Exploration on role of peripheral blood FAR and Lp-PLA2 in thrombotic susceptibility of patients with idiopathic membranous nephropathy
-
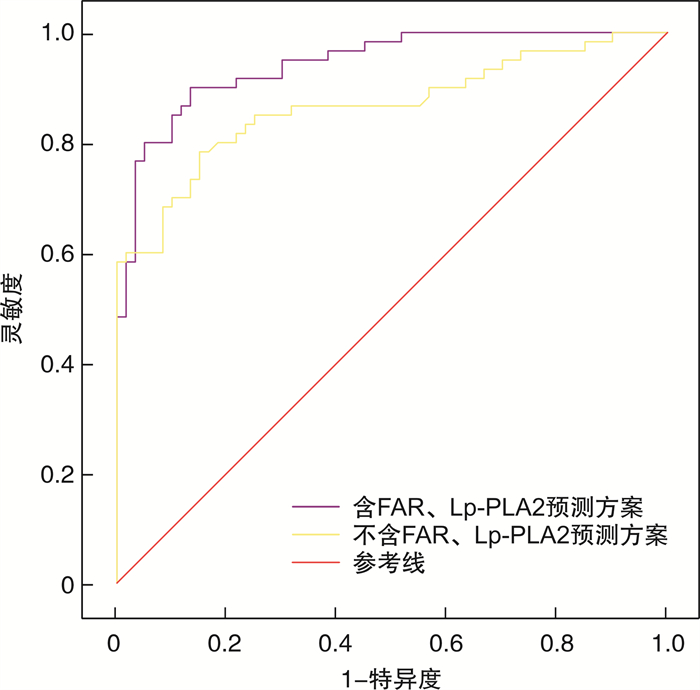
摘要: 目的 探讨特发性膜性肾病(idiopathic membranous nephropathy,IMN)患者外周血纤维蛋白原/白蛋白比值(fibrinogen/albumin ratio,FAR)、脂蛋白相关磷脂酶A2(lipoprotein-associated phospholipase A2,Lp-PLA2)水平,分析其对IMN并发血栓的预测价值。方法 选取2020年1月—2023年1月医院收治的60例IMN并发血栓患者作为研究组,另选同期60例IMN无血栓患者作为对照组。比较2组一般资料、24 h尿蛋白定量(24 h Upro)、血脂指标(甘油三酯、总胆固醇、高密度脂蛋白胆固醇、低密度脂蛋白胆固醇)、凝血功能指标[凝血酶时间(TT)、凝血酶原时间(PT)、纤维蛋白原(FIB)、活化部分凝血酶原时间(APTT)]、外周血FAR、Lp-PLA2水平。logistic回归分析IMN并发血栓的影响因素。分析研究组外周血FAR、Lp-PLA2水平与IMN并发血栓影响因素的相关性。对比分析含与不含外周血FAR、Lp-PLA2预测方案对IMN并发血栓的预测价值。结果 2组IMN病程、病理分期、24 h Upro、外周血D-D、FIB、APTT、FAR、Lp-PLA2水平比较差异有统计学意义(P < 0.05);IMN病程、病理分期、24 h Upro、外周血D-D、FIB、APTT、FAR、Lp-PLA2水平为IMN并发血栓的影响因素(P < 0.05);外周血FAR、Lp-PLA2联合预测IMN并发血栓的受试者工作特征曲线下面积(AUC)大于单项指标预测(P < 0.05);含FAR、Lp-PLA2预测方案对IMN并发血栓的预测效果较不含FAR、Lp-PLA2预测方案明显改善(P < 0.05)。结论 IMN并发血栓患者外周血FAR、Lp-PLA2水平升高,且与血栓易感性密切相关,含外周血FAR、Lp-PLA2预测方案对IMN并发血栓具有一定预测价值。
-
关键词:
- 特发性膜性肾病 /
- 纤维蛋白原 /
- 白蛋白 /
- 脂蛋白相关磷脂酶A2
Abstract: Objective To investigate the levels of fibrinogen/albumin ratio(FAR) and lipoprotein-associated phospholipase A2(Lp-PLA2) in peripheral blood of patients with idiopathic membranous nephropathy(IMN), and analyze their predictive value for thrombosis in IMN.Methods Sixty patients with IMN complicated by thrombosis admitted to the hospital from January 2020 to January 2023 were selected as the study group, and another 60 patients with IMN without thrombosis in the same period were selected as the control group. The general data, 24 h urine protein quantification(24 h Upro), lipid indexes(triglycerides, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol), coagulation indexes(D-dimer[D-D], prothrombin time[TT], prothrombin time[PT], fibrinogen[FIB]) were compared between the two groups. Logistic regression was used to analyze the factors influencing the complication of thrombosis in IMN. The correlation between peripheral blood FAR and Lp-PLA2 levels in the study group and the factors affecting IMN complicating thrombosis was analyzed. The predictive value of the prediction scheme with and without peripheral blood FAR and Lp-PLA2 for IMN complicating thrombosis was compared.Results There were significant differences in IMN course, pathological stage, 24 h Upro, peripheral blood D-D, FIB, APTT, FAR and Lp-PLA2 levels between the two groups(P < 0.05). The course of IMN disease, pathological stage, 24 h Upro, peripheral blood D-D, FIB, APTT, FAR and Lp-PLA2 levels were the influencing factors of IMN complicated with thrombus(P < 0.05). The AUC of peripheral blood FAR and Lp-PLA2 combined predicted thrombus of IMN was greater than that of single index(P < 0.05). The prediction effect of FAR and Lp-PLA2 prediction schemes on thrombosis complicated by IMN was significantly improved compared with that without FAR and Lp-PLA2 prediction schemes(P < 0.05).Conclusion The levels of FAR and Lp-PLA2 in peripheral blood of patients with IMN complicated with thrombus were increased, which was closely related to the susceptibility to thrombus. The prediction scheme including peripheral blood FAR and Lp-PLA2 might have a certain value in predicting thrombus complicated with IMN. -

-
表 1 2组一般资料及实验室指标比较
项目 研究组(n=60) 对照组(n=60) t/χ2/u P 性别/例(%) 0.556 0.456 男 38(63.33) 34(56.67) 女 22(36.67) 26(43.33) 年龄/岁 46.12±8.41 43.79±8.25 1.532 0.128 IMN病程/年 4.11±0.93 2.86±0.77 8.019 <0.001 BMI 23.75±2.16 23.21±1.94 1.441 0.152 病理分期/例(%) 8.124 0.017 Ⅰ期 20(33.33) 33(55.00) Ⅱ期 22(36.67) 20(33.33) Ⅲ期 18(30.00) 7(11.67) 饮酒史/例(%) 0.519 0.471 有 12(20.00) 9(15.00) 无 48(80.00) 51(85.00) 吸烟史/例(%) 0.786 0.375 有 15(25.00) 11(18.33) 无 45(75.00) 49(81.67) 高血压/例(%) 0.891 0.345 有 13(21.67) 9(15.00) 无 47(78.33) 51(85.00) 糖尿病/例(%) 0.563 0.453 有 11(18.33) 8(13.33) 无 49(81.67) 52(86.67) 激素治疗/例(%) 0.686 0.408 是 9(15.00) 6(10.00) 否 51(85.00) 54(90.00) 24 h Upro/(g/24 h) 5.63±1.35 3.41±0.82 10.887 <0.001 TG/(mmol/L) 3.03±0.85 2.81±0.79 1.469 0.145 TC/(mmol/L) 9.72±2.86 9.25±2.49 0.960 0.339 HDL-C/(mmol/L) 1.47±0.39 1.52±0.43 0.667 0.506 LDL-C/(mmol/L) 5.26±1.18 4.87±1.04 1.921 0.057 D-D/(μg/mL) 0.61±0.07 0.30±0.04 29.784 <0.001 TT/s 30.17±5.26 29.40±4.93 0.827 0.410 PT/s 12.85±0.91 12.56±0.88 1.774 0.079 FIB/(g/L) 7.15±1.94 4.62±1.25 8.492 <0.001 APTT/s 36.71±4.25 30.96±3.88 7.740 <0.001 FAR 1.12±0.21 0.95±0.17 4.874 <0.001 Lp-PLA2/(U/L) 663.91±95.42 71.02±16.45 47.430 <0.001 表 2 赋值方法
变量 赋值 因变量 并发血栓 否=0,是=1 自变量 IMN病程 连续变量,原值代入 病理分期 Ⅰ期=1,Ⅱ期=2,Ⅲ期=3 24 h Upro 连续变量,原值代入 D-D 连续变量,原值代入 FIB 连续变量,原值代入 APTT 连续变量,原值代入 FAR 连续变量,原值代入 Lp-PLA2 连续变量,原值代入 表 3 IMN并发血栓的影响因素分析
变量 β SE Wald χ2 OR 95%CI P 下限 上限 IMN病程 1.377 0.425 10.499 3.963 1.241 12.657 < 0.001 病理分期 1.779 0.451 15.558 5.923 2.013 17.429 < 0.001 24 h Upro 1.618 0.429 14.230 5.045 1.684 15.112 < 0.001 D-D 1.538 0.433 12.619 4.656 1.507 14.385 < 0.001 FIB 1.475 0.426 11.991 4.372 1.446 13.217 < 0.001 APTT 1.561 0.398 15.387 4.765 1.513 15.004 < 0.001 FAR 1.879 0.418 20.215 6.549 2.216 19.357 < 0.001 Lp-PLA2 1.827 0.426 18.394 6.215 2.108 18.326 < 0.001 表 4 FAR、Lp-PLA2与IMN并发血栓影响因素的相关性
指标 IMN病程 病理分期 24 h Upro D-D FIB APTT FAR r 0.215 0.208 0.119 0.224 0.196 0.209 P 0.139 0.145 0.412 0.120 0.152 0.142 Lp-PLA2 r 0.228 0.235 0.131 0.233 0.210 0.218 P 0.117 0.126 0.357 0.105 0.131 0.129 表 5 FAR、Lp-PLA2预测IMN并发血栓的价值
指标 AUC 95%CI 截断值 敏感度 特异度 P FAR 0.717 0.628~0.796 1.05 0.716 7 0.666 7 < 0.001 Lp-PLA2 0.726 0.637~0.804 420.15 U/L 0.751 2 0.667 3 < 0.001 联合预测 0.855 0.780~0.913 - 0.733 5 0.866 9 < 0.001 表 6 含与不含FAR、Lp-PLA2预测方案对IMN并发血栓的预测价值比较
成对对比 AUC差异(95%CI) NRI(95%CI) IDI(95%CI) 含FAR、Lp-PLA2预测方案vs不含FAR、Lp-PLA2预测方案 0.077(0.005~0.150) 0.864(0.226~1.157) 0.213(0.056~0.351) P 0.037 0.009 0.015 -
[1] Liu W, Gao C, Liu Z, et al. Idiopathic Membranous Nephropathy: Glomerular Pathological Pattern Caused by Extrarenal Immunity Activity[J]. Front Immunol, 2020, 11(1): 1846-1856.
[2] Zhu H, Xu L, Liu X, et al. Anti-PLA2R antibody measured by ELISA predicts the risk of vein thrombosis in patients with primary membranous nephropathy[J]. Ren Fail, 2022, 44(1): 594-600. doi: 10.1080/0886022X.2022.2057861
[3] Cremoni M, Brglez V, Perez S, et al. Th17-Immune Response in Patients With Membranous Nephropathy Is Associated With Thrombosis and Relapses[J]. Front Immunol, 2020, 11(1): 574997-575007.
[4] Roca N, Martinez C, Jatem E, et al. Activation of the acute inflammatory phase response in idiopathic nephrotic syndrome: association with clinicopathological phenotypes and with response to corticosteroids[J]. Clin Kidney J, 2021, 14(4): 1207-1215. doi: 10.1093/ckj/sfaa247
[5] Luo B, Sun M, Huo X, et al. Two new inflammatory markers related to the CURB-65 score for disease severity in patients with community-acquired pneumonia: The hypersensitive C-reactive protein to albumin ratio and fibrinogen to albumin ratio[J]. Open Life Sci, 2021, 16(1): 84-91. doi: 10.1515/biol-2021-0011
[6] Yang F, Ma L, Zhang L, et al. Association between serum lipoprotein-associated phospholipase A2, ischemic modified albumin and acute coronary syndrome: a cross-sectional study[J]. Heart Vessels, 2019, 34(10): 1608-1614. doi: 10.1007/s00380-019-01403-3
[7] 樊均明. 临床循证治疗手册·肾脏疾病[M]. 北京: 人民卫生出版社, 2007: 58-59.
[8] 黎晓辉, 卢叶明, 梁艳萍, 等. 脂蛋白相关磷脂酶A2与肾病综合征血栓形成的相关研究[J]. 内科理论与实践, 2015, 10(5): 367-370. https://www.cnki.com.cn/Article/CJFDTOTAL-NKLL201505018.htm
[9] Rovin BH, Adler SG, Barratt J, et al. Executive summary of the KDIGO 2021 Guideline for the Management of Glomerular Diseases[J]. Kidney Int, 2021, 100(4): 753-779. doi: 10.1016/j.kint.2021.05.015
[10] 李强, 张全, 冯威, 等. 血清PLA2R抗体, KIM-1和Hcy联合检测在特发性膜性肾病患者诊断中的临床价值[J]. 临床血液学杂志, 2022, 33(6): 398-401. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2022.06.002
[11] Zou H, Li Y, Xu G. Management of anticoagulation and antiplatelet therapy in patients with primary membranous nephropathy[J]. BMC Nephrol, 2019, 20(1): 442-452. doi: 10.1186/s12882-019-1637-y
[12] Li X, Xie X, Zhao Y, et al. Some Points for the KDIGO 2021 Guideline for Prophylactic Anticoagulation in Membranous Nephropathy: Is It Clear Enough for Us to Follow?[J]. Nephron, 2023, 147(3-4): 193-198. doi: 10.1159/000525913
[13] Uzun S, Kaya. The Association of Flow-Mediated Dilatation and Blood Parameters in Primary Raynaud's Phenomenon[J]. Int J Clin Pract, 2022, 2(1): 46-52.
[14] 沃眉宏, 陆雨纯, 靳津, 等. 纤维蛋白原/前白蛋白比值和纤维蛋白原/白蛋白比值与早期糖尿病肾脏疾病患者肾小管损伤的相关性研究[J]. 中国糖尿病杂志, 2021, 29(12): 896-901. doi: 10.3969/j.issn.1006-6187.2021.12.003
[15] Wang C, Li G, Liang X, et al. Predictive Value of Fibrinogen-to-Albumin Ratio for Post-Contrast Acute Kidney Injury in Patients Undergoing Elective Percutaneous Coronary Intervention[J]. Med Sci Monit, 2020, 26(2): 924498-924508.
[16] 梁文琪, 蔡娅茜, 曹灵. 纤维蛋白原/白蛋白比值、全身炎症反应指数与慢性肾脏病患者肾功能进展的相关性研究[J]. 实用医院临床杂志, 2023, 20(1): 119-124. doi: 10.3969/j.issn.1672-6170.2023.01.032
[17] Luyendyk JP, Schoenecker JG, Flick MJ. The multifaceted role of fibrinogen in tissue injury and inflammation[J]. Blood, 2019, 133(6): 511-520. doi: 10.1182/blood-2018-07-818211
[18] van de Wouw J, Joles JA. Albumin is an interface between blood plasma and cell membrane, and not just a sponge[J]. Clin Kidney J, 2021, 15(4): 624-634.
[19] Carlisi M, Lo Presti R, Mancuso S, et al. Calculated Whole Blood Viscosity and Albumin/Fibrinogen Ratio in Patients with a New Diagnosis of Multiple Myeloma: Relationships with Some Prognostic Predictors[J]. Biomedicines, 2023, 11(3): 964-974. doi: 10.3390/biomedicines11030964
[20] Zifu T, Jiaquan L, Juan Z. Effect of Qingre Jiedu Huoxue Huayu Recipe on blood stasis and toxin syndrome in patients with non-ST segment elevation acute coronary syndrome, serum Lp-PLA2, TNF-α, and PIGF expression level[J]. Cell Mol Biol(Noisy-le-grand), 2022, 67(4): 121-129. doi: 10.14715/cmb/2021.67.4.14
[21] Verdoia M, Rolla R, Gioscia R, et al. Lipoprotein associated-phospholipase A2 in STEMI vs. NSTE-ACS patients: a marker of cardiovascular atherosclerotic risk rather than thrombosis[J]. J Thromb Thrombolysis, 2023, 6(1): 1-10.
[22] 孙晶琳, 陈涛, 张健, 等. 脂蛋白相关磷脂酶A2与老年急性ST段抬高型心肌梗死患者冠状动脉高血栓负荷相关性[J]. 中华老年心脑血管病杂志, 2020, 22(6): 577-579. doi: 10.3969/j.issn.1009-0126.2020.06.005
[23] Williams PT. Quantile-Specific Heritability of Inflammatory and Oxidative Stress Biomarkers Linked to Cardiovascular Disease[J]. J Inflamm Res, 2022, 15(1): 85-103.
[24] Ma CY, Xu ZY, Wang SP, et al. Change of Inflammatory Factors in Patients with Acute Coronary Syndrome[J]. Chin Med J(Engl), 2018, 131(12): 1444-1449.
[25] 高玉伟, 杨洪娟, 胡秀红, 等. 特发性膜性肾病临床病理特征、预后及其影响因素分析[J]. 临床军医杂志, 2021, 49(6): 673-675. https://www.cnki.com.cn/Article/CJFDTOTAL-JYGZ202106025.htm
[26] Kobayashi S, Amano H, Terawaki H, et al. Spot urine protein/creatinine ratio as a reliable estimate of 24-hour proteinuria in patients with immunoglobulin A nephropathy, but not membranous nephropathy[J]. BMC Nephrol, 2019, 20(1): 306-316. doi: 10.1186/s12882-019-1486-8
[27] 刘海波, 卢佩, 李春梦, 等. 肾病综合征患者凝血指标检测价值分析[J]. 陕西医学杂志, 2020, 49(4): 506-509. doi: 10.3969/j.issn.1000-7377.2020.04.030
[28] Chebotareva N, Berns A, McDonnell V, et al. Thrombodynamics as a tool for monitoring hemostatic disorders in patients with chronic glomerulonephritis complicated by nephrotic syndrome[J]. Clin Hemorheol Microcirc, 2022, 82(2): 141-148. doi: 10.3233/CH-221391
[29] Zhang L, Zhang F, Xu F, et al. Construction and Evaluation of a Sepsis Risk Prediction Model for Urinary Tract Infection[J]. Front Med(Lausanne), 2021, 8(1): 671184-671194.
-





 下载:
下载: