Clinical characteristics and prognosis of 27 patients with primary plasma cell leukemia
-
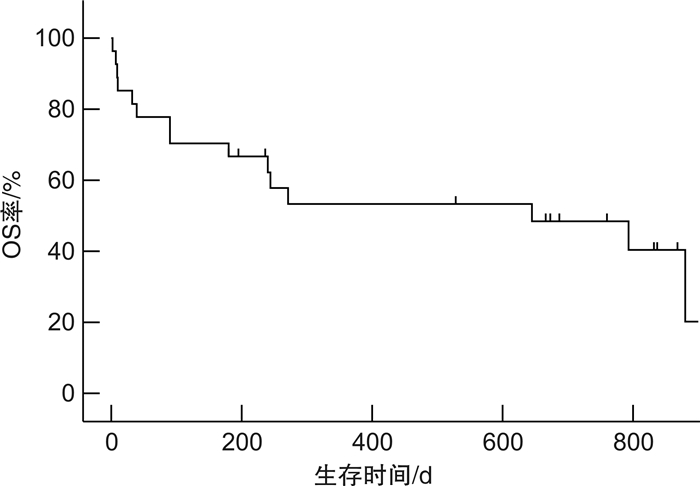
摘要: 目的 探讨原发性浆细胞白血病(primary plasma cell leukemia,pPCL)患者的临床特征及预后分析。方法 选取在郑州大学第一附属医院2018年5月—2022年5月就诊的pPCL患者,收集患者的临床特征、细胞免疫表型、FISH检测、NGS基因检测、治疗和预后情况,结合收集的资料进行单因素和多因素生存分析。结果 27例pPCL患者中位发病年龄为58(29~82)岁,男13例(48.1%)。单因素生存分析结果显示,年龄、是否化疗、外周血中浆细胞(PBPCs)比例、CD27表达、血钙>2.65 mmol/L、β2-MG水平影响pPCL患者预后(P < 0.05);多因素生存分析显示,是否接受化疗、PBPCs比例、CD27表达、血钙>2.65 mmol/L独立影响患者的总生存(P < 0.05)。结论 是否接受化疗、PBPCs、CD27表达、血钙>2.65 mmol/L独立影响患者的总生存,即提示初诊时患者未接受化疗、PBPCs水平越高、伴有CD27表达、血钙>2.65 mmol/L,患者的疾病进展和死亡的风险越高。Abstract: Objective To explore the clinical features and prognosis of patients with primary plasma cell leukemia(pPCL).Methods The pPCL patients who visited the First Affiliated Hospital of Zhengzhou University from May 2018 to May 2022 were selected, and the clinical characteristics, cellular immunophenotype, FISH detection, NGS gene detection, treatment and prognosis of the patients were collected, and univariate and multi-factor survival analysis was carried out based on the collected data.Results The median age of onset was 58 years in 27 patients with pPCL and 13 cases (48.1%) were male. The results of univariate survival analysis showed that age, whether to receive chemotherapy, the proportion of PBPCs, the expression of CD27, serum calcium>2.65 mmol/L, β2-MG affected the prognosis of patients with pPCL(P < 0.05). Multivariate survival analysis showed that only whether to receive chemotherapy, the proportion of PBPCs, the expression of CD27 and serum calcium>2.65 mmol/L independently affected the overall survival of patients(P < 0.05).Conclusion Whether to receive chemotherapy, the proportion of PBPCs, the expression of CD27 and serum calcium>2.65 mmol/L independently affect the patient's overall survival. That is, when the primary-care patient does not receive chemotherapy, the higher the level of PBPCs, accompanied by CD27 expression and serum calcium>2.65 mmol/L, the higher risk of disease progression and death.
-
Key words:
- primary plasma cell leukemia /
- clinical features /
- immunophenotype /
- cytogenetics /
- treatment /
- prognosis
-

-
表 1 27例pPCL患者的实验室指标
指标 数值 年龄/岁 58.7±13.2 BMPCs/% 60.5±18.0 FCM/% 54.7±21.2 HB/(g/L) 75.0±16.8 PLT/(×109/L) 66.9±33.9 PBPCs/% 33.0(20.0~86.0) WBC/(×109/L) 12.9(4.5~86.0) 血钙/(mmol/L) 2.6(2.0~4.8) Scr/(μmol/L) 132.0(38.0~659.0) GLO/(g/L) 52.9(10.7~135.6) ALB/(g/L) 36.5(18.4~99.2) β2-MG/(mg/L) 12.5(2.6~59.4) LDH/(U/L) 266.0(11.0~1 072.0) 表 2 27例pPCL患者的M蛋白类型
一般指标 例数(n=27) 比例/% M蛋白分型 IgG 13 48.1 IgA 4 14.8 单纯轻链型 9 33.3 单纯κ 4 14.8 单纯λ 5 18.5 不分泌型 1 3.7 轻链分型 κ 14 51.9 λ 12 44.4 表 3 27例pPCL患者的免疫表型
类型 高表达例数 占比/% 类型 高表达例数 占比/% CD138 25 92.6 CD117 3 11.1 CD38 24 88.9 CD27 3 11.1 CD81 16 59.3 CD33 3 11.1 CD56 11 40.7 CD22 1 3.7 CD23 9 33.3 CD200 1 3.7 CD28 7 25.9 CD19 1 3.7 CD20 5 18.5 CD71 1 3.7 CD4 3 11.1 CD57 1 3.7 表 4 单因素和多因素Cox生存分析
因素 单因素分析 多因素分析 HR(95%CI) P HR(95%CI) P 是否化疗 0.11(0.03~0.37) < 0.001 0.08(0.01~0.56) 0.012 PBPCs 1.04(1.01~1.06) 0.005 1.06(1.02~1.11) 0.003 CD27 5.46(1.35~22.06) 0.017 13.00(1.68~100.84) 0.014 血钙>2.65 mmol/L 3.72(1.23~11.23) 0.020 5.41(1.05~27.72) 0.043 β2-MG 1.05(1.01~1.09) 0.020 1.03(0.98~1.08) 0.235 年龄 1.05(1.00~1.11) 0.041 1.07(0.99~1.15) 0.088 表中仅纳入单因素分析中P < 0.05的因素。 -
[1] 李群, 孙春艳, 胡豫. 原发性浆细胞白血病生物学的研究进展[J]. 中华血液学杂志, 2022, 43(7): 603-607. https://cdmd.cnki.com.cn/Article/CDMD-10183-1021097224.htm
[2] Gundesen MT, Lund T, Moeller HEH, et al. Plasma cell leukemia: definition, presentation, and treatment[J]. Curr Oncol Rep, 2019, 21(1): 8. doi: 10.1007/s11912-019-0754-x
[3] de Larrea CF, Kyle RA, Durie BM, et al. Plasma cell leukemia: consensus statement on diagnostic requirements, response criteria and treatment recommendations by the International Myeloma Working Group[J]. Leukemia, 2013, 27(4): 780-791. doi: 10.1038/leu.2012.336
[4] Fernández de Larrea C, Kyle R, Rosiñol L, et al. Primary plasma cell leukemia: consensus definition by the International Myeloma Working Group according to peripheral blood plasma cell percentage[J]. Blood Cancer J, 2021, 11: 192. doi: 10.1038/s41408-021-00587-0
[5] Zhang DF, Huang JC, Zhang WY, et al. Young female patients with multiple myeloma have low occurrence of osteolytic lesion[J]. Bone, 2018, 110: 21-28. doi: 10.1016/j.bone.2018.01.021
[6] Kang SJ, Kishimoto T. Interplay between interleukin-6 signaling and the vascular endothelium in cytokine storms[J]. Exp Mol Med, 2021, 53(7): 1116-1123. doi: 10.1038/s12276-021-00649-0
[7] Guo RQ, Hu FX, Weng QT, et al. Guiding T lymphopoiesis from pluripotent stem cells by defined transcription factors[J]. Cell Res, 2020, 30(1): 21-33. doi: 10.1038/s41422-019-0251-7
[8] Rojas EA, Gutiérrez NC. Genomics of plasma cell leukemia[J]. Cancers, 2022, 14(6): 1594. doi: 10.3390/cancers14061594
[9] 王权钢, 白波, 马梁明, 等. 初诊多发性骨髓瘤患者CD56表达与以硼替佐米联合来那度胺为基础方案诱导治疗疗效的临床研究[J]. 临床血液学杂志, 2022, 35(11): 821-825. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2022.11.014
[10] Bezdekova R, Jelinek T, Kralova R, et al. Necessity of flow cytometry assessment of circulating plasma cells and its connection with clinical characteristics of primary and secondary plasma cell leukaemia[J]. Br J Haematol, 2021, 195(1): 95-107. doi: 10.1111/bjh.17713
[11] Moreau P, Robillard N, Jégo G, et al. Lack of CD27 in myeloma delineates different presentation and outcome[J]. Br J Haematol, 2006, 132(2): 168-170. doi: 10.1111/j.1365-2141.2005.05849.x
[12] Bezdekova R, Jelinek T, Kralova R, et al. Necessity of flow cytometry assessment of circulating plasma cells and its connection with clinical characteristics of primary and secondary plasma cell leukaemia[J]. Br J Haematol, 2021, 195: 95-107. doi: 10.1111/bjh.17713
[13] Pellat-Deceunynck C, Barillé S, Jego G, et al. The absence of CD56(NCAM)on malignant plasma cells is a hallmark of plasma cell leukemia and of a special subset of multiple myeloma[J]. Leukemia, 1998, 12(12): 1977-1982. doi: 10.1038/sj.leu.2401211
[14] Chen F, Hu YP, Wang XH, et al. Expression of CD81 and CD117 in plasma cell myeloma and the relationship to prognosis[J]. Cancer Med, 2018, 7(12): 5920-5927. doi: 10.1002/cam4.1840
[15] Mosca L, Musto P, Todoerti K, et al. Genome-wide analysis of primary plasma cell leukemia identifies recurrent imbalances associated with changes in transcriptional profiles[J]. Am J Hematol, 2013, 88(1): 16-23. doi: 10.1002/ajh.23339
[16] Gowin K, Skerget S, Keats JJ, et al. Plasma cell leukemia: a review of the molecular classification, diagnosis, and evidenced-based treatment[J]. Leuk Res, 2021, 111: 106687. doi: 10.1016/j.leukres.2021.106687
[17] Cifola I, Lionetti M, Pinatel E, et al. Whole-exome sequencing of primary plasma cell leukemia discloses heterogeneous mutational patterns[J]. Oncotarget, 2015, 6(19): 17543-17558. doi: 10.18632/oncotarget.4028
[18] Schinke C, Boyle EM, Ashby C, et al. Genomic analysis of primary plasma cell leukemia reveals complex structural alterations and high-risk mutational patterns[J]. Blood Cancer J, 2020, 10(6): 70. doi: 10.1038/s41408-020-0336-z
[19] Kryukov F, Dementyeva E, Kubiczkova L, et al. Cell cycle genes co-expression in multiple myeloma and plasma cell leukemia[J]. Genomics, 2013, 102(4): 243-249. doi: 10.1016/j.ygeno.2013.06.007
[20] Chang H, Qi XY, Yeung J, et al. Genetic aberrations including chromosome 1 abnormalities and clinical features of plasma cell leukemia[J]. Leuk Res, 2009, 33(2): 259-262. doi: 10.1016/j.leukres.2008.06.027
[21] Jung SH, Lee JJ. Update on primary plasma cell leukemia[J]. Blood Res, 2022, 57(S1): 62-66. doi: 10.5045/br.2022.2022033
[22] Visram A, Suska A, Jurczyszyn A, et al. Practical management and assessment of primary plasma cell leukemia in the novel agent era[J]. Cancer Treat Res Commun, 2021, 28: 100414. doi: 10.1016/j.ctarc.2021.100414
[23] 杨玉, 林彩芹, 李春雨, 等. 1q21扩增对于初治多发性骨髓瘤预后影响的异质性分析[J]. 临床血液学杂志, 2021, 34(9): 628-635. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202109006.htm
[24] Papadhimitriou SI, Terpos E, Liapis K, et al. The cytogenetic profile of primary and secondary plasma cell leukemia: etiopathogenetic perspectives, prognostic impact and clinical relevance to newly diagnosed multiple myeloma with differential circulating clonal plasma cells[J]. Biomedicines, 2022, 10(2): 209. doi: 10.3390/biomedicines10020209
[25] Gavriatopoulou M, Musto P, Caers J, et al. European myeloma network recommendations on diagnosis and management of patients with rare plasma cell dyscrasias[J]. Leukemia, 2018, 32(9): 1883-1898. doi: 10.1038/s41375-018-0209-7
[26] Ge XY, Meng WH, Wang WB, et al. Causes of death in primary plasma cell leukemia differ from multiple myeloma: a STROBE-compliant descriptive study based on SEER database[J]. Medicine(Baltimore), 2022, 101(29): e29578.
[27] Zhang DF, Huang JC, Wang FF, et al. BMI1 regulates multiple myeloma-associated macrophage's pro-myeloma functions[J]. Cell Death Dis, 2021, 12(5): 495. doi: 10.1038/s41419-021-03748-y
[28] Jurczyszyn A, Radocha J, Davila J, et al. Prognostic indicators in primary plasma cell leukaemia: a multicentre retrospective study of 117 patients[J]. Br J Haematol, 2018, 180(6): 831-839. doi: 10.1111/bjh.15092
[29] Mina R, Joseph NS, Kaufman JL, et al. Survival outcomes of patients with primary plasma cell leukemia(pPCL)treated with novel agents[J]. Cancer, 2019, 125(3): 416-423. doi: 10.1002/cncr.31718
-




 下载:
下载: