The relationship between the proportion of peripheral blood primitive cells and the prognostic risk stratification in patients with chronic myelomonocyticleukemia
-
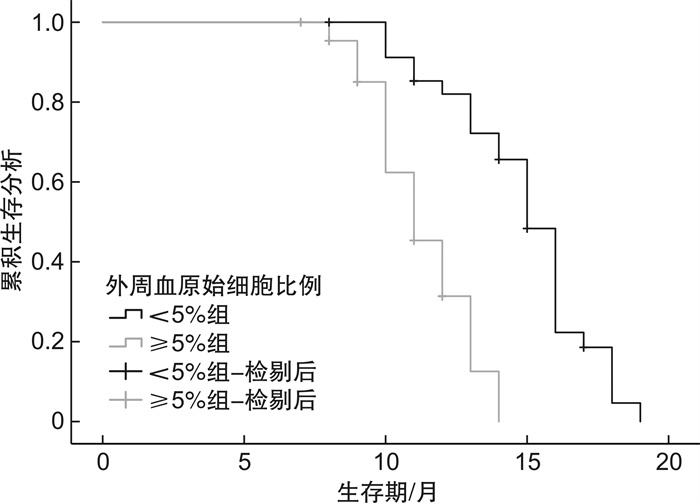
摘要: 目的 分析外周血原始细胞比例与慢性粒单核细胞白血病(CMML)患者预后危险度分层的相关性。方法 纳入医院血液科2017年10月至2023年7月收治的80例CMML患者资料进行回顾性分析,收集患者治疗前外周血原始细胞比例,治疗结束后参照全球M.D.安德森预后积分(MDAPS)将患者分为低危(20例)、中危(42例)和高危组(18例),分析外周血原始细胞比例与CMML患者预后危险度分层的关系。同时根据外周血原始细胞比例将患者分为 < 5%组(36例)和≥5%组(44例),随访记录2组患者的生存结局,分析外周血原始细胞比例与CMML患者生存结局的关系。结果 不同预后危险度分层患者白细胞计数、外周原始细胞比例、血红蛋白比较,差异有统计学意义(P < 0.05)。经Kendall's tau-b相关性检验,白细胞计数、外周血原始细胞比例与CMML患者预后危险度呈正相关,血红蛋白与预后危险度分层呈负相关(P < 0.05)。随访1年,80例患者总生存率为71.25%,原始细胞比例 < 5%组和原始细胞比例≥5%组生存率分别为77.78%(28/36)、65.91%(29/44)。Log-rank χ2检验显示,原始细胞比例 < 5%组和原始细胞比例≥5%组总生存期比较, 差异有统计学意义[(12.75±2.82)个月vs (10.45±1.74)个月,P < 0.05]。Cox回归分析显示,白细胞计数、外周血原始细胞比例是CMML患者生存结局的影响因素(P < 0.05),其他指标对CMML患者生存结局无显著影响(P>0.05)。结论 外周血原始细胞比例与CMML患者预后危险度分层有关,且患者治疗前外周血原始比例越高,生存结局越差。
-
关键词:
- 慢性粒单核细胞白血病 /
- 外周血原始细胞比例 /
- 预后危险度分层
Abstract: Objective To analyze the correlation between the proportion of peripheral blood primitive cells and the prognostic risk stratification in patients with chronic myelomonocytic leukemia(CMML).Methods The data of 80 CMML patients admitted to the Department of Hematology of Hospital from October 2017 to July 2023 were retrospectively analyzed. The proportion of peripheral blood blast cells before treatment was collected, and the patients were divided into low-risk group(20 cases), medium-risk group(42 cases) and high-risk group(18 cases) according to the global M. D. Anderson prognostic score(MDAPS) after treatment. The relationship between the proportion of peripheral blood primitive cells and the prognostic risk stratification of CMML patients was analyzed. At the same time, patients were divided into a < 5% group(36 cases) and a ≥5% group(44 cases) based on the proportion of peripheral blood primitive cells. The survival outcomes of patients in the two groups were followed up and recorded, and the relationship between the proportion of peripheral blood primitive cells and the survival outcomes of CMML patients was analyzed.Results There were significant difference in white blood cell count, peripheral primitive cell ratio, and hemoglobin in patients with different prognostic risk stratification(P < 0.05). According to Kendall's tau-b correlation test, white blood cell count, proportion of peripheral blood primitive cells, and prognosis risk of CMML patients were positively correlated, while hemoglobin was negatively correlated with prognosis risk stratification(P < 0.05). Following up for one year, the overall survival rate of 80 patients was 71.25%. The survival rates of the group with a ratio of < 5% and a ratio of ≥5% were 77.78%(28/36) and 65.91%(29/44), respectively. Log-rank χ2 tests showed that the total survival time was significantly different between the group with a ratio of < 5% of primitive cells and the group with a ratio of ≥5% of primitive cells ([12.75±2.82] months vs [10.45±1.74] months, P < 0.05). Cox regression analysis showed that white blood cell count and peripheral blood primordial cell ratio were influencing factors for the survival outcome of CMML patients(P < 0.05), while other indicators had no significant impact on the survival outcome of CMML patients(P>0.05).Conclusion The proportion of peripheral blood primordial cells is related to the risk stratification of prognosis in CMML patients, and the higher the proportion of peripheral blood primordial cells before treatment, the worse the survival outcome. -

-
表 1 MDAPS评分标准
预后参数 评分 1分 2分 3分 体力状态/分 - ≥2 - 年龄/岁 60~64 ≥65 - 骨髓原始细胞比例/% 5~10 11~29 - 血小板计数/(×109/L) 50~199 30~49 < 30 血红蛋白水平/(g/dL) - < 12 - 白细胞计数/(×109/L) - >20 - 染色体核型 - - 7号染色体异常或复杂核型≥3种 输血史 有 - - 注:“-”代表无此项。 表 2 不同预后危险度分层患者基线资料及实验室指标比较
资料 低危组(20例) 中危组(42例) 高危组(18例) χ2/F P 性别/例(%) 0.099 0.952 男 12(60.00) 24(57.14) 11(61.11) 女 8(40.00) 18(42.86) 7(38.89) 年龄/岁 68.75±4.36 66.90±5.10 67.24±4.89 疾病分型/例(%) 0.405 0.982 CMML-0 2(10.00) 4(9.52) 2(11.11) CMML-1 12(60.00) 28(66.67) 12(66.67) CMML-2 6(30.00) 10(23.81) 4(22.22) 合并症/例(%) 高血压 4(20.00) 6(14.29) 2(11.11) 0.610 0.737 糖尿病 3(15.00) 5(11.90) 2(11.11) 0.155 0.925 脾肿大/例(%) 0.272 0.873 是 2(10.00) 6(14.29) 2(11.11) 否 18(90.00) 36(85.71) 16(88.89) 输血史/例(%) 0.624 0.732 有 2(10.00) 5(11.90) 1(5.56) 无 18(90.00) 37(88.10) 17(94.44) 白细胞计数/(×109/L) 27.23±4.02 29.04±3.38 32.95±4.62 11.088 < 0.001 中性粒细胞计数/(×109/L) 10.48±2.42 11.05±2.63 12.46±2.56 3.001 0.056 单核细胞计数/(×109/L) 9.86±1.22 10.27±1.24 10.67±1.34 2.014 0.140 淋巴细胞计数/(×109/L) 3.56±1.22 3.68±1.15 3.62±1.20 0.073 0.930 外周血原始细胞比例/% 1.20±0.36 3.40±0.52 12.82±2.34 541.060 < 0.001 血红蛋白水平/(g/L) 48.85±6.70 42.11±5.95 36.85±5.36 19.090 < 0.001 白蛋白水平/(g/L) 36.20±3.44 35.63±3.52 35.10±4.14 0.426 0.655 表 3 各指标与CMML患者预后危险度分层的相关性
指标 r P 白细胞计数 0.351 < 0.001 外周血原始细胞比例 0.788 < 0.001 血红蛋白水平 -0.461 < 0.001 表 4 各指标对CMML患者生存结局影响的Cox回归分析
因素 β SE Wald P 95%CI 性别 0.498 0.879 0.321 0.571 0.294~9.204 年龄 0.006 0.066 0.009 0.924 0.885~1.145 疾病分型 CMML-1 0.313 1.039 0.091 0.764 0.095~5.605 CMML-2 1.084 1.144 0.897 0.344 0.036~3.186 高血压 0.703 0.902 0.607 0.436 0.345~11.835 糖尿病 1.341 1.004 1.782 0.182 0.534~27.375 脾肿大 0.258 0.966 0.072 0.789 0.116~5.127 输血史 0.271 1.120 0.058 0.809 0.146~11.786 白细胞计数 0.229 0.087 6.941 0.008 1.060~1.491 中性粒细胞计数 0.174 0.133 1.702 0.192 0.647~1.091 单核细胞计数 0.012 0.287 0.002 0.965 0.562~1.734 淋巴细胞计数 0.285 0.267 1.142 0.285 0.446~1.268 外周血原始细胞比例 0.323 0.117 7.573 0.006 1.098~1.739 血红蛋白水平 0.085 0.065 1.710 0.191 0.959~1.236 白蛋白水平 0.098 0.095 1.068 0.301 0.753~1.092 -
[1] Dhawan A, Padron E. Abnormal monocyte differentiation and function in chronic myelomonocytic leukemia[J]. Curr Opin Hematol, 2022, 29(1): 20-26. doi: 10.1097/MOH.0000000000000689
[2] 刘凤琪, 梁子杨, 王荷花, 等. 地西他滨联合化学治疗对中高危慢性粒单核细胞白血病的疗效分析[J]. 新医学, 2019, 50(4): 244-248. https://www.cnki.com.cn/Article/CJFDTOTAL-XYXX201904004.htm
[3] Adès L, Girshova L, Doronin VA, et al. Pevonedistat plus azacitidine vs azacitidine alone in higher-risk MDS/chronic myelomonocytic leukemia or low-blast-percentage AML[J]. Blood Adv, 2022, 6(17): 5132-5145. doi: 10.1182/bloodadvances.2022007334
[4] 中华医学会血液学分会白血病淋巴瘤学组, 肖志坚. 慢性粒-单核细胞白血病诊断与治疗中国指南(2021年版)[J]. 中华血液学杂志, 2021, 42(1): 5-9.
[5] 姜艳红, 陈光意, 盛家和, 等. 外周血原始细胞比例高于骨髓的初治原发AML的临床特征及其与患者第一次完全缓解的关系[J]. 实用医学杂志, 2018, 34(9): 1545-1549. doi: 10.3969/j.issn.1006-5725.2018.09.034
[6] 王静钰, 陈剑芳, 王世芳, 等. 慢性粒-单核细胞白血病患者临床特征及生存分析[J]. 中国实验血液学杂志, 2023, 31(2): 476-482. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY202302024.htm
[7] Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia[J]. Blood, 2016, 128(3): 462-463. doi: 10.1182/blood-2016-06-721662
[8] Savona MR, Malcovati L, Komrokji R, et al. An international consortium proposal of uniform response criteria for myelodysplastic/myeloproliferative neoplasms(MDS/MPN)in adults[J]. Blood, 2015, 125(12): 1857-1865. doi: 10.1182/blood-2014-10-607341
[9] Beran M, Wen S, Shen Y, et al. Prognostic factors and risk assessment in chronic myelomonocytic leukemia: validation study of the M.D. Anderson Prognostic Scoring System[J]. Leuk Lymphoma, 2007, 48(6): 1150-1160. doi: 10.1080/10428190701216386
[10] 王静钰, 马艳萍. 慢性粒单核细胞白血病靶向治疗研究进展[J]. 医学研究杂志, 2023, 52(1): 18-22. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYZ202301006.htm
[11] Benzarti S, Daskalakis M, Feller A, et al. Trends of incidence and survival of patients with chronic myelomonocytic leukemia between 1999 and 2014: a comparison between Swiss and American population-based cancer registries[J]. Cancer Epidemiol, 2019, 59: 51-57. doi: 10.1016/j.canep.2019.01.003
[12] Itzykson R, Fenaux P, Bowen D, et al. Diagnosis and treatment of chronic myelomonocytic leukemias in adults: recommendations from the European hematology association and the European LeukemiaNet[J]. Hemasphere, 2018, 2(6): e150. doi: 10.1097/HS9.0000000000000150
[13] 李娜, 周阳, 赵晨, 等. 单倍型造血干细胞移植与同胞相合造血干细胞移植治疗慢性粒-单核细胞白血病的疗效比较[J]. 临床血液学杂志, 2022, 35(5): 323-327. doi: 10.13201/j.issn.1004-2806.2022.05.005
[14] Bazinet A, Darbaniyan F, Jabbour E, et al. Azacitidine plus venetoclax in patients with high-risk myelodysplastic syndromes or chronic myelomonocytic leukaemia: phase 1 results of a single-centre, dose-escalation, dose-expansion, phase 1-2 study[J]. Lancet Haematol, 2022, 9(10): e756-e765. doi: 10.1016/S2352-3026(22)00216-2
[15] Hunter A, Padron E. Genomic landscape and risk stratification in chronic myelomonocytic leukemia[J]. Curr Hematol Malig Rep, 2021, 16(3): 247-255. doi: 10.1007/s11899-021-00613-9
[16] 阎拂蒙, 陈春燕. 慢性中性粒细胞白血病预后因素的研究进展[J]. 中国肿瘤临床, 2021, 48(18): 964-967. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGZL202118011.htm
[17] 唐元艳, 张利铭, 张江召, 等. 细胞发育异常在骨髓增生异常综合征患者预后评估中的价值[J]. 现代肿瘤医学, 2018, 26(11): 1759-1761. doi: 10.3969/j.issn.1672-4992.2018.11.027
[18] Guastafierro V, Ubezio M, Manes N, et al. CSF3R-mutant chronic myelomonocytic leukemia is a distinct clinically subset with abysmal prognosis: a case report and systematic review of the literature[J]. Leuk Lymphoma, 2023, 64(9): 1566-1573. doi: 10.1080/10428194.2023.2227750
[19] 武英伟, 王丽红, 耿学丽, 等. 慢性粒单核细胞白血病实验室特点及预后分析[J]. 大连医科大学学报, 2019, 41(2): 144-147, 155. https://www.cnki.com.cn/Article/CJFDTOTAL-DLYK201902013.htm
[20] 潘登, 施杰, 李艳. 慢性粒单核细胞白血病22例分析[J]. 现代肿瘤医学, 2013, 21(7): 1608-1609. doi: 10.3969/j.issn.1672-4992.2013.07.57
[21] 宋晓颖, 袁宝军, 崔晶晶, 等. 骨髓增生异常综合征患者红细胞参数水平变化及临床意义[J]. 国际检验医学杂志, 2020, 41(13): 1629-1631, 1635. doi: 10.3969/j.issn.1673-4130.2020.13.022
[22] Mei M, Pillai R, Kim S, et al. The mutational landscape in chronic myelomonocytic leukemia and its impact on allogeneic hematopoietic cell transplantation outcomes: a Center for Blood and Marrow Transplantation Research(CIBMTR)analysis[J]. Haematologica, 2023, 108(1): 150-160.
[23] 罗丽, 祝先进, 施鹏冲, 等. 红细胞参数在慢性粒细胞白血病慢性期患者诊断和治疗反应性预测中的价值[J]. 检验医学与临床, 2022, 19(9): 1177-1180, 1184. doi: 10.3969/j.issn.1672-9455.2022.09.007
-




 下载:
下载: