Clinical characteristics and prognosis of adult lymphoma-associated hemophagocytic lymphohistiocytosis
-
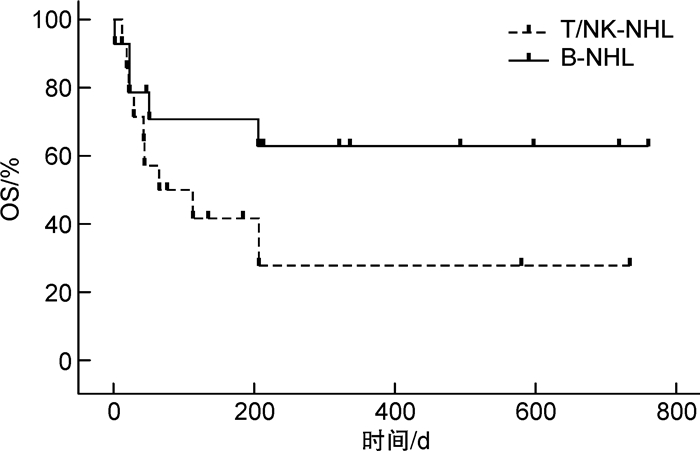
摘要: 目的 分析淋巴瘤相关噬血细胞综合征(lymphoma-associated hemophagocytic lymphohistiocytosis,LA-HLH)的临床特征,探讨不同治疗方案对预后的影响。方法 回顾性分析2021年7月至2023年7月在我院血液科确诊的32例LA-HLH患者的临床资料,比较不同淋巴瘤病理亚型LA-HLH患者的临床特征和预后差异。结果 纳入的32例患者均符合HLH-2004的诊断标准,经组织病理确诊为淋巴瘤且年龄大于18岁。①临床特征:32例患者中位年龄58岁(范围:18~82岁),17例(53.1%)为男性;中位诊断时间11.5 d(范围:2~56 d);病理类型分别为B细胞非霍奇金淋巴瘤(B-NHL)15例、T/NK细胞非霍奇金淋巴瘤(T/NK-NHL)15例和经典霍奇金淋巴瘤2例。所有患者均有发热和铁蛋白升高;发生比例比较高的其他临床特征包括乳酸脱氢酶升高(96.9%)、淋巴细胞减少(90.6%)、≥2系的血细胞减少(87.5%)、脾大(84.4%)、低蛋白血症(84.4%)、sCD25水平升高(75.0%)、肝功能不全(68.8%)、噬血现象(65.6%)和黄疸(62.5%)。32例患者中位Hscore评分为250.5(范围:178~376),均高于截断值169。②32例患者中位总生存时间(OS)207 d。与T/NK-NHL患者的中位OS 89 d比较,B-NHL患者的中位OS(未达到)有延长的趋势,但差异无统计学意义(P>0.05)。在接受HLH诱导治疗的患者中,接受含依托泊苷方案治疗的患者较仅接受地塞米松治疗的患者中位OS明显延长(335 d vs 7 d,P < 0.01)。此外,接受淋巴瘤化疗方案的患者较仅接受HLH诱导治疗方案的患者中位OS明显延长(未达到vs 23 d,P < 0.01)。③15例合并EBV感染的LA-HLH患者均为EBV相关淋巴瘤,其中T/NK细胞淋巴瘤的EBV感染率为86.7%,B细胞淋巴瘤的EBV感染率为6.7%。结论 在诱发HLH的淋巴瘤类型中,B-NHL和T/NK-NHL所占的比例相当,远高于霍奇金淋巴瘤,最常见诱发HLH的3种淋巴瘤类型分别为弥漫大B细胞淋巴瘤、结外NK/T细胞淋巴瘤和血管免疫母细胞淋巴瘤。应用Hscore评分或能帮助临床早期识别LA-HLH患者。基于依托泊苷的HLH诱导治疗序贯多药联合化疗治疗淋巴瘤是LA-HLH治疗的合理选择。Abstract: Objective To examine the clinical characteristics of lymphoma-associated hemophagocytic lymphohistiocytosis(LA-HLH) and investigate the effects of various treatment strategies on the prognosis of patients.Methods The clinical data of 32 LA-HLH patients diagnosed from July 2021 to July 2023 were retrospectively analyzed. The clinical characteristics and prognosis differences among patients with different lymphoma pathological subtypes were compared.Results All 32 patients met the HLH-2004 criteria, were pathologically diagnosed as malignant lymphomas, and were older than 18 years. The clinical characteristics were as follows: ①The median age of 32 patients was 58 years(range: 18-82 years), with 17 cases(53.1%) were male. The median diagnostic time was 11.5 days(range: 2-56 days). The pathological types were B-cell non-Hodgkin's lymphoma(B-NHL)(15 cases), T/NK-cell non-Hodgkin's lymphoma(T/NK-NHL)(15 cases), and classic Hodgkin's lymphoma(2 cases). All patients had fever and increased ferritin. The other common clinical manifestations included elevated lactic dehydrogenase(96.9%), lymphocytopenia(90.6%), cytopenias affecting ≥ 2 of 3 lineages in the peripheral blood(87.5%), splenomegaly(84.4%), hypoproteinemia(84.4%), elevated soluble CD25 level(75.0%), liver dysfunction(68.8%), hemophagocytosis(65.6%), and jaundice(62.5%). The median Hscore value of 32 patients was 250.5(range: 178-376), all of which were higher than the cut-off value of 169. ②The median overall survival(OS) of 32 patients was 207 days. Compared with the median OS of 89 days in the T/NK-NHL group, the median OS of the B-NHL group(not reached) showed a trend of prolongation, but there was no significant difference(P>0.05). Among the patients receiving HLH induction therapy, those receiving etoposide-containing regimen had a significantly longer median OS than those receiving dexamethasone alone(335 d vs 7 d, P < 0.01). In addition, patients receiving lymphoma chemotherapy regimen had a significantly longer median OS than those receiving HLH induction therapy only(not reached vs 23 d, P < 0.01). ③Among the 15 LA-HLH patients with concurrent EBV infection, all were diagnosed as EBV-related lymphomas, and the EBV infection rate was 86.7% in T/NK cell lymphomas and 6.7% in B cell lymphomas.Conclusion The proportion of B-NHL and T/NK-NHL is relatively equal in LA-HLH, and significantly higher than that of Hodgkin's lymphoma. The three most common types of lymphomas that induce HLH are diffuse large B-cell lymphoma, extranodal T/NK-cell lymphoma, and angio-immunoblastic T-cell lymphoma. The application of the HScore may aid in the early clinical identification of patients with LA-HLH. An etoposide-containing HLH induction therapy followed by multidrug combined chemotherapy is a reasonable choice for the treatment of LA-HLH.
-
Key words:
- hemophagocytic lymphohistiocytosis /
- lymphoma /
- treatment /
- prognosis
-

-
表 1 LA-HLH患者感染的淋巴细胞亚群
淋巴细胞亚群 检测结果(EBV-DNA拷贝每100万个细胞) EBV+
DLBCLcHL ENKTL
1#ENKTL
2#ENKTL
3#AITL AITL伴EBV+
DLBCLCD3+CD4+细胞 CD4+T细胞 未检出 未检出 未检出 未检出 未检出 7.8×102 4.3×104 CD3+CD8+细胞 CD8+T细胞 未检出 未检出 未检出 2.3×104 1.8×104 9.9×102 6.6×104 CD3-CD19+细胞 B细胞 2.2×106 1.8×104 未检出 未检出 未检出 1.2×105 1.3×106 CD56+细胞 NK/NKT细胞 7.5×104 1.7×104 2.7×103 5.6×105 5.4×104 2.0×102 5.0×104 -
[1] Henter JI, Horne A, Aricó M, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis[J]. Pediatr Blood Cancer, 2007, 48(2): 124-131. doi: 10.1002/pbc.21039
[2] Zhang R, Cui T, He L, et al. A study on early death prognosis model in adult patients with secondary hemophagocytic lymphohistiocytosis[J]. J Healthc Eng, 2022, 2022: 6704859.
[3] Brito-Zerón P, Kostov B, Moral-Moral P, et al. Prognostic factors of death in 151 adults with hemophagocytic syndrome: etiopathogenically driven analysis[J]. Mayo Clin Proc Innov Qual Outcomes, 2018, 2(3): 267-276. doi: 10.1016/j.mayocpiqo.2018.06.006
[4] Jumic S, Nand S. Hemophagocytic lymphohistiocytosis in adults: associated diagnoses and outcomes, a ten-year experience at a single institution[J]. J Hematol, 2019, 8(4): 149-154. doi: 10.14740/jh592
[5] Abdelhay A, Mahmoud AA, Al Ali O, et al. Epidemiology, characteristics, and outcomes of adult haemophagocytic lymphohistiocytosis in the USA, 2006-19: a national, retrospective cohort study[J]. E Clinical Medicine, 2023, 62: 102143.
[6] Ramos-Casals M, Brito-Zerón P, López-Guillermo A, et al. Adult haemophagocytic syndrome[J]. Lancet, 2014, 383(9927): 1503-1516. doi: 10.1016/S0140-6736(13)61048-X
[7] Ishii E, Ohga S, Imashuku S, et al. Nationwide survey of hemophagocytic lympho-histiocytosis in Japan[J]. Int J Hematol, 2007, 86(1): 58-65. doi: 10.1532/IJH97.07012
[8] Sano H, Kobayashi R, Tanaka J, et al. Risk factor analysis of non-Hodgkin lymphoma associated haemophagocytic syndromes: a multicentre study[J]. Br J Haematol, 2014, 165(6): 786-792. doi: 10.1111/bjh.12823
[9] Lehmberg K, Nichols KE, Henter JI, et al. Study Group on Hemophagocytic Lympho-histiocytosis Subtypes of the Histiocyte Society. Consensus recommendations for the diagnosis and management of hemophagocytic lymphohistiocytosis-associated with malignancies[J]. Haematologica, 2015, 100(8): 997-1004.
[10] Veerakul G, Sanpakit K, Tanphaichitr VS, et al. Secondary hemophagocytic lymphohistiocytosis in children: an analysis of etiology and outcome[J]. J Med Assoc Thai, 2002, 85 Suppl 2: S530.
[11] Lorenz F, Klimkowska M, Pawłowicz E, et al. Clinical characteristics, therapy response, and outcome of 51 adult patients with hematological malignancy-associated hemophagocytic lymphohistiocytosis: a single institution experience[J]. Leuk Lymphoma, 2018, 59(8): 1840-1850. doi: 10.1080/10428194.2017.1403018
[12] Parikh SA, Kapoor P, Letendre L, et al. Prognostic factors and outcomes of adults with hemophagocytic lymphohistiocytosis[J]. Mayo Clin Proc, 2014, 89: 484-492. doi: 10.1016/j.mayocp.2013.12.012
[13] Tamamyan GN, Kantarjian HM, Ning J, et al. Malignancy-associated hemophagocytic lymphohistiocytosis in adults: Relation to hemophagocytosis, characteristics, and outcomes[J]. Cancer, 2016, 122(18): 2857-2866. doi: 10.1002/cncr.30084
[14] Henter JI, Elinder G, Söder O, et al. Incidence in Sweden and clinical features of familial hemophagocytic lymphohistiocytosis[J]. Acta Paediatr Scand, 1991, 80(4): 428-435. doi: 10.1111/j.1651-2227.1991.tb11878.x
[15] Yu JT, Wang CY, Yang Y, et al. Lymphoma-associated hemophagocytic lymphohistiocytosis: experience in adults from a single institution[J]. Ann Hematol, 2013, 92(11): 1529-1536. doi: 10.1007/s00277-013-1784-3
[16] Ménard F, Besson C, Rincé P, et al. Hodgkin lymphoma-associated hemophagocytic syndrome: a disorder strongly correlated with Epstein-Barr virus[J]. Clin Infect Dis, 2008, 47(4): 531-534. doi: 10.1086/590152
[17] 刘艺, 郭涛. 血液系统肿瘤治疗相关噬血细胞综合征的诊疗进展[J]. 临床血液学杂志, 2022, 35(1): 16-20. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2022.01.004
[18] Shimazaki C, Inaba T, Nakagawa M. B-cell lymphoma-associated hemophagocytic syndrome[J]. Leuk Lymphoma, 2000, 38(1-2): 121-130. doi: 10.3109/10428190009060325
-




 下载:
下载:

