignant to the most curable form of acute leukemia[J]. Oncol Ther, 2019, 7(1): 33-65. doi: 10.1007/s40487-018-0091-5
[2] 中华医学会血液学分会. 中国急性早幼粒细胞白血病诊疗指南(2018版)[J]. 中华血液学杂志, 2018, 39(3): 179-183.
[3] Sanz MA, Fenaux P, Tallman MS, et al. Management of acute promyelocytic leukemia: updated recommendations from an expert panel of the European LeukemiaNet[J]. Blood, 2019, 133(15): 1630-1643. doi: 10.1182/blood-2019-01-894980
[4] Testa U, Lo-Coco F. Prognostic factors in acute promyelocytic leukemia: strategies to define high-risk patients[J]. Ann Hematol, 2016, 95(5): 673-680. doi: 10.1007/s00277-016-2622-1
[5] Epstein-Peterson ZD, Derkach A, Geyer S, et al. Effect of additional cytogenetic abnormalities on survival in arsenic trioxide-treated acute promyelocytic leukemia[J]. Blood Adv, 2022, 6(11): 3433-3439. doi: 10.1182/bloodadvances.2021006682
[6] Breccia M, De Propris MS, Minotti C, et al. Aberrant phenotypic expression of CD15 and CD56 identifies poor prognostic acute promyelocytic leukemia patients[J]. Leuk Res, 2014, 38(2): 194-197. doi: 10.1016/j.leukres.2013.11.008
[7] Ono T, Takeshita A, Kishimoto Y, et al. Expression of CD56 is an unfavorable prognostic factor for acute promyelocytic leukemia with higher initial white blood cell counts[J]. Cancer Sci, 2014, 105(1): 97-104. doi: 10.1111/cas.12319
[8] Xu S, Li X, Zhang J, et al. Prognostic value of CD56 in patients with acute myeloid leukemia: a meta-analysis[J]. J Cancer Res Clin Oncol, 2015, 141(10): 1859-1870. doi: 10.1007/s00432-015-1977-3
[9] 马荣军, 朱尊民, 袁晓莉, 等. 成人急性早幼粒细胞白血病预后相关因素分析[J]. 中华血液学杂志, 2017, 38(7): 592-596.
[10] 杨柳, 梁晶晶, 董春霞, 等. 急性早幼粒细胞白血病患者合并弥散性血管内凝血的影响因素及列线图模型构建[J]. 临床血液学杂志, 2023, 36(1): 21-26. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2023.01.005
[11] 李娜, 窦春慧, 管浩然, 等. 维甲酸联合亚砷酸治疗伴FLT3-ITD突变的APL患者的预后分析[J]. 临床血液学杂志, 2019, 32(9): 687-692. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ201909011.htm
[12] Chen C, Huang XL, Wang KL, et al. Early mortality in acute promyelocytic leukemia: potential predictors[J]. Oncol Lett, 2018, 15(4): 4061-4069.
[13] Sobas M, Montesinos P, Boluda B, et al. An analysis of the impact of CD56 expression in de novo acute promyelocytic leukemia patients treated with upfront all-trans retinoic acid and anthracycline-based regimens[J]. Leuk Lymphoma, 2019, 60(4): 1030-1035. doi: 10.1080/10428194.2018.1516875
[14] Montesinos P, Rayón C, Vellenga E, et al. Clinical significance of CD56 expression in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline-based regimens[J]. Blood, 2011, 117(6): 1799-1805. doi: 10.1182/blood-2010-04-277434
[15] Montesinos P, Bergua JM, Vellenga E, et al. Differentiation syndrome in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline chemotherapy: characteristics, outcome, and prognostic factors[J]. Blood, 2009, 113(4): 775-783. doi: 10.1182/blood-2008-07-168617
[16] de la Serna J, Montesinos P, Vellenga E, et al. Causes and prognostic factors of remission induction failure in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and idarubicin[J]. Blood, 2008, 111(7): 3395-3402. doi: 10.1182/blood-2007-07-100669
[17] Guglielmi C, Martelli MP, Diverio D, et al. Immunophenotype of adult and childhood acute promyelocytic leukaemia: correlation with morphology, type of PML gene breakpoint and clinical outcome. A cooperative Italian study on 196 cases[J]. Br J Haematol, 1998, 102(4): 1035-1041.
[18] Albano F, Mestice A, Pannunzio A, et al. The biological characteristics of CD34+ CD2+ adult acute promyelocytic leukemia and the CD34 CD2 hypergranular(M3) and microgranular(M3v)phenotypes[J]. Haematologica, 2006, 91(3): 311-316.
[19] Ng CH, Chng WJ. Recent advances in acute promyelocytic leukaemia[J]. F1000Research, 2017, 6: 1273.
[20] Lou YJ, Ma YF, Suo SS, et al. Prognostic factors of patients with newly diagnosed acute promyelocytic leukemia treated with arsenic trioxide-based frontline therapy[J]. Leuk Res, 2015, 39(9): 938-944.
[21] Takeshita A, Asou N, Atsuta Y, et al. Impact of CD56 continuously recognizable as prognostic value of acute promyelocytic leukemia: results of multivariate analyses in the Japan adult leukemia study group(JALSG)-APL204 study and a review of the literature[J]. Cancers(Basel), 2020, 12(6): 1444.
[22] Guru Murthy GS, Szabo A, Michaelis L, et al. Improving outcomes of acute promyelocytic leukemia in the current era: analysis of the SEER database[J]. J Natl Compr Canc Netw, 2020, 18(2): 169-175.
[23] Tallman MS, Altman JK. Curative strategies in acute promyelocytic leukemia[J]. Hematology Am Soc Hematol Educ Program, 2008: 391-399.
-




 下载:
下载: