Analysis of column chart model for severe hyperbilirubinemia in children with hemolytic disease of newborns
-
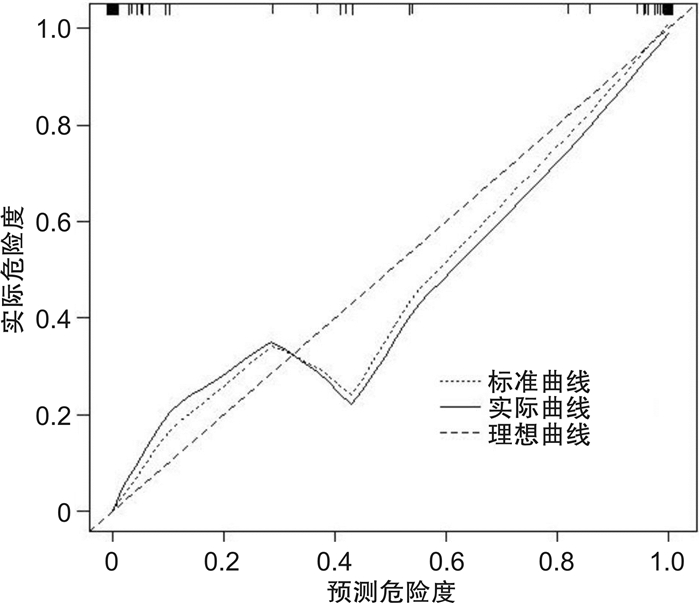
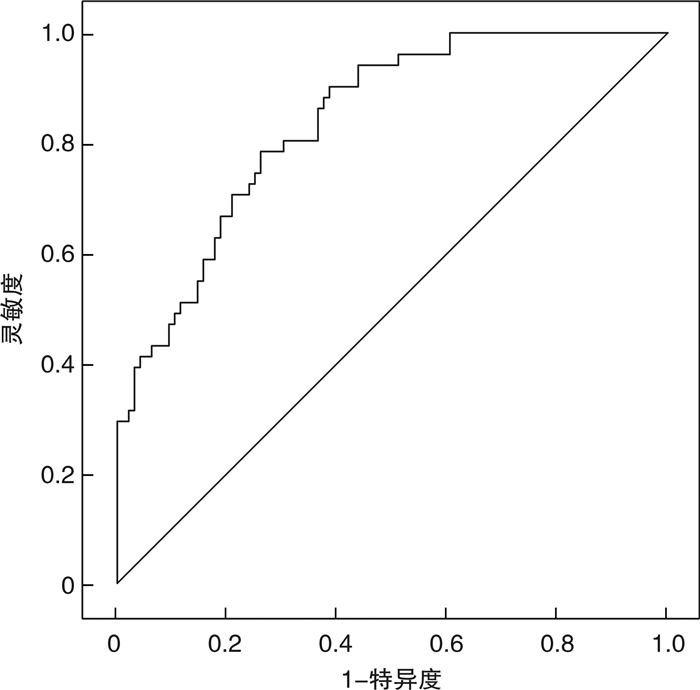
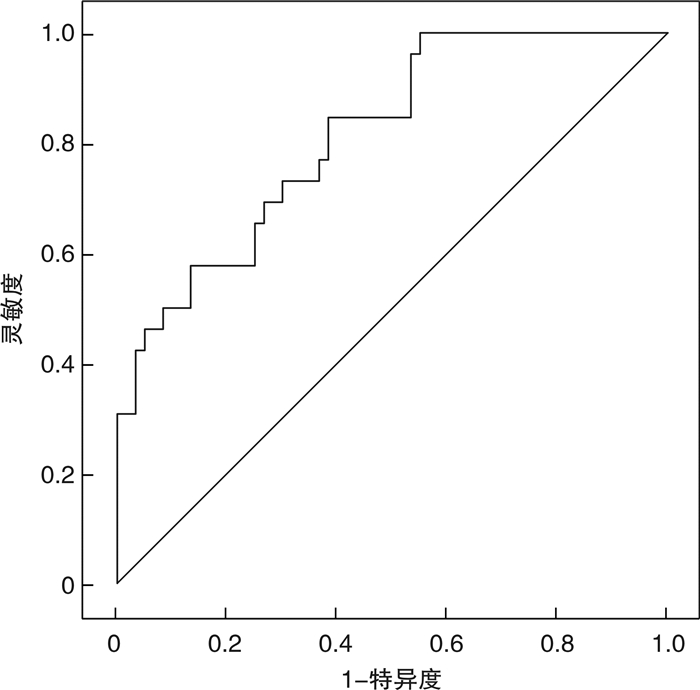
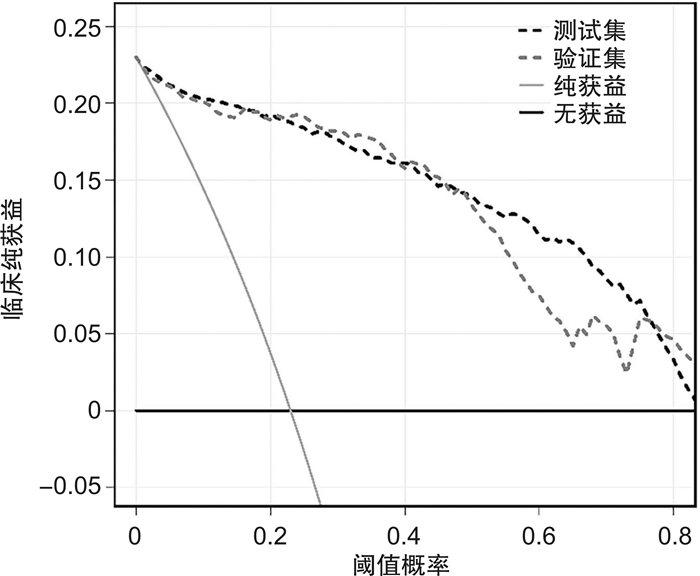
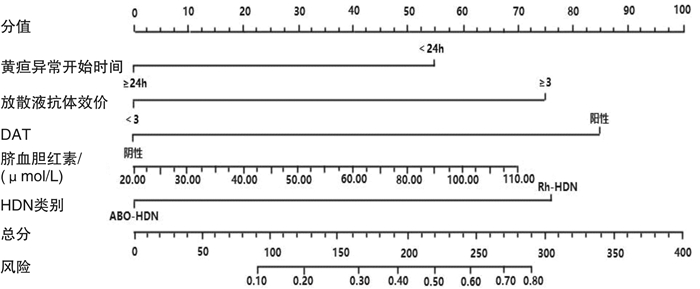
摘要: 目的 分析新生儿溶血病(hemolytic disease of newborns,HDN)患儿重度高胆红素血症影响因素和预测模型,为临床预防、治疗、规范化管理提供依据。方法 选取2021年1月—2023年10月联勤保障部队第九〇〇医院诊断和治疗的HDN患儿147例作为测试集,同期中南大学湘雅医学院附属株洲医院HDN患儿86例作为验证集。根据是否发生重度高胆红素血症将患儿分为重度高胆红素血症组和非重度高胆红素血症组,单因素和多因素分析HDN患者重度高胆红素血症的影响因素,受试者工作曲线(ROC)、校正曲线评估模型预测效能。结果 单因素和多因素分析显示,黄疸异常开始时间、放散液凝集强度、直接抗人球蛋白试验(DAT)阳性、脐血胆红素、HDN类别均为HDN患儿重度高胆红素血症的独立影响因素,OR值分别为0.387、2.549、3.015、1.043、2.559。基于二元logistic回归影响因素建立列线图模型,经验证模型在测试集预测曲线下面积(AUC)为0.842,灵敏度为78.43%,特异度为73.96%,在验证集预测AUC为0.813,灵敏度为84.61%,特异度为61.67%。决策曲线分析显示,当列线图预测概率为0~0.34时,使用该模型可获得更高的临床收益。结论 HDN重度高胆红素血症列线图模型具有较好的准确性、校准度,可为HDN发生重度高胆红素血症的预防、诊断、管理提供参考依据。Abstract: Objective To construct a predictive model for severe hyperbilirubinemia in children with hemolytic disease of newborns(HDN), and provide a basis for clinical prevention, treatment, and standardized management.Methods A total of 147 children with HDN diagnosed and treated at the 900th Hospital between January 2021 and October 2023 were selected as the test set, and 86 HDN children at the Zhuzhou Hospital affiliated to Xiangya Medical College of Central South University during the same period were selected as the validation set. According to the occurrence of severe hyperbilirubinemia, the children were divided into severe hyperbilirubinemia group and non severe hyperbilirubinemia group. The clinical data differences between the two groups were compared. Based on the principle of binary logistic regression analysis, a HDN severe hyperbilirubinemia column chart model was constructed, and the predictive performance of the model was evaluated through receiver operating curve(ROC) and correction curve.Results Univariate and multivariate analyses showed that the onset time of jaundice abnormalities, coagulation intensity of dispersed fluid, DAT positive, bilirubin in cord blood, and HDN category were all independent influencing factors for severe hyperbilirubinemia in the children with HDN, the OR values were 0.387, 2.549, 3.015, 1.043 and 2.559, respectively. Based on the above influencing factors, a risk prediction model was constructed. After verification, the model predicted an area under the curve(AUC) of 0.842, sensitivity of 78.43%, and specificity of 73.96% in the test set. The AUC predicted in the validation set was 0.813, sensitivity of 84.61%, and specificity of 61.67%. Decision curve analysis showed that when the predicted probability of the column chart model was between 0 and 0.34, using this model to predict the occurrence of severe hyperbilirubinemia in HDN could achieve higher clinical benefits.Conclusion The HDN severe hyperbilirubinemia column chart model may have good accuracy and calibration, which can provide reference for the prevention, diagnosis, and management of severe hyperbilirubinemia in HDN.
-

-
表 1 测试集、验证集间产妇、患儿临床资料比较
例(%) 临床资料 测试集
(n=147)验证集
(n=86)U/χ2 P 重度高胆红素血症 0.488 0.485 否 51(34.69) 26(30.23) 是 96(65.31) 60(69.77) 母亲年龄/岁 1.202 0.273 < 35 109(74.15) 58(67.44) ≥35 38(25.85) 28(32.56) 分娩方式 1.408 0.235 自然分娩 131(89.12) 72(83.72) 剖宫产 16(10.88) 14(16.28) 产次 1.376 0.241 初产妇 95(64.63) 62(72.09) 经产妇 52(35.37) 24(27.91) 新生儿性别 0.027 0.870 男 77(52.38) 46(53.49) 女 70(47.62) 40(46.51) 出生体重/kg 0.745 0.388 < 2.50 18(12.24) 14(16.28) ≥2.50 129(87.76) 72(83.72) 出生后Hb/(g/L) 0.778 0.378 < 150 24(16.33) 18(20.93) ≥150 123(83.67) 68(79.07) 黄疸异常开始时间/h 0.572 0.449 < 24 48(32.65) 24(27.91) ≥24 99(67.35) 62(72.09) HDN类别 0.021 0.886 HDN 136(92.52) 80(93.02) Rh-HDN 11(7.48) 6(6.98) 放散液凝集强度 0.055 0.815 < 3+ 103(70.07) 59(68.60) ≥3+ 44(29.93) 27(31.40) DAT 0.093 0.761 阴性 117(79.59) 67(77.91) 阳性 30(20.41) 19(22.09) 脐血胆红素/(μmol/L) 52.17
(32.22,69.54)51.46
(29.74,67.23)1.012 0.681 表 2 HDN患儿重度高胆红素血症单因素分析
例(%) 临床资料 研究组
(n=51)对照组
(n=96)U/χ2 P 母亲年龄/岁 0.517 0.472 < 35 36(70.59) 73(76.04) ≥35 15(29.41) 23(23.96) 分娩方式 0.062 0.803 自然分娩 45(88.24) 86(89.58) 剖宫产 6(11.76) 10(10.42) 产次 2.059 0.151 初产妇 29(56.86) 66(68.75) 经产妇 22(43.14) 30(31.25) 放散液凝集强度 4.708 0.030 < 3+ 30(58.82) 73(76.04) ≥3+ 21(41.18) 23(23.96) 新生儿性别 0.01 0.921 男 27(52.94) 50(52.08) 女 24(47.06) 46(47.92) 出生体重/kg 0.861 0.354 < 2.50 8(15.69) 10(10.42) ≥2.50 43(84.31) 86(89.58) 出生后Hb/(g/L) 1.571 0.210 < 150 11(21.57) 13(13.54) ≥150 40(78.43) 83(86.46) 黄疸异常开始时间/h 3.903 0.048 < 24 22(43.14) 26(27.08) ≥24 29(56.86) 70(72.92) HDN类别 5.885 0.015 ABO-HDN 43(84.31) 93(96.88) Rh-HDN 8(15.69) 3(3.12) DAT 5.780 0.016 阴性 35(68.63) 82(85.42) 阳性 16(31.37) 14(14.58) 脐血胆红素/(μmol/L) 54.32
(34.17,71.22)46.27
(30.06,65.35)3.121 0.013 表 3 HDN患儿重度高胆红素血症的二元logistic回归分析
变量 β SE Wald P OR 95%CI 下限 上限 黄疸异常开始时间 -0.949 0.458 4.302 0.038 0.387 0.158 0.949 放散液凝集强度 0.936 0.441 4.507 0.034 2.549 1.075 6.046 DAT阳性 1.103 0.502 4.840 0.028 3.015 1.128 8.058 脐血胆红素 0.042 0.011 13.830 <0.001 1.043 1.020 1.066 HDN类别 0.940 0.465 4.091 0.043 2.559 1.030 6.363 常数 -3.080 0.742 17.232 <0.001 0.046 表 4 模型在测试集、验证集预测效能
组别 AUC
(95%CI)灵敏度
/%特异度
/%Youden
指数正确率
/%测试集 0.842
(0.777~0.903)78.43 73.96 0.524 75.51 验证集 0.813
(0.720~0.901)84.61 61.67 0.463 68.60 -
[1] Rosenfeld WN, Hudak ML, Ruiz N, et al. Stannsoporfin with phototherapy to treat hyperbilirubinemia in newborn hemolytic disease[J]. J Perinatol, 2022, 42(1): 110-115. doi: 10.1038/s41372-021-01223-2
[2] Dziegiel MH, Krog GR, Hansen AT, et al. Laboratory monitoring of mother, fetus, and newborn in hemolytic disease of fetus and newborn[J]. Transfus Med Hemother, 2021, 48(5): 306-315. doi: 10.1159/000518782
[3] Loh CLY, Lam JCM. Importance of antenatal blood group typing and antibody screening in non-ABO/Rh haemolytic disease of the newborn[J]. Ann Acad Med Singap, 2021, 50(1): 84-85. doi: 10.47102/annals-acadmedsg.2020310
[4] 郭琼, 张蜜, 胡月圆, 等. 新生儿溶血病和葡萄糖-6-磷酸脱氢酶缺乏症致重度高胆红素血症的临床特点分析[J]. 中华新生儿科杂志(中英文), 2023, 38(2): 65-69.
[5] 邹昕, 虞茜, 葛平英, 等. 常州地区Rh、MNS血型不合致新生儿溶血病的试验结果分析及治疗[J]. 检验医学与临床, 2021, 18(9): 1185-1188. doi: 10.3969/j.issn.1672-9455.2021.09.001
[6] 刘建朝, 王亚红, 贺锋. 新生儿溶血病患儿临床资料与溶血程度关系的研究[J]. 临床血液学杂志, 2021, 34(2): 105-108. doi: 10.13201/j.issn.1004-2806.2021.02.007
[7] Mehta R, Petrova A. Direct antiglobulin test in the prediction of hyperbilirubinemia and predischarge bilirubin levels in infants with mother-infant blood type incompatibility[J]. Pediatr Neonatol, 2021, 62(4): 406-411. doi: 10.1016/j.pedneo.2021.04.002
[8] 邵肖梅, 叶鸿瑁, 丘小汕. 实用新生儿学[M]. 5版. 北京: 人民卫生出版社, 2019: 767-768.
[9] 中华医学会儿科学分会新生儿学组, 《中华儿科杂志》编辑委员会. 新生儿高胆红素血症诊断和治疗专家共识[J]. 中华儿科杂志, 2014, 52(10): 745-748.
[10] 汪德清. 输血技术操作规程: 输血科部分[M]. 北京: 人民卫生出版社, 2016: 119-122.
[11] 刘昕, 乐芳, 王莲慧, 等. 江西地区不规则抗体致新生儿溶血病回顾性分析[J]. 中国实验血液学杂志, 2023, 31(1): 215-220.
[12] 韩婷, 唐代玉. 141例母婴血型不合患儿新生儿溶血病检测结果分析[J]. 临床血液学杂志, 2023, 36(6): 402-405. doi: 10.13201/j.issn.1004-2806.2023.06.004
[13] Wang Y, Sheng GY, Shi LN, et al. Increased serum total bilirubin-albumin ratio was associated with bilirubin encephalopathy in neonates[J]. Biosci Rep, 2020, 40(1): BSR20192152.
[14] Thakkar P, Chavda H, Doshi V. Transcutaneous bilirubin nomogram for healthy term and late preterm neonates in first 96 hours of life[J]. Indian Pediatr, 2017, 54(5): 369-372.
[15] 宋菲菲, 曾峰, 殷苑琴. 胆红素/白蛋白比值预测重度高胆红素血症新生儿神经发育的价值及诺莫图预测模型构建[J]. 热带医学杂志, 2022, 22(7): 996-1000.
[16] 符小玲, 赵兴丹, 王亚洲, 等. 脐血胆红素水平结合高风险因素构建ABO新生儿溶血病发生高胆红素血症风险的预测模型与效能验证[J]. 实用医学杂志, 2023, 39(20): 2658-2663.
[17] Castillo A, Grogan TR, Wegrzyn GH, et al. Umbilical cord blood bilirubins, gestational age, and maternal race predict neonatal hyperbilirubinemia[J]. PLoS One, 2018, 13(6): e0197888.
[18] 陈娟, 黄蓉, 胡文静. 不同病因的新生儿高胆红素血症换血治疗前后相关指标分析[J]. 临床输血与检验, 2022, 24(5): 596-599.
[19] 胡丽华. 临床输血学检验技术[M]. 北京: 人民卫生出版社, 2017: 42-43.
[20] Shin KH, Lee HJ, Song D, et al. Characteristics of bilirubin according to the results of the direct antiglobulin test and its impact in hemolytic disease of the newborn[J]. Lab Med, 2019, 50(2): 138-144.
[21] Kaplan M, Hammerman C, Vreman HJ, et al. Direct antiglobulin titer strength and hyperbilirubinemia[J]. Pediatrics, 2014, 134(5): e1340-e1344.
[22] Chowdhary S, Devi U, Giridhar S. Predicting significant hyperbilirubinemia in ABO incompatibility: is cord direct antiglobulin test useful?[J]. Indian J Hematol Blood Transfus, 2022, 38(3): 591-595.
[23] 董树岭, 刘欣, 谢莹, 等. 1040例ABO系统胎儿新生儿溶血病检测结果及其影响因素分析[J]. 中国输血杂志, 2023, 36(7): 605-609.
[24] 段灵, 陈萍, 胡红兵. 直接抗球蛋白试验和总胆红素与白蛋白比值联合检测在ABO新生儿溶血病导致的严重高胆红素血症中的临床意义[J]. 临床输血与检验, 2022, 24(5): 600-604. doi: 10.3969/j.issn.1671-2587.2022.05.010
[25] Bhardwaj U, Kohli V, Thukral A. Management of hyperbilirubinemia in newborn infants 35 or more weeks of gestation: American academy of pediatrics, 2022[J]. Indian Pediatr, 2023, 60(1): 63-66.
-




 下载:
下载: