The correlation between inflammatory indicators related to blood routine and bloodstream infections in blood disease patients with neutropenia
-
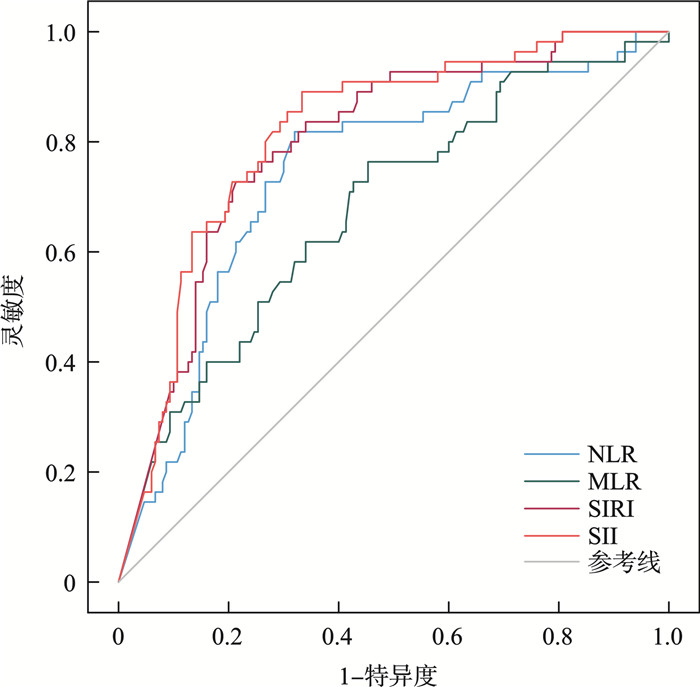
摘要: 目的 评估血常规相关炎性指标用于筛查中性粒细胞减少(chemotherapy-induced neutropenia,CIN)的血液病患者发生血流感染(bloodstream infection,BSI)的价值。方法 回顾性分析2021年8月1日—2024年7月31日就诊于医院血液内科,出现化疗导致CIN的205例血液病患者的临床资料。收集患者疑诊BSI进行血培养及鉴定,收集同时间段血常规参数(白细胞、中性粒细胞、淋巴细胞、单核细胞、血小板)的检测结果,并计算相关炎性指标:中性粒细胞计数与淋巴细胞计数比值(NLR)、单核细胞计数与淋巴细胞计数比值(MLR)、血小板计数与淋巴细胞计数比值(PLR)、全身炎症反应指数(SIRI)、全身免疫炎症指数(SII)。根据是否发生BSI分为BSI组(55例)和非BSI组(150例),比较两组血常规参数以及各炎性指标的水平。受试者工作特征(ROC)曲线分析各炎性指标筛查CIN血液病患者发生BSI的诊断价值。结果 BSI组血常规各参数、各炎性指标水平除PLR外均明显低于非BSI组,差异有统计学意义(P<0.05)。ROC分析显示NLR、MLR、SIRI、SII均可有效筛查BSI,曲线下面积(AUC)范围0.678~0.816,其中单项指标SII的AUC最高(0.816),当SII<8.089时灵敏度、阴性预测值最高;SIRI<0.008时其特异度、阳性预测值最高。结论 CIN血液病患者发生BSI时炎性指标NLR、MLR、SIRI、SII水平明显下降,各项炎性指标中SII是最合适用于筛查BSI的炎性指标,当SII<8.089时可基本排除BSI的发生。Abstract: Objective To evaluate the value of inflammatory indicators related to routine blood tests in screening for bloodstream infections(BSI) among blood disease patients with neutropenia.Methods A retrospective analysis was conducted on the clinical data of 205 patients with hematological diseases who experienced chemotherapy-induced neutropenia(CIN) at our hospital, spanning from August 1, 2021, to July 31, 2024. Concurrently, the results of blood routine parameters(including white blood cell, neutrophils, lymphocyte, monocyte and platelet) were collected from patients suspected of having bloodstream infection(BSI), and relevant inflammatory indicators were calculated: neutrophils-to-lymphocyte ratio(NLR), monocyte-to-lymphocyte ratio(MLR), platelet-to-lymphocyte ratio(PLR), systemic inflammatory response index(SIRI) and systemic immune inflammatory index(SII). Subsequently, the patients were categorized into two groups: BSI group(55 cases) and non-BSI(NBSI) group(150 cases), based on the occurrence of BSI. A comparative analysis was performed to evaluate the differences in levels of blood routine parameters and various inflammatory indicators between these two groups. Additionally, a receiver operating characteristic curve(ROC) analysis was conducted to assess the diagnostic value of various inflammatory indicators in screening for BSI among CIN hematological disease patients.Results The blood routine parameters and inflammatory index levels in the BSI group were significantly lower than those in the non-BSI group, with the exception of PLR, and these differences were statistically significant. ROC analysis demonstrated that NLR, MLR, SIRI, and SII can all serve as effective screening tools for BSI, exhibiting an area under the curve(AUC) ranging from 0.678 to 0.816. Notably, the AUC for the single indicator SII was the highest(0.816), achieving the greatest sensitivity and negative predictive value(NPV) when SII was less than 8.089. Conversely, when SIRI was less than 0.008, it displayed the highest specificity and positive predictive value(PPV).Conclusion When patients with CIN blood disease develop BSI, the levels of inflammatory markers such as NLR, MLR, SIRI and SII significantly decrease. Among these various inflammatory markers, SII is the most suitable for screening for BSI. Specifically, when SII is less than 8.089, the occurrence of BSI can be essentially ruled out.
-
Key words:
- inflammatory indicators /
- blood disease /
- neutropenia /
- bloodstream infections
-

-
表 1 BSI患者病原菌分布
病原菌 例数 构成比/% G- 大肠埃希菌 17 27.87 铜绿假单胞菌 14 22.95 肺炎克雷伯菌肺炎亚种 11 18.03 产气克雷伯菌 2 3.28 阴沟肠杆菌 1 1.64 嗜水气单胞菌 1 1.64 嗜麦芽寡养单胞菌 1 1.64 皮氏罗尔斯通氏菌 1 1.64 合计 48 78.69 G+ 金黄色葡萄球菌 4 6.56 缓症链球菌 2 3.28 肺炎链球菌 1 1.64 孔科氏葡萄球菌 1 1.64 蜡样芽孢杆菌 1 1.64 口腔链球菌 1 1.64 牛链球菌Ⅱ型 1 1.64 少酸链球菌 1 1.64 屎肠球菌 1 1.64 合计 13 21.31 总计 61 100.00 表 2 两组血常规参数及炎性指标的比较
M(P25,P75) 类型 BSI组(n=55) NBSI组(n=150) 统计值 P 年龄/岁 48(35,60) 55(44,65) -1.840 0.066 男性占比/% 45.45 58.67 2.840 0.092 血常规参数 WBC/(×109/L) 0.24(0.14,0.37) 1.13(0.56,2.25) -8.096 <0.001 中性粒细胞/(×109/L) 0.01(0.01, 0.04) 0.33(0.07, 0.74) -7.344 <0.001 淋巴细胞/(×109/L) 0.17(0.10, 0.25) 0.47(0.27, 0.83) -6.881 <0.001 单核细胞/(×109/L) 0.01(0.01, 0.04) 0.10(0.03, 0.34) -6.209 <0.001 PLT/(×109/L) 10(3, 25) 32(15, 88) -5.892 <0.001 炎性指标 NLR 0.118(0.048, 0.286) 0.605(0.208, 1.474) -5.432 <0.001 MLR 0.100(0.022, 0.184) 0.237(0.092, 0.593) -3.900 <0.001 PLR 75.000(16.667, 114.286) 71.429(32.500, 192.593) -1.327 0.184 SIRI 0.001(0, 0.009) 0.072(0.010, 0.381) -6.352 <0.001 SII 1.000(0.160, 3.391) 20.170(3.576, 68.406) -6.921 <0.001 表 3 NLR、MLR、SIRI、SII筛查CIN血液病发生BSI的性能评价
炎性指标 截断值 Youden
指数AUC(95%CI) 灵敏度
/%特异度
/%阳性
预测值/%阴性
预测值/%NLR 0.366 0.498 0.744(0.667~0.820) 81.82 68.00 48.39 91.07 MLR 0.192 0.310 0.678(0.595~0.761) 76.36 54.67 38.18 86.32 SIRI 0.008 0.501 0.797(0.731~0.752) 72.73 77.33 54.05 88.55 SII 8.089 0.558 0.816(0.752~0.879) 89.09 66.67 49.49 94.34 -
[1] 中国抗癌协会肿瘤临床化疗专业委员会, 中国抗癌协会肿瘤支持治疗专业委员会, 冯继锋, 等. 肿瘤化疗导致的CIN诊治中国专家共识(2023版)[J]. 中华肿瘤杂志, 2023, 45(7): 575-583.
[2] Ba Y, Shi YK, Jiang WQ, et al. Current management of chemotherapy-induced neutropenia in adults: key points and new challenges: Committee of Neoplastic Supportive-Care(CONS), China Anti-Cancer Association Committee of Clinical Chemotherapy, China Anti-Cancer Association[J]. Cancer Biol Med, 2020, 17(4): 896-909. doi: 10.20892/j.issn.2095-3941.2020.0069
[3] Yang JJ, Wang HM, Hua Q, et al. Diagnostic value of systemic inflammatory response index for catheter-related bloodstream infection in patients undergoing haemodialysis[J]. J Immunol Res, 2022, 2022: 7453354.
[4] Zhou T, Ren ZT, Ma YM, et al. Early identification of bloodstream infection in hemodialysis patients by machine learning[J]. Heliyon, 2023, 9(7): e18263. doi: 10.1016/j.heliyon.2023.e18263
[5] 卢玉朱, 张雪梅, 谢邦贵, 等. PCT、NLR、MLR及NEUT在诊断新生儿血流感染中的应用[J]. 中华医院感染学杂志, 2021, 31(7): 1093-1096.
[6] 刘鹏. PCT RDW SII SIRI NLR联合检测在BSI早期诊断中的价值分析[J]. 山东医学高等专科学校学报, 2024, 46(3): 26-28, 101.
[7] 邹小红, 凌利芬, 刘小晴, 等. NLR和SII在不同类型血流感染中的诊断价值[J]. 检验医学与临床, 2021, 18(17): 2501-2503.
[8] Liang PP, Yu F. Value of CRP, PCT, and NLR in prediction of severity and prognosis of patients with bloodstream infections and sepsis[J]. Front Surg, 2022, 9: 857218. doi: 10.3389/fsurg.2022.857218
[9] Roldgaard M, Benfield T, Tingsgård S. Blood neutrophil to lymphocyte ratio is associated with 90-day mortality and 60-day readmission in Gram negative bacteremia: a multi-center cohort study[J]. BMC Infect Dis, 2024, 24(1): 255. doi: 10.1186/s12879-024-09127-0
[10] Altın N, Hekimo lu CH, Unver Ulusoy T, et al. Gram-negative bloodstream infections in healthcare: the relationship between antibiotic resistance, mortality, and novel serological biomarker[J]. Cureus, 2024, 16(4): e57720.
[11] 中国医疗保健国际交流促进会临床微生物与感染分会, 中华医学会检验医学分会临床微生物学组, 中华医学会微生物学和免疫学分会临床微生物学组, 等. 血液培养技术用于血流感染诊断临床实践专家共识[J]. 中华检验医学杂志, 2022, 45(2): 105-121.
[12] Zboromyrska Y, Cillóniz C, Cobos-Trigueros N, et al. Evaluation of the magicplexTM sepsis real-time test for the rapid diagnosis of bloodstream infections in adults[J]. Front Cell Infect Microbiol, 2019, 9: 56. doi: 10.3389/fcimb.2019.00056
[13] Peri AM, Harris PNA, Paterson DL. Culture-independent detection systems for bloodstream infection[J]. Clin Microbiol Infect, 2022, 28(2): 195-201. doi: 10.1016/j.cmi.2021.09.039
[14] Ignak S, Unay-Demirel O, Yuksel M. Early prediction of bloodstream infection with complete blood count parameters: an ex-vivo human whole blood model[J]. Clin Lab, 2024, 70(4).
[15] 高陆, 彭志元, 任娜娜, 等. 恶性血液病合并血流感染病原菌分布及发生脓毒症休克危险因素分析[J]. 遵义医科大学学报, 2024, 47(3): 254-261.
[16] 郭谦, 王鑫炜, 陈新月, 等. 血液病患者并发血流感染的病原菌分布、耐药性和死亡危险因素分析[J]. 中国实验血液学杂志, 2023, 31(5): 1556-1562.
[17] 龚忠义, 魏涛, 余林. 重症血液病伴中性粒细胞减少患者血流感染病原菌分布、耐药性及预后因素分析[J]. 中国病原生物学杂志, 2024, 19(8): 950-954.
[18] 孟庆彩, 王卫红, 陈爱地, 等. 2014-2020年血液病伴中性粒细胞减少患者血流感染病原菌耐药性及预后因素分析[J]. 临床军医杂志, 2023, 51(8): 814-817.
[19] 刘晨光. 不同中性粒细胞水平恶性血液病患者血流感染病原菌分布的特点分析[D]. 沈阳: 中国医科大学, 2023.
[20] 袁丹, 郭晓敏, 刘波. 外周血NLR联合PLR对动脉粥样硬化性脑梗死诊断及预测斑块稳定性的价值研究[J]. 现代检验医学杂志, 2022, 37(1): 199-202.
[21] 杨雪彦, 吴寅平, 吕丽, 等. 单核细胞与淋巴细胞比值动态变化对慢加急性乙型肝炎肝衰竭预后的诊断价值[J]. 山东大学学报(医学版), 2024, 62(3): 61-69.
[22] Yang L, Wang HB, Ma JP, et al. Association between the platelet to lymphocyte ratio, neutrophil to lymphocyte ratio and axillary lymph node metastasis in cT1N0 breast cancer patients[J]. Am J Transl Res, 2021, 13(3): 1854-1861.
[23] 余超, 吴玉玲, 张手丽, 等. 血细胞相关比值与多发性骨髓瘤患者临床预后的相关性[J]. 临床血液学杂志, 2023, 36(4): 249-254. doi: 10.13201/j.issn.1004-2806.2023.04.006
[24] 恽琪, 崔玥, 张雯婷, 等. 血常规相关参数在儿童支原体肺炎中的表达及临床价值[J]. 临床血液学杂志, 2023, 36(12): 860-864, 868. doi: 10.13201/j.issn.1004-2806.2023.12.004
[25] 陈敏. 血液透析患者感染危险因素分析及风险评估模型的建立[D]. 南昌: 南昌大学, 2022.
-

计量
- 文章访问数: 64
- 施引文献: 0



 下载:
下载: