Construction and validation of a nomogram model for high-frequency blood transfusion in preterm infants with gestational age < 32 weeks based on multivariate analysis
-
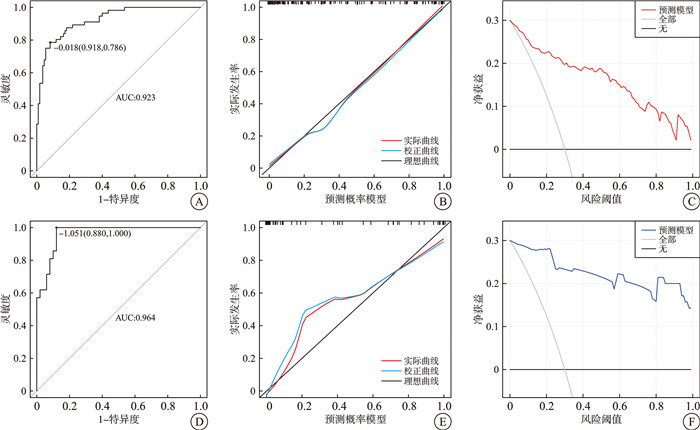
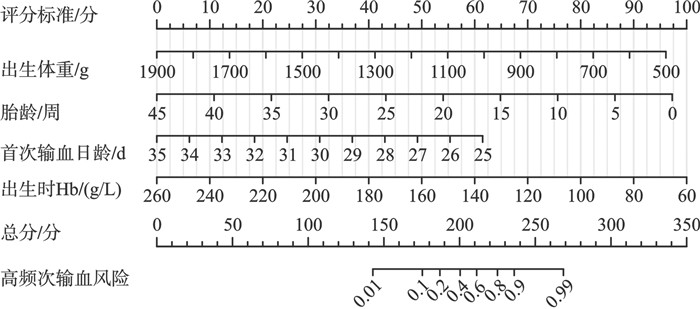
摘要: 目的 探究胎龄<32周早产儿高频次输血的相关因素,构建列线图预测模型并验证,有助于识别高风险患儿并提前干预。方法 回顾性分析2019年1月—2024年8月于医院出生的237例早产儿输血病例,以7∶3的比例对病例进行随机分配,从而形成训练集(166例)与验证集(71例)。按照早产儿的输血次数进行分组,分为低频次组(输血次数≤3次,160例)和高频次组(输血次数>3次,77例),其中训练集中低频次组110例,高频次组56例。对训练集病例采用单因素分析和logistic回归分析,筛选出最终预测变量纳入列线图预测模型,并应用验证集病例对模型进行区分度、校准度和临床决策曲线的评价。结果 训练集中低频次组与高频次组在出生体重、胎龄、阿氏评分1 min、阿氏评分5 min、阿氏评分10 min、首次输血日龄以及出生时血红蛋白(Hb)方面差异有统计学意义(P<0.05)。经过多因素logistic回归分析筛选后,将出生体重、胎龄、首次输血日龄和出生时Hb 4个预测变量纳入列线图预测模型。训练集和验证集的受试者工作特征曲线和曲线下面积依次达到0.923和0.964,表明该预测模型具有较为出色的区分度。训练集和验证集都呈现出良好的校准曲线,显示出该模型的可靠性与有效性。临床决策曲线显示该模型在0~1阈值范围内对预测胎龄<32周早产儿高频次输血风险的受益更大。结论 本研究构建的基于出生体重、胎龄、首次输血日龄和出生时Hb的列线图预测模型,具有较好的区分度、校准度和临床应用价值,可作为预测胎龄<32周早产儿高频次输血风险的评估手段。Abstract: Objective Exploring the related factors of high-frequency blood transfusion in premature infants with gestational age < 32 weeks, establishing a column chart prediction model and verifying it, can help identify high-risk children and intervene in advance.Methods Retrospective analysis of 237 premature infants born in our hospital between January 2019 and August 2024 who received blood transfusions. They were randomly divided into a training set(166 cases) and a validation set(71 cases) in a 7∶3 ratio. Based on the number of blood transfusions during hospitalization of premature infants, they were divided into a low-frequency group(transfusion frequency≤3 times, 160 cases) and a high-frequency group(transfusion frequency>3 times, 77 cases). Among them, there were 110 cases in the low-frequency group and 56 cases in the high-frequency group in the training set. Single factor analysis and logistic regression were applied in the training set to screen the final predictive factors for inclusion in the column chart prediction model, and validation set data was used to evaluate the model's discrimination, calibration and clinical decision curve.Results There were statistically significant differences(P < 0.05) between the low-frequency group and the high-frequency group in terms of birth weight, gestational age, 1-minute, 5-minute and 10 minute A-scores, age of first blood transfusion and Hb at birth in the training set. After screening through multiple logistic regression analysis, four predictive factors including birth weight, gestational age, age of first blood transfusion and Hb at birth were included in the column chart prediction model. The receiver operating characteristic curves and area under the curve of the training and validation sets reached 0.923 and 0.964, respectively, indicating that the prediction model has good discriminability, and both the training set and validation set have good calibration curves. The clinical decision curve shows that the model has a greater benefit in predicting the risk of high-frequency blood transfusions in premature infants with gestational age < 32 weeks within the threshold range of 0-1.Conclusion The column chart prediction model constructed in this study based on birth weight, gestational age, age of first transfusion and Hb at birth has good discrimination, calibration and clinical application value, and can be used as a reference tool for predicting high-frequency blood transfusions in premature infants with gestational age < 32 weeks.
-
Key words:
- premature /
- anemia /
- blood transfusion frequency /
- nomogram model
-

-
表 1 训练集2组患儿一般资料比较
X±S,M(P25,P75),例(%) 变量 低频次组(110例) 高频次组(56例) t/Z/χ2 P 出生体重/g 1 346.55±237.53 1 103.75±232.24 6.27 <0.01 胎龄/周 30.86(29.43,31.43) 28.86(28.14,29.29) -6.97 <0.01 男婴 52(47.27) 25(44.64) 0.10 0.75 剖宫产 86(78.18) 42(75.00) 0.21 0.65 双胎 15(13.64) 11(19.64) 1.01 0.31 阿氏评分1 min/分 9(8,9) 8(7,9) -2.96 <0.01 阿氏评分5 min/分 9(9,9) 9(8,9) -3.66 <0.01 阿氏评分10 min/分 9(9,9) 9(8,9) -3.80 <0.01 首次输血日龄/d 21(15,24) 7(4,11) -7.40 <0.01 出生时Hb/(g/L) 165(152,176) 156(144,166) -2.75 <0.01 表 2 训练集2组患儿母亲一般资料
X±S,M(P25,P75),例(%) 变量 低频次组(110例) 高频次组(56例) t/Z/χ2 P 年龄/岁 31.12±3.86 31.43±3.90 -0.49 0.63 孕次/次 2(1,3) 2(1,3) -0.80 0.43 产次/次 1(1,2) 1(1,2) -0.67 0.50 人工助孕 19(17.27) 10(17.86) 0.01 0.93 孕期并发症 胎膜早破 36(32.73) 13(23.21) 1.61 0.20 胎盘早剥 18(16.36) 10(17.86) 0.06 0.81 妊娠期高血压 44(40.00) 21(37.50) 0.10 0.76 妊娠期糖尿病 15(13.64) 8(14.29) 0.01 0.91 妊娠期贫血 26(23.64) 16(28.57) 0.48 0.49 前置胎盘 6(5.45) 1(1.79) 0.50 0.48 妊娠期肝内胆汁淤积症 9(8.18) 3(5.36) 0.12 0.73 胎儿宫内窘迫 27(24.55) 17(30.36) 0.64 0.42 表 3 logistic回归分析影响胎龄<32周早产儿高频次输血的因素
影响因素 β SE Wald P OR(95%CI) 出生体重 -0.005 0.002 10.231 0.001 0.995(0.992~0.998) 胎龄 -0.459 0.207 4.929 0.026 0.632(0.421~0.948) 阿氏评分1 min -0.015 0.253 0.003 0.954 0.985(0.601~1.617) 阿氏评分5 min 0.493 1.145 0.185 0.667 1.638(0.173~15.459) 阿氏评分10 min -0.271 1.166 0.054 0.816 0.763(0.078~7.493) 首次输血日龄 -0.161 0.036 19.486 <0.001 0.851(0.793~0.914) 出生时Hb -0.037 0.015 5.916 0.015 0.964(0.935~0.993) -
[1] Keir AK, Yang JM, Harrison A, et al. Temporal changes in blood product usage in preterm neonates born at less than 30 weeks' gestation in Canada[J]. Transfusion, 2015, 55(6): 1340-1346. doi: 10.1111/trf.12998
[2] Ghirardello S, Dusi E, Cortinovis I, et al. Effects of red blood cell transfusions on the risk of developing complications or death: an observational study of a cohort of very low birth weight infants[J]. Am J Perinatol, 2017, 34(1): 88-95.
[3] 李琦, 李宇丹, 许婧, 等. 早产儿贫血与输血治疗相关因素分析[J]. 中国输血杂志, 2022, 35(6): 618-621.
[4] 陈嘉雯, 谢伊玲, 杨勇. 输注红细胞对极低/超低出生体重新生儿呼吸窘迫综合征患儿的危险因素分析[J]. 中国输血杂志, 2023, 36(8): 696-700.
[5] Wang YC, Chan OW, Chiang MC, et al. Red blood cell transfusion and clinical outcomes in extremely low birth weight preterm infants[J]. Pediatr Neonatol, 2017, 58(3): 216-222. doi: 10.1016/j.pedneo.2016.03.009
[6] 欧阳足兰, 刘鑫, 倪建萍, 等. 极低出生体重儿输血并发症的影响因素分析[J]. 临床血液学杂志, 2024, 37(8): 563-567. doi: 10.13201/j.issn.1004-2806.2024.08.008
[7] 张沂洁, 朱燕, 陈超. 早产儿发生率及变化趋势[J]. 中华新生儿科杂志(中英文), 2021, 36(4): 74-77.
[8] Hasanbegovic E, Cengic N, Hasanbegovic S, et al. Evaluation and treatment of Anemia in premature infants[J]. Med Arch, 2016, 70(6): 408-412.
[9] 欧阳足兰, 倪建萍, 龙浴皎. 极低出生体重儿红细胞输注疗效及其影响因素分析[J]. 临床血液学杂志, 2024, 37(2): 94-98. doi: 10.13201/j.issn.1004-2806.2024.02.004
[10] 邓丽平, 王彦蕊, 李海英. 极早产儿与极低出生体重儿输血治疗的高危因素[J]. 滨州医学院学报, 2022, 45(6): 425-428.
[11] 刘海燕. NICU新生儿输注血液制剂的现状分析[J]. 检验医学与临床, 2024, 21(5): 677-681, 686.
[12] 宋贺, 李建刚, 赵家宁, 等. 极低和超低出生体重儿高频次输血相关因素分析[J]. 临床血液学杂志, 2023, 36(8): 583-587. doi: 10.13201/j.issn.1004-2806.2023.08.011
[13] 纪卫华, 王金元, 王红宇. 首次输血日龄与极低和超低出生体重儿近期主要并发症的相关性[J]. 中国妇幼健康研究, 2021, 32(9): 1326-1330.
[14] 张磊, 贾阳, 安婷婷, 等. 不同时机应用EPO治疗早产儿贫血的效果及对血常规指标的影响[J]. 医学临床研究, 2023, 40(5): 676-679.
[15] 郝素芳, 丁瑛雪, 杨丽君, 等. 影响早产儿贫血的相关因素分析[J]. 中国妇幼健康研究, 2017, 28(12): 1503-1507.
[16] 胡晓艳, 周于新, 徐颂周, 等. 基础血红蛋白水平对极低和超低出生体重早产儿治疗结局的影响[J]. 中国优生与遗传杂志, 2015, 23(5): 60-62.
[17] Dang D, Zhang C, Shi S, et al. Umbilical cord milking reduces need for red cell transfusions and improves neonatal adaptation in preterm infants: Meta-analysis[J]. J Obstet Gynaecol Res, 2015, 41(6): 890-895.
[18] Chiruvolu A, Tolia VN, Qin H, et al. Effect of delayed cord clamping on very preterm infants[J]. Am J Obstet Gynecol, 2015, 213(5): 676. e1-676. e7.
[19] 谢雨婕, 王蓓, 张永红, 等. 不同脐带挤勒方式对早产儿贫血的早期影响[J]. 中华新生儿科杂志(中英文), 2021, 36(5): 40-44.
[20] 赵德荣. 延迟断脐与断脐方式选择对胎龄小于32周早产儿临床结局的影响[J]. 中国医学创新, 2024, 21(8): 84-88.
[21] Mireku MO, Davidson LL, Boivin MJ, et al. Prenatal iron deficiency, neonatal ferritin, and infant cognitive function[J]. Pediatrics, 2016, 138(6): e20161319.
-

计量
- 文章访问数: 28
- 施引文献: 0



 下载:
下载: