Association analysis of ApoE gene polymorphism with glucolipid metabolism and arteriosclerosis
-
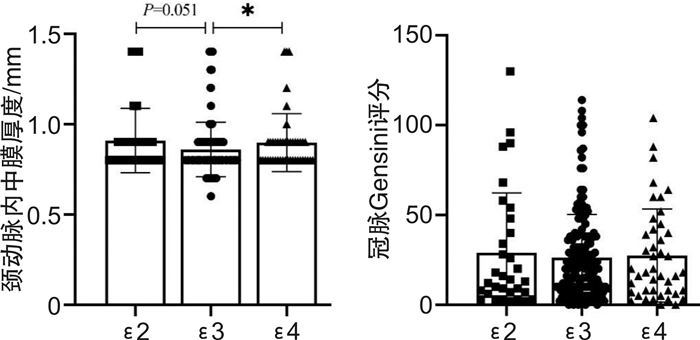
摘要: 目的 探究冠心病(coronary heart disease,CHD)患者中载脂蛋白E(ApoE)基因多态性与血脂及动脉硬化严重程度之间关联性。方法 回顾性收集2021年9月至2022年8月收治的245例CHD患者,根据ApoE基因型分组:ApoE2(32例)、ApoE3(171例)及ApoE4(42例)组,比较各组间血脂、血糖、颈动脉内中膜厚度(carotid artery intima-media thickness,cIMT)、冠脉Gensini评分以及甘油三酯葡萄糖乘积指数(triglyceride-glucose index,TyG)、致动脉粥样硬化指数(atherogenic index of plasma,AIP)的差异。结果 245例CHD患者中ε3/ε3基因型最常见(69.0%),ε3等位基因频率最高(82.4%),其次为ε4(9.6%)和ε2(8.0%)。CHD患者均已接受他汀降脂治疗,而烟酸类与贝特类药物使用较少。与ApoE3组比较,E2组患者血浆总胆固醇(cholesterol,TC)、脂蛋白a[Lipoprotein a,Lp(a)]及高密度脂蛋白胆固醇(high density lipoprotein cholesterol,HDL-C)水平降低,但差异无统计学意义(P>0.05);E4组低密度脂蛋白(low-density lipoprotein cholesterol,LDL-C)降低,甘油三酯(triglycerides,TG)则升高(均P < 0.05)。ApoE4组CHD患者的cIMT显著高于E3组,TyG与血浆促动脉硬化指数(atherogenic index of plasma,AIP)显著增加(P < 0.05);E2组患者AIP指数增加,cIMT与TyG指数与E3组比较差异无统计学意义(P>0.05)。3组间冠脉Gensini评分、颈动脉斑块比例及冠脉病变支数分布基本类似(P>0.05)。结论 ApoE2和E4基因型的CHD患者接受他汀治疗能有效改善血脂异常情况,但仍存在较高的动脉硬化与胰岛素抵抗风险。Abstract: Objective To explore the association between apolipoprotein E(ApoE) gene polymorphism and blood lipids and severity of arteriosclerosis in the patients with coronary heart disease(CHD).Methods A total of 245 patients with CHD admitted from September 2021 to August 2022 were retrospectively selected and divided into three groups according to ApoE genotype. The differences in blood lipids and glucose, carotid intima-media thickness(cIMT), coronary Gensini score, triglyceride-glucose index(TyG) and atherogenic index of plasma(AIP) were compared between groups.Results Among 245 CHD patients, the genotype ε3/ε3 was the most common(69.0%), and allele ε3 had the highest frequency(82.4%), followed by ε4(9.6%) and ε2(8.0%). All CHD patients had given statins for lipid-lowering therapy, while niacin and fibrates were less commonly used. Compared to ApoE3 group, the plasma levels of TC, Lp(a) and HDL-C in E2 group were decreased with no significance(P>0.05), while LDL-C significantly decreased and TG increased in E4 group(P < 0.05). The cIMT of CHD patients in ApoE4 group was significantly higher than that in E3 group, and the TyG and AIP index were both significantly increased(P < 0.05). AIP index increased in E2 group, while cIMT and TyG index were similar with those of E3 group(P>0.05). The Gensini score, the proportion of carotid plaque and the number of coronary artery lesions were similar among the three groups(all P>0.05).Conclusion In CHD patients with ApoE2 and E4 genotypes, statins could effectively ameliorate dyslipidemia, but still left a higher residual risk of atherosclerosis and insulin resistance.
-
Key words:
- atherosclerosis /
- apolipoprotein E /
- gene polymorphism /
- dyslipidemia /
- insulin resistance
-

-
表 1 CHD患者中ApoΕ基因型与等位基因分布频率比较
组别 ε2/ε2 ε2/ε3 ε2/ε4 ε3/ε3 ε3/ε4 ε4/ε4 ε2 ε3 ε4 频数/例 5 27 2 169 39 3 - - - 比例/% 2.0 11.0 0.8 69.0 15.9 1.2 8.0 82.4 9.6 肖懿慧/%[11] 0.7 11.7 1.2 70.3 15.3 0.8 7.1 83.8 9.1 表 2 组间血脂、血糖水平比较
X±S 项目 ApoE2(n=32) ApoE3(n=171) ApoE4(n=42) H P TC/(mmol/L) 3.36±0.98 3.80±1.09 3.65±0.90 4.868 0.088 TG/(mmol/L) 1.80±1.68 1.43±0.82 2.02±1.471) 7.391 0.025 LDL-C/(mmol/L) 1.17±0.31 1.32±0.58 1.06±0.321) 11.510 0.003 HDL-C/(mmol/L) 1.63±0.62 2.03±0.88 1.98±0.79 4.972 0.083 Lp(a)/(mg/dL) 15.80±20.30 24.00±28.40 22.50±28.10 5.423 0.066 FBG/(mmol/L) 5.47±1.46 5.84±1.99 2.99±2.27 0.624 0.732 HbA1c/% 6.21±0.90 6.28±1.20 6.17±1.27 1.200 0.549 SUA/(μmol/L) 338.70±60.20 327.00±88.40 331.30±97.10 0.532 0.766 Hcy/(μmol/L) 16.45±8.42 21.85±19.47 21.05±17.46 2.632 0.268 与ApoE3组比较,1) P < 0.05。 表 3 组间颈部斑块与冠脉病变支数比较
例(%) 项目 ApoE2(n=32) ApoE3(n=171) ApoE4(n=42) χ2 P 颈动脉斑块 25(78.1) 138(80.7) 40(95.2) 2.684 0.261 冠脉病变支数 0.505 0.973 单支 9(28.1) 42(24.9) 11(25.0) 双支 15(46.9) 78(46.2) 18(40.9) 三支 8(25.0) 44(26.0) 13(29.5) -
[1] Narula N, Olin JW, Narula N. Pathologic Disparities Between Peripheral Artery Disease and Coronary Artery Disease[J]. Arterioscler Thromb Vasc Biol, 2020, 40(9): 1982-1989. doi: 10.1161/ATVBAHA.119.312864
[2] Banach M, Stulc T, Dent R, et al. Statin non-adherence and residual cardiovascular risk: There is need for substantial improvement[J]. Int J Cardiol, 2016, 225: 184-196. doi: 10.1016/j.ijcard.2016.09.075
[3] 黎安玲, 段勇威, 廖凡路, 等. 急性脑梗死患者血栓弹力图和常规凝血试验及脂代谢指标的相关性研究[J]. 临床血液学杂志, 2020, 33(6): 871-873. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202012018.htm
[4] Marais AD. Apolipoprotein E in lipoprotein metabolism, health and cardiovascular disease[J]. Pathology, 2019, 51(2): 165-176. doi: 10.1016/j.pathol.2018.11.002
[5] 胡强, 韩雪松, 李安娜, 等. 冠心病心脏康复患者的关注焦点和影响因素分析[J]. 临床心血管病杂志, 2022, 38(10): 817-822. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202210012.htm
[6] Marais AD. Apolipoprotein E and Atherosclerosis[J]. CurrAtheroscler Rep, 2021, 23(7): 34. http://journals.lww.com/co-lipidology/Fulltext/2000/06000/Apolipoprotein_E_and_atherosclerosis.4.aspx
[7] Xu M, Zhao J, Zhang Y, et al. Apolipoprotein E Gene Variants and Risk of Coronary Heart Disease: A Meta-Analysis[J]. Biomed Res Int, 2016, 2016: 3912175. http://europepmc.org/articles/PMC5102878?pdf=render
[8] Zhang L, He S, Li Z, et al. Apolipoprotein E polymorphisms contribute to statin response in Chinese ASCVD patients with dyslipidemia[J]. Lipids Health Dis, 2019, 18(1): 129. doi: 10.1186/s12944-019-1069-5
[9] Wu Z, Liu L, Wang W, et al. Triglyceride-glucose index in the prediction of adverse cardiovascular events in patients with premature coronary artery disease: a retrospective cohort study[J]. Cardiovasc Diabetol, 2022, 21(1): 142. doi: 10.1186/s12933-022-01576-8
[10] 文洁. 血浆致动脉粥样硬化指数与非酒精性脂肪性肝病的相关性[J]. 临床荟萃, 2022, 37(1): 35-38. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFC202201006.htm
[11] 肖懿慧, 舒娟, 袁祖贻, et al. 陕西地区心血管疾病患者ApoE基因多态性分布及其与血脂水平和冠心病类型的相关性[J]. 西安交通大学学报(医学版), 2021, 42(3): 398-401. https://www.cnki.com.cn/Article/CJFDTOTAL-XAYX202103014.htm
[12] Petrovic D, Zorc M, Peterlin B. Effect of apolipoprotein E polymorphism and apolipoprotein A-1 gene promoter polymorphism on lipid parameters and premature coronary artery disease[J]. Folia Biol(Praha), 2000, 46(5): 181-185. http://europepmc.org/abstract/MED/11055796
[13] Bazzaz JT, Nazari M, Nazem h, et al. Apolipoprotein E gene polymorphism and total serum cholesterol level in Iranian population[J]. J Postgrad Med, 2010, 56(3): 173-175. http://dx.doi.org/10.4103/0022-3859.68629
[14] Ma W, Ren X, Zhang L, et al. Apolipoprotein E Gene Polymorphism and Coronary Artery Disease Risk Among Patients in Northwest China[J]. Pharmgenomics Pers Med, 2021, 14: 1591-1599. http://doc.paperpass.com/foreign/rgArti2021254617646.html
[15] Letonja M, Guzic-salobir B, Peterlin B, et al. Apolipoprotein E gene polymorphism effects triglycerides but not CAD risk in Caucasian women younger than 65 years[J]. Ann Genet, 2004, 47(2): 147-153. http://europepmc.org/abstract/MED/15636445
[16] Cheema M, Bhatti A, Wang X, et al. APOE gene polymorphism and risk of coronary stenosis in Pakistani population[J]. Biomed Res Int, 2015, 2015: 587465. http://dx.doi.org/10.1155/2015/587465
[17] Luo JQ, Ren H, Banh HL, et al. The Associations between Apolipoprotein E Gene Epsilon2/Epsilon3/Epsilon4 Polymorphisms and the Risk of Coronary Artery Disease in Patients with Type 2 Diabetes Mellitus[J]. Front Physiol, 2017, 8: 1031. http://europepmc.org/articles/PMC5732920/
[18] Chen Q, Reis SE, Kammerer CM, et al. APOE polymorphism and angiographic coronary artery disease severity in the Women's Ischemia Syndrome Evaluation(WISE)study[J]. Atherosclerosis, 2003, 169(1): 159-167. http://pubmed.ncbi.nlm.nih.gov/12860263/
[19] Sánchez DCV, Castellanos SG, Sandoval MEV, et al. B-Cell Activating Factor Increases Related to Adiposity, Insulin Resistance, and Endothelial Dysfunction in Overweight and Obese Subjects[J]. Life(Basel), 2022, 12(5): 634.
[20] Ormazabal V, Nair S, Elfeky O, et al. Association between insulin resistance and the development of cardiovascular disease[J]. Cardiovasc Diabetol, 2018, 17(1): 122.
-




 下载:
下载:
