Detection and clinical significance of urinary bilirubin cast in hospitalized cholestasis patients
-
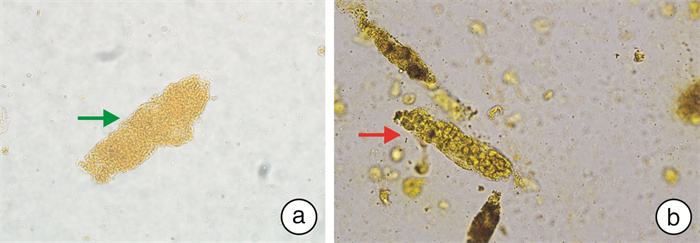
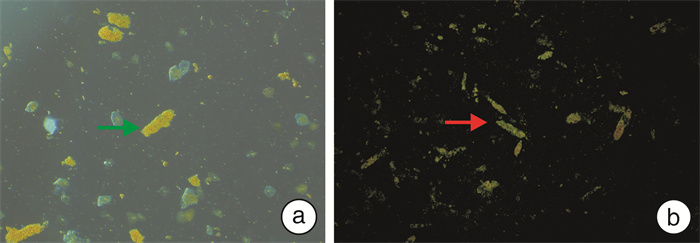
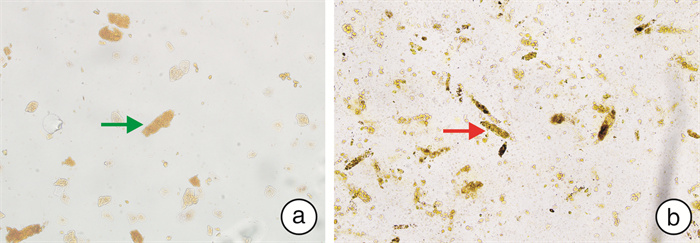
摘要: 目的 探讨胆汁淤积症患者的尿胆红素管型的检测及其临床意义。方法 回顾性分析2022年9月—2023年9月武汉协和医院的153例胆汁淤积症住院患者。根据显微镜镜检尿胆红素管型的结果将研究对象分为2组:尿胆红素管型阳性51例为研究组,包括39例肝内胆汁淤积症患者和12例肝外胆汁淤积症患者;尿胆红素管型阴性102例为对照组,包括69例肝内胆汁淤积症患者和33例肝外胆汁淤积症患者。收集2组患者的临床资料以及部分实验室检测数据,采用逻辑回归分析尿胆红素管型与总胆汁酸(TBA)、总胆红素(TBIL)、直接胆红素(DBIL)、白蛋白(ALB)和尿胆红素(UBIL)的相关性。结果 ① 研究组的肾功能不全发病率高于对照组(17.65% vs 1.96%,χ2=12.54,P < 0.01),差异有统计学意义。②研究组与对照组比较,TBIL[245.30(139.50,380.70)μmol/L vs 26.15(12.58,62.55)μmol/L,Z=8.265,P < 0.001]、DBIL[150.20(83.00,212.40)μmol/L vs 12.75(5.60,32.35)μmol/L,Z=8.559,P < 0.001]、TBA[163.90(99.60,235.90)μmol/L vs 18.55(6.98,92.28)μmol/L,Z=6.274,P < 0.001]、血肌酐(sCr)[(80.94±41.14)μmol/L vs(66.76±20.83)μmol/L,t=2.835,P=0.005]、UBIL阳性率(92.16% vs 12.75%,χ2=89.95,P < 0.01)及管型计数(UF-5000i)[0.88(0.30,2.50)个/μL vs 0.37(0.14,0.73)个/μL,Z=3.028,P=0.002]均高于对照组;ALB[(32.21±5.73) g/L vs(34.48±6.62) g/L,t=2.085,P=0.039]低于对照组;差异有统计学意义。③单变量分析显示,TBIL[OR(95%CI) 1.013(1.009~1.017),P < 0.001]、DBIL[OR(95%CI) 1.026(1.018~1.035),P < 0.001]、TBA[OR(95%CI) 1.011(1.007~1.016),P < 0.001]、ALB[OR(95%CI) 0.942(0.889~0.997),P=0.041]和UBIL(+)[OR(95%CI) 42.727(13.877~131.557),P < 0.001]均可用于预测尿胆红素管型。多变量分析显示,UBIL(+)[OR(95%CI) 7.883(1.939~32.059),P=0.004]可用于预测尿胆红素管型。结论 当胆汁淤积患者的UBIL(+)时,需通过显微镜镜检患者的离心尿中是否含有尿胆红素管型。尿胆红素管型阳性的胆汁淤积症患者的sCr较高,合并肾功能不全的概率更高。Abstract: Objective To explore the detection and clinical significance of urinary bilirubin cast in hospitalized cholestasis patients.Methods 153 hospitalized cholestasis patients were collected as study objects in our hospital during September 2022 to September 2023 for a retrospective study. 51 patients with urine bilirubin casts were selected as study group, including 39 intrahepatic cholestasis patients and 12 obstructive cholestasis patients; another 102 patients without urine bilirubin casts were selected as control group, including 69 intrahepatic cholestasis patients and 33 obstructive cholestasis patients. The clinical data and laboratory data were collected, and the relationship between urinary bilirubin cast and the TBA, TBIL, DBIL, ALB and UBIL were analyzed by logistic regression.Results ① The incidence of renal dysfunction of study group(17.65% vs 1.96%, χ2=12.54, P < 0.01) were higher than that of the control group and the difference was statistically significant. ②TBIL(245.30[139.50, 380.70]μmol/L vs 26.15[12.58, 62.55]μmol/L, Z=8.265, P < 0.001), DBIL(150.20[83.00, 212.40]μmol/L vs 12.75[5.60, 32.35]μmol/L, Z=8.559, P < 0.001), TBA(163.90[99.60, 235.90]μmol/L vs 18.55[6.98, 92.28]μmol/L, Z=6.274, P < 0.001), sCr([80.94±41.14]μmol/L vs [66.76±20.83]μmol/L, t=2.835, P=0.005) and the positive rate of UBIL(92.16% vs 12.75%; χ2=89.95, P < 0.01) and the cast values by UF-5000(0.88[0.30, 2.50]/μL vs 0.37[0.14, 0.73]/μL, Z=3.028, P=0.002) of the study group were higher than those of the control group; ALB([32.21±5.73]g/L vs [34.48±6.62]g/L, t=2.085, P=0.039) was lower than that of the control group. ③On univariate analysis, TBIL(OR[95%CI] 1.013[1.009-1.017], P < 0.001), DBIL(OR[95%CI] 1.026[1.018-1.035], P < 0.001), TBA(OR[95%CI] 1.011[1.007-1.016], P < 0.001), ALB(OR[95%CI] 0.942[0.889-0.997], P=0.041) and UBIL(+)(OR[95%CI] 42.727[13.877-131.557], P < 0.001) could be used to predict urinary bilirubin cast; On multivariate analysis, UBIL(+)(OR[95%CI] 7.883[1.939-32.059], P=0.004) could be used to predict urinary bilirubin cast.Conclusion Detection of urinary bilirubin cast in centrifuged urine by microscope was necessary for hospitalized cholestasis patients if the UBIL was positive by dry chemical method. Hospitalized cholestasis patients with urinary bilirubin cast might suffer a higher risk of renal dysfunction with relatively higher sCr levels.
-
Key words:
- cholestasis /
- urobilirubin /
- bilirubin cast /
- renal dysfunction
-

-
表 1 2组的临床资料统计分析
类型 研究组(n=51) 对照组(n=102) 性别(男/女)/例 41/10 71/31 年龄/岁 51.88±12.22 54.23±10.49 肝外胆汁淤积/例(%) 12(23.53) 33(32.35) 肝内胆汁淤积/例(%) 39(76.47) 69(67.65) 病因/例(%) 肝炎病毒(B,C,E) 36(70.59) 52(50.98) 结石 10(19.61) 21(20.59) 酒精中毒 1(1.96) 3(2.94) 药物损伤 1(1.96) 7(6.86) 自身免疫性疾病 3(5.88) 13(12.75) 胰腺/胆道肿瘤 2(3.92) 12(11.76) 并发症/例(%) 肾功能不全 9(17.65) 2(1.96) 表 2 2组的肝肾功能及尿液分析结果
指标 研究组(n=51) 对照组(n=102) 检验值 P TBIL/(μmol/L) 245.30(139.50,380.70) 26.15(12.58,62.55) Z=8.265 < 0.001 DBIL/(μmol/L) 150.20(83.00,212.40) 12.75(5.60,32.35) Z=8.559 < 0.001 TBA/(μmol/L) 163.90(99.60,235.90) 18.55(6.98,92.28) Z=6.274 < 0.001 TP/(g/L) 60.63±10.10 60.50±7.04 t=0.093 0.926 ALB/(g/L) 32.21±5.73 34.48±6.62 t=2.085 0.039 BUN/(mmol/L) 4.26(3.19,6.43) 4.66(3.50,5.83) Z=0.523 0.601 sCr/(μmol/L) 80.94±41.14 66.76±20.83 t=2.835 0.005 UBIL(+)/例(%) 47(92.16) 13(12.75) χ2=89.950 < 0.010 尿蛋白(+)/例(%) 7(13.73) 9(8.82) χ2=1.010 >0.050 管型(UF-5000i)/(个/μL) 0.88(0.30,2.50) 0.37(0.14,0.73) Z=3.028 0.002 管型阳性率(UF-5000i)/例(%) 15(29.41) 3(2.94) χ2=22.950 < 0.010 表 3 尿胆红素管型的预测指标
变量 单变量分析 多变量分析 OR(95%CI) P OR(95%CI) P TBIL 1.013(1.009~1.017) < 0.001 1.001(0.992~1.011) 0.775 DBIL 1.026(1.018~1.035) < 0.001 1.012(0.995~1.030) 0.166 TBA 1.011(1.007~1.016) < 0.001 1.002(0.997~1.008) 0.455 ALB 0.942(0.889~0.997) 0.041 0.971(0.891~1.060) 0.522 UBIL(+) 42.727(13.877~131.557) < 0.001 7.883(1.939~32.059) 0.004 -
[1] Navarro D, Fonseca NM, Ferreira AC, et al. Urinary sediment microscopy and correlations with kidney biopsy: red flags not to be missed[J]. Kidney360, 2023, 4(1): 32-40. doi: 10.34067/KID.0003082022
[2] Perazella MA, Parikh CR. How can urine microscopy influence the differential diagnosis of AKI?[J]. Clin J Am Soc Nephrol, 2009, 4(4): 691-693. doi: 10.2215/CJN.06691208
[3] Varghese V, Rivera MS, Alalwan A, et al. Concomitant identification of muddy brown granular casts and low fractional excretion of urinary sodium in AKI[J]. Kidney360, 2022, 3(4): 627-635. doi: 10.34067/KID.0005692021
[4] Liapis H, Boils C, Hennigar R, et al. Myoglobin casts in renal biopsies: immunohistochemistry and morphologic spectrum[J]. Hum Pathol, 2016, 54: 25-30. doi: 10.1016/j.humpath.2016.02.026
[5] 中华医学会检验医学分会血液学与体液学学组. 尿液检验有形成分名称与结果报告专家共识[J]. 中华检验医学杂志, 2021, 44(7): 574-586. doi: 10.3760/cma.j.cn114452-20210115-00038
[6] van Slambrouck CM, Salem F, Meehan SM, et al. Bile cast nephropathy is a common pathologic finding for kidney injury associated with severe liver dysfunction[J]. Kidney Int, 2013, 84(1): 192-197. doi: 10.1038/ki.2013.78
[7] Pinter K, Rosenkranz A. Cholemic Nephropathy: Role in Acute Kidney Injury in Cholestasis and Cirrhosis[J]. Adv Kidney Dis Health, 2024, 31(2): 111-126. doi: 10.1053/j.akdh.2023.07.001
[8] Tinti F, Umbro I, D'Alessandro M, et al. Cholemic nephropathy as cause of acute and chronic kidney disease. update on an under-diagnosed disease[J]. Life, 2021, 11(11): 1200. doi: 10.3390/life11111200
[9] 中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 胆汁淤积性肝病诊断和治疗共识(2015)[J]. 肝脏, 2015, 20(12): 950-959. https://www.cnki.com.cn/Article/CJFDTOTAL-GBSY201606042.htm
[10] Angeli P, Garcia-Tsao G, Nadim MK, et al. News in pathophysiology, definition and classification of hepatorenal syndrome: a step beyond the International Club of Ascites(ICA)consensus document[J]. J Hepatol, 2019, 71(4): 811-822. doi: 10.1016/j.jhep.2019.07.002
[11] Luciano RL, Castano E, Moeckel G, et al. Bile acid nephropathy in a bodybuilder abusing an anabolic androgenic steroid[J]. Am J Kidney Dis, 2014, 64(3): 473-476. doi: 10.1053/j.ajkd.2014.05.010
[12] van de Ven SE, Pavlov KV, Beutler JJ, et al. Bile cast nephropathy caused by obstructive pancreatic carcinoma and failed ERCP[J]. ACG Case Rep J, 2018, 5: e88. doi: 10.14309/02075970-201805000-00088
[13] Yusuf F, Weissman S, Qureshi N, et al. Bile cast nephropathy an important biliary culprit of kidney injury[J]. J Community Hosp Intern Med Perspect, 2021, 11(2): 253-255. doi: 10.1080/20009666.2021.1877397
[14] Sellinger M, Haag K, Burckhardt G, et al. Sulfated bile acids inhibit Na(+)-H+ antiport in human kidney brush-border membrane vesicles[J]. Am J Physiol, 1990, 258(4 Pt 2): F986-F991.
[15] Bomzon A, Holt S, Moore K. Bile acids, oxidative stress, and renal function in biliary obstruction[J]. Semin Nephrol, 1997, 17(6): 549-562.
[16] Krones E, Pollheimer MJ, Rosenkranz AR, et al. Cholemic nephropathy-Historical notes and novel perspectives[J]. Biochim Biophys Acta Mol Basis Dis, 2018, 1864(4 Pt B): 1356-1366.
[17] Betjes MG, Bajema I. The pathology of jaundice-related renal insufficiency: cholemic nephrosis revisited[J]. J Nephrol, 2006, 19(2): 229-233.
[18] 刘善凤, 王利民, 高云, 等. 肝病住院患者的尿胆红素与管型的相关性分析[J]. 临床血液学杂志, 2023, 36(12): 884-888, 892. doi: 10.13201/j.issn.1004-2806.2023.12.009
[19] Lee W, Ha JS, Ryoo NH. Comparison of the automated cobas u 701 urine microscopy and UF-1000i flow cytometry systems and manual microscopy in the examination of urine sediments[J]. J Clin Lab Anal, 2016, 30(5): 663-671.
[20] Giuliani KTK, Kassianos AJ, Kildey K, et al. Role of inflammation and inflammasome activation in human bile cast nephropathy[J]. Nephrology, 2020, 25(6): 502-506.
[21] Mohapatra MK, Behera AK, Karua PC, et al. Urinary bile casts in bile cast nephropathy secondary to severe falciparum malaria[J]. Clin Kidney J, 2016, 9(4): 644-648.
[22] Nayak SL, Kumar M, Bihari C, et al. Bile cast nephropathy in patients with acute kidney injury due to hepatorenal syndrome: a postmortem kidney biopsy study[J]. J Clin Transl Hepatol, 2017, 5(2): 92-100.
[23] Adebayo D, Morabito V, Davenport A, et al. Renal dysfunction in cirrhosis is not just a vasomotor nephropathy[J]. Kidney Int, 2015, 87(3): 509-515.
[24] 王江滨. 肝肾综合征的新概念[J]. 中华消化杂志, 2021, 41(5): 312-315. https://www.cnki.com.cn/Article/CJFDTOTAL-NJYK198402040.htm
[25] Zhao X, Huang RY, Wong P, et al. Renal tubular injury in hyperbilirubinemia: Bile cast nephropathy[J]. Can Liver J, 2021, 4(3): 332-337.
[26] Bräsen JH, Mederacke YS, Schmitz J, et al. Cholemic nephropathy causes acute kidney injury and is accompanied by loss of aquaporin 2 in collecting ducts[J]. Hepatology, 2019, 69(5): 2107-2119.
[27] 宦红娣. 胆汁性肾病: 肝病中被低估的引起肾功能异常的原因[J]. 肝脏, 2019, 24(7): 732-734. https://www.cnki.com.cn/Article/CJFDTOTAL-ZUAN201907003.htm
-




 下载:
下载: