Evaluation of the prognosis of patients with diffuse large B-cell lymphoma treated with R-CHOP by cachexia index
-
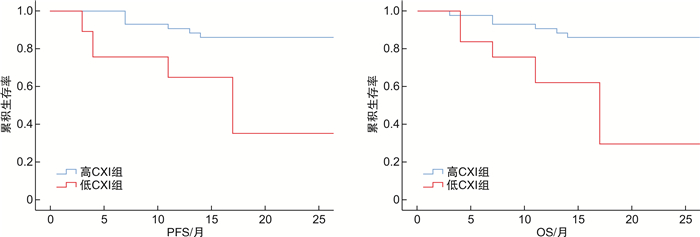
摘要: 目的 分析恶病质指数(cachexia index,CXI)对R-CHOP治疗的弥漫性大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL)患者预后的评价。方法 回顾性分析2020年1月—2022年1月接受R-CHOP治疗的DLBCL患者80例,收集患者相关资料并计算CXI值,根据CXI中位数将患者分为低CXI组和高CXI组,比较2组临床资料、治疗反应、无进展生存期(PFS)、总生存期(OS)和治疗相关毒性。结果 CXI中位数男性为42.61,女性为25.28,高CXI组43例,低CXI组37例。低CXI组年龄>60岁患者、ECOG PS 2~3分、B症状、Ann Arbor Ⅲ~Ⅳ级、LDH异常、IPI高中危和高危比例均高于高CXI组,差异有统计学意义(P<0.05)。低CXI组所有患者CR低于高CXI组,疾病进展例数高于高CXI组(P<0.05)。高CXI患者PFS和OS高于低CXI患者(P<0.05)。多变量分析表明,BMI<18.5、IPI高中危和高危以及低CXI是PFS和OS的独立预后指标(P<0.05)。高CXI组3~4级贫血、血小板减少和发热性中性粒细胞减少发生率,以及3级或以上的非血液毒性均低于低CXI组(P<0.05)。低CXI组早期治疗中断例数高于高CXI组(P<0.05)。结论 CXI是一种有效的癌症恶病质生物标志物,可以预测DLBCL患者的生存率、治疗反应和治疗相关毒性。
-
关键词:
- 恶病质指数 /
- 免疫化疗 /
- 弥漫性大B细胞淋巴瘤 /
- 预后
Abstract: Objective To analyze the evaluation of cachexia index(CXI) on the prognosis of patients with diffuse large B-cell lymphoma(DLBCL) treated with R-CHOP.Methods A retrospective analysis was conducted on 80 DLBCL patients treated with R-CHOP from January 2020 to January 2022. Patient data and calculate CXI values were collected. Patients were divided into low CXI group and high CXI group according to the median CXI. Clinical data, treatment response, progression-free survival(PFS), overall survival(OS) and treatment-related toxicity were compared between the two groups.Results The median CXI was 42.61 for males and 25.28 for females, with 43 cases in the high CXI group and 37 cases in the low CXI group. The low CXI group's proportion of patients over 60 years old, ECOG PS scores of 2-3, B-symptoms, Ann Arbor grades Ⅲ-Ⅳ, abnormal LDH and high, medium-high risk IPI were higher than the high CXI group, with statistically significant differences (P < 0.05).The CR of all patients in the low CXI group was lower than that in the high CXI group, and the number of cases with disease progression was higher than that in the high CXI group(P < 0.05). The PFS and OS of patients with high CXI were higher than those with low CXI(P < 0.05). Multivariate analysis showed that BMI < 18.5, high-intermediate risk and high risk IPI, and low CXI were independent prognostic indicators for PFS and OS(P < 0.05). The incidence of grade 3-4 anemia, thrombocytopenia and febrile neutropenia in the high CXI group were lower than those in the low CXI group, and the non-hematologic toxicity of grade 3 or above was lower than that in the low CXI group(P < 0.05). The number of cases with early treatment discontinuation in the low CXI group was higher than that in the high CXI group(P < 0.05).Conclusion CXI is an effective biomarker of cancer cachexia, which can predict the survival rate, treatment response and treatment-related toxicity of DLBCL patients.-
Key words:
- cachexia index /
- immunochemotherapy /
- diffuse large B-cell lymphoma /
- prognosis
-

-
表 1 2组一般资料比较
变量 高CXI组(n=43) 低CXI组(n=37) t/χ2 P 年龄/岁 62.49±8.17 73.64±9.48 5.651 <0.001 不同年龄段/例(%) 13.082 0.004 ≤40岁 5(11.63) 1(2.70) 41~60岁 16(37.21) 5(13.51) 61~74岁 17(39.53) 16(43.24) ≥75岁 5(11.63) 15(40.54) 性别(男/女)/例 24/19 21/16 0.007 0.932 ECOG PS(0~1/2~3)/例 35/8 17/20 10.985 0.001 B症状/例(%) 6(13.95) 12(32.43) 3.894 0.048 BMI 23.42±3.55 22.20±4.28 1.394 0.167 大包块/例(%) 9(20.93) 7(18.92) 0.050 0.823 Ann Arbor分期(Ⅰ~Ⅱ/Ⅲ~Ⅳ)/例 22/21 8/29 7.405 0.007 结外疾病/例(%) 26(60.47) 27(72.97) 1.392 0.238 LDH/例(%) 15.034 0.001 正常值 22(51.16) 6(16.22) >1倍~≤3倍 19(44.19) 20(54.05) >3倍 2(4.65) 11(29.73) IPI/例(%) 27.441 0.001 低危 6(13.95) 1(2.70) 低中危 20(46.51) 3(8.11) 高中危 13(30.23) 12(32.43) 高危 4(9.30) 21(56.76) 表 2 根据治疗依从性的完全缓解率
例(%) 变量 高CXI组(n=43) 低CXI组(n=37) χ2 P 所有患者CR 36/43(83.72) 17/37(45.95) 12.692 <0.001 无剂量调整患者CR 21/23(91.30) 4/8(50.00) 6.488 0.011 剂量调整患者CR 12/13(92.31) 6/9(66.67) 2.350 0.125 相对剂量强度≥75% 8/9(88.89) 6/7(85.71) 0.036 0.849 相对剂量强度<75% 4/4(100.00) 0/2(0) 6.000 0.014 早期停止治疗患者CR 1/4(25.00) 2/16(12.5) 0.392 0.531 疾病稳定 3/43(6.98) 6/37(16.22) 1.700 0.192 疾病进展 4/43(9.30) 14/37(37.84) 9.287 0.002 表 3 PFS和OS的多因素分析
变量 单因素 多因素 HR 95%CI P HR 95%CI P PFS 性别女 0.813 0.563~1.175 0.271 - - - B症状 2.263 1.513~3.385 <0.001 1.277 0.827~1.971 0.269 BMI<18.5 1.956 1.023~3.739 0.042 2.291 1.153~4.549 0.018 大包块疾病 0.776 0.470~1.282 0.323 - - - IPI高中危 4.483 2.722~7.382 <0.001 3.619 2.149~6.094 <0.001 IPI高危 9.477 5.616~15.995 <0.001 7.432 4.188~13.188 <0.001 低CXI 4.053 2.671~6.149 <0.001 1.904 1.189~3.051 0.007 OS 性别女 0.778 0.528~1.148 0.207 - - - B症状 2.200 1.443~3.356 <0.001 1.246 0.792~1.958 0.341 BMI<18.5 1.965 0.993~3.890 0.052 2.463 1.197~5.072 0.014 大包块疾病 0.760 0.447~1.293 0.311 - - - IPI高中危 4.350 2.585~7.320 <0.001 3.490 2.026~6.011 <0.001 IPI高危 9.702 5.603~16.799 <0.001 7.387 4.026~13.554 <0.001 低CXI 4.403 2.837~6.835 <0.001 2.103 1.278~3.460 0.003 表 4 2组治疗相关毒性比较
例(%) 变量 高CXI组(n=43) 低CXI组(n=37) χ2 P 血液毒性≥3级 贫血 5(11.63) 11(29.73) 4.073 0.044 血小板减少 9(20.93) 16(43.24) 4.609 0.032 嗜中性白血球减少症 32(74.42) 30(81.08) 0.506 0.477 发热性中性粒细胞减少症 8(18.60) 15(40.54) 4.672 0.031 非血液毒性≥3级 13(30.23) 20(54.05) 4.657 0.031 治疗相关死亡率 1(2.33) 2(5.41) 0.353 0.552 早期治疗中断 5(11.63) 15(40.54) 8.867 0.003 -
[1] 许彭鹏, 赵维莅. 中国临床肿瘤学会淋巴瘤诊疗指南解读之弥漫性大B细胞淋巴瘤的规范治疗[J]. 华西医学, 2019, 34(4): 351-354. https://www.cnki.com.cn/Article/CJFDTOTAL-HXYX201904001.htm
[2] 冯要须, 苏丽萍. 国际预后指数修订国际预后指数改良国际预后指数及西班牙淋巴瘤组/自体骨髓移植国际预后指数对弥漫性大B细胞淋巴瘤的预后评估价值[J]. 中华肿瘤杂志, 2020, 42(11): 949-954.
[3] Burkart M, Schieber M, Basu S, et al. Evaluation of the impact of cachexia on clinical outcomes in aggressive lymphoma[J]. Br J Haematol, 2019, 186(1): 45-53. doi: 10.1111/bjh.15889
[4] Matsunaga T, Deto T, Yamada T, et al. Limitations of the L3 skeletal muscle index and the Asian Working Group for Sarcopenia 2019 consensus diagnostic criteria for sarcopenia evaluation in a case of diffuse large B-cell lymphoma[J]. Clin Case Rep, 2022, 10(6): e5949. doi: 10.1002/ccr3.5949
[5] Jafri SH, Previgliano C, Khandelwal K, et al. Cachexia index in advanced non-small-cell lung cancer patients[J]. Clin Med Insights Oncol, 2015, 9: 87-93.
[6] Go SI, Park MJ, Park S, et al. Cachexia index as a potential biomarker for cancer Cachexia and a prognostic indicator in diffuse large B-cell lymphoma[J]. J Cachexia Sarcopenia Muscle, 2021, 12(6): 2211-2219. doi: 10.1002/jcsm.12837
[7] 谢萌, 张青青, 郭瑞昕, 等. 头颈部弥漫大B细胞淋巴瘤的临床特征分析[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(1): 1-7. doi: 10.13201/j.issn.2096-7993.2022.01.001
[8] 肖远喆, 张清媛. 弥漫性大B细胞淋巴瘤免疫治疗进展[J]. 现代肿瘤医学, 2022, 30(18): 3441-3444. doi: 10.3969/j.issn.1672-4992.2022.18.041
[9] 熊婕妤, 汪君娣, 罗明青, 等. 不同化疗方案治疗弥漫大B细胞淋巴瘤患者的疗效及不良反应分析[J]. 国际输血及血液学杂志, 2021, 44(5): 415-423.
[10] 陈文馨, 孙圣荣. 癌症恶病质相关肌肉萎缩发病机制的研究进展[J]. 中华实用诊断与治疗杂志, 2022, 36(1): 106-108. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202201025.htm
[11] 朱垲枫, 胡抢, 杨家立, 等. 恶病质评估在胃恶性肿瘤治疗中的意义[J]. 浙江临床医学, 2023, 25(2): 307-309.
[12] 王杰敏, 贾维慧, 厉丹阳, 等. 肺癌患者恶病质的药物治疗与营养支持研究进展[J]. 中国肺癌杂志, 2022, 25(6): 420-424. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ202206004.htm
[13] Go SI, Park MJ, Lee GW. Clinical significance of the cachexia index in patients with small cell lung cancer[J]. BMC Cancer, 2021, 21(1): 1-9.
[14] Jo H, Yoshida T, Horinouchi H, et al. Prognostic significance of cachexia in advanced non-small cell lung cancer patients treated with pembrolizumab[J]. Cancer Immunol Immunother, 2022, 71(2): 387-398.
[15] 汪玉芳, 柯金勇, 柯善栋. 原发性胃弥漫大B细胞淋巴瘤患者的生存情况及其影响因素分析[J]. 癌症进展, 2018, 16(8): 1020-1023. https://www.cnki.com.cn/Article/CJFDTOTAL-AZJZ201808027.htm
[16] Iltar U, Sözel H, Sözel YK, et al. Prognostic impact of the psoas muscle index, a parameter of sarcopenia, in patients with diffuse large B-cell lymphoma treated with rituximab-based chemoimmunotherapy[J]. Leuk Lymphoma, 2021, 62(5): 1098-1106.
[17] Wei YQ, Wei XL, Huang WM, et al. Albumin improves stratification in the low IPI risk patients with diffuse large B-cell lymphoma[J]. Int J Hematol, 2020, 111(5): 681-685.
[18] Wei XL, Zheng JX, Zhang ZW, et al. Consecutive hypoalbuminemia predicts inferior outcome in patients with diffuse large B-cell lymphoma[J]. Front Oncol, 2020, 10: 610681.
[19] 朱成斌, 蔡春莲. 血常规指标对初诊多发性骨髓瘤临床分期和预后预测价值的研究[J]. 临床血液学杂志, 2021, 34(10): 723-727. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2021.10.010
[20] 林樟萍, 陆喆, 王敏, 等. 外周血NLR、LMR对睾丸原发性弥漫性大B细胞淋巴瘤患者预后的预测价值[J]. 标记免疫分析与临床, 2021, 28(3): 414-422. https://www.cnki.com.cn/Article/CJFDTOTAL-BJMY202103013.htm
[21] Zhao J, Wang M, Huang R, et al. Effects of CALM intervention on neutrophil-to-lymphocyte ratio(NLR), fear of cancer recurrence and quality of life in patients with lung cancer[J]. Support Care Cancer, 2023, 31(7): 447.
[22] Karmali R, Alrifai T, Fughhi IAM, et al. Impact of cachexia on outcomes in aggressive lymphomas[J]. Ann Hematol, 2017, 96(6): 951-956.
[23] Martin A, Freyssenet D. Phenotypic features of cancer cachexia-related loss of skeletal muscle mass and function: lessons from human and animal studies[J]. J Cachexia Sarcopenia Muscle, 2021, 12(2): 252-273.
[24] Sadeghi M, Keshavarz-Fathi M, Baracos V, et al. Cancer cachexia: diagnosis, assessment, and treatment[J]. Crit Rev Oncol Hematol, 2018, 127: 91-104.
[25] Freudenberger DC, Vudatha V, Riner AN, et al. A Review of the Clinical Implications of Cachexia, Sarcopenia, and BMI in Patients with Peritoneal Carcinomatosis Receiving Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy[J]. Cancers(Basel), 2022, 14(12): 2853.
-




 下载:
下载: