-
-
Key words:
- inflammatory bowel disease /
- anemia /
- diagnosis /
- treatment
-

-
表 1 估算总铁需要量的简易方案
血红蛋白/(g·dL-1) 体重 < 70 kg 体重≥70 kg 10~12(女性) 1000 mg 1500 mg 10~13(男性) 7~10 1500 mg 2000 mg -
[1] Akhuemonkhan E, Parian A, Miller K, et al. Prevalence and screening for anaemia in mild to moderate Crohn's disease and ulcerative colitis in the United States, 2010-2014[J]. BMJ Open Gastroenterol, 2017, 4(1): e000155. doi: 10.1136/bmjgast-2017-000155
[2] Resál T, Farkas K, Molnár T. Iron Deficiency Anemia in Inflammatory Bowel Disease: What Do We Know?[J]. Front Med(Lausanne), 2021, 8: 686778.
[3] Filmann N, Rey J, Schneeweiss S, et al. Prevalence of anemia in inflammatory bowel diseases in european countries: a systematic review and individual patient data meta-analysis[J]. Inflamm Bowel Dis, 2014, 20(5): 936-945. doi: 10.1097/01.MIB.0000442728.74340.fd
[4] Bonovas S, Fiorino G, Allocca M, et al. Intravenous Versus Oral Iron for the Treatment of Anemia in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials[J]. Medicine(Baltimore), 2016, 95(2): e2308. http://diposit.ub.edu/dspace/bitstream/2445/118799/1/bonovas2016_2764.pdf
[5] Khan N, Patel D, Shah Y, et al. Factors Predicting Testing and Treatment of Iron Deficiency in a Nationwide Cohort of Anemic UC Patients[J]. Inflamm Bowel Dis, 2016, 22(12): 2894-2901. https://academic.oup.com/ibdjournal/article/22/12/2894/4561948
[6] Dranga M, Boiculese LV, Popa IV, et al. Anemia in Crohn's Disease-The Unseen Face of Inflammatory Bowel Disease[J]. Medicina(Kaunas), 2021, 57(10): 1046. https://link.springer.com/article/10.1007/BF02088127
[7] Abomhya A, Tai W, Ayaz S, et al. Iron Deficiency Anemia: An Overlooked Complication of Crohn's Disease[J]. J Hematol, 2022, 11(2): 55-61.
[8] Iesalnieks I, Spinelli A, Frasson M, et al. Risk of postoperative morbidity in patients having bowel resection for colonic Crohn's disease[J]. Tech Coloproctol, 2018, 22(12): 947-953. doi: 10.1007/s10151-018-1904-0
[9] Dignass AU, Gasche C, Bettenworth D, et al. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases[J]. J Crohns Colitis, 2015, 9(3): 211-222. doi: 10.1093/ecco-jcc/jju009
[10] Martin J, Radeke HH, Dignass A, et al. Current evaluation and management of anemia in patients with inflammatory bowel disease[J]. Expert Rev Gastroenterol Hepatol, 2017, 11(1): 19-32. doi: 10.1080/17474124.2017.1263566
[11] Cacoub P, Choukroun G, Cohen-Solal A, et al. Iron deficiency screening is a key issue in chronic inflammatory diseases: A call to action[J]. J Intern Med, 2022, 292(4): 542-556. doi: 10.1111/joim.13503
[12] Shah Y, Patel D, Khan N. Iron deficiency anemia in IBD: an overlooked comorbidity[J]. Expert Rev Gastroenterol Hepatol, 2021, 15(7): 771-781. doi: 10.1080/17474124.2021.1900730
[13] Speeckaert MM, Speeckaert R, Delanghe JR. Biological and clinical aspects of soluble transferrin receptor[J]. Crit Rev Clin Lab Sci, 2010, 47(5-6): 213-228. doi: 10.3109/10408363.2010.550461
[14] Archer NM, Brugnara C. Diagnosis of iron-deficient states[J]. Crit Rev Clin Lab Sci, 2015, 52(5): 256-272.
[15] Nielsen OH, Soendergaard C, Vikner ME, et al. Rational Management of Iron-Deficiency Anaemia in Inflammatory Bowel Disease[J]. Nutrients, 2018, 10(1): 82. doi: 10.3390/nu10010082
[16] Stojkovic LM, Toncev L, Stankovic S, et al. Hepcidin Is a Reliable Marker of Iron Deficiency Anemia in Newly Diagnosed Patients with Inflammatory Bowel Disease[J]. Dis Markers, 2020, 2020: 8523205.
[17] Bergamaschi G, Di Sabatino A, Albertini R, et al. Serum hepcidin in inflammatory bowel diseases: biological and clinical significance[J]. Inflamm Bowel Dis, 2013, 19(10): 2166-2172. doi: 10.1097/MIB.0b013e31829a6e43
[18] Karaskova E, Pospisilova D, Velganova-Veghova M, et al. Importance of Hepcidin in the Etiopathogenesis of Anemia in Inflammatory Bowel Disease[J]. Dig Dis Sci, 2021, 66(10): 3263-3269. doi: 10.1007/s10620-020-06652-1
[19] Gargallo-Puyuelo CJ, Alfambra E, García-Erce JA, et al. Iron Treatment May Be Difficult in Inflammatory Diseases: Inflammatory Bowel Disease as a Paradigm[J]. Nutrients, 2018, 10(12): 1959. doi: 10.3390/nu10121959
[20] Mücke V, Mücke MM, Raine T, et al. Diagnosis and treatment of anemia in patients with inflammatory bowel disease[J]. Ann Gastroenterol, 2017, 30(1): 15-22.
[21] Muñoz M, Gómez-Ramírez S, Bhandari S. The safety of available treatment options for iron-deficiency anemia[J]. Expert Opin Drug Saf, 2018, 17(2): 149-159. doi: 10.1080/14740338.2018.1400009
[22] Kumar A, Brookes MJ. Iron Therapy in Inflammatory Bowel Disease[J]. Nutrients, 2020, 12(11): 3478. doi: 10.3390/nu12113478
[23] Lee T, Clavel T, Smirnov K, et al. Oral versus intravenous iron replacement therapy distinctly alters the gut microbiota and metabolome in patients with IBD[J]. Gut, 2017, 66(5): 863-871. doi: 10.1136/gutjnl-2015-309940
[24] Mahalhal A, Williams JM, Johnson S, et al. Oral iron exacerbates colitis and influences the intestinal microbiome[J]. PLoS One, 2018, 13(10): e0202460. doi: 10.1371/journal.pone.0202460
[25] Nielsen OH, Ainsworth M, Coskun M, et al. Management of Iron-Deficiency Anemia in Inflammatory Bowel Disease: A Systematic Review[J]. Medicine(Baltimore), 2015, 94(23): e963. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4616486/
[26] Stoffel NU, Zeder C, Brittenham GM, et al. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women[J]. Haematologica, 2020, 105(5): 1232-1239.
[27] Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials[J]. Lancet Haematol, 2017, 4(11): e524-e533. https://www.sciencedirect.com/science/article/pii/S2352302617301825
[28] Jimenez KM, Gasche C. Management of Iron Deficiency Anaemia in Inflammatory Bowel Disease[J]. Acta Haematol, 2019, 142(1): 30-36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4616486/
[29] Lee TW, Kolber MR, Fedorak RN, et al. Iron replacement therapy in inflammatory bowel disease patients with iron deficiency anemia: a systematic review and meta-analysis[J]. J Crohns Colitis, 2012, 6(3): 267-275. https://www.sciencedirect.com/science/article/pii/S1873994611002601
[30] Abhyankar A, Moss AC. Iron Replacement in Patients with Inflammatory Bowel Disease: A Systematic Review and Meta-analysis[J]. Inflamm Bowel Dis, 2015, 21(8): 1976-1981. https://academic.oup.com/ibdjournal/article/21/8/1976/4602968
[31] Tulewicz-Marti E, Moniuszko A, Rydzewska G. Management of anemia in inflammatory bowel disease: a challenge in everyday clinical practice[J]. Prz Gastroenterol, 2017, 12(4): 239-243. https://www.termedia.pl/Management-of-anemia-in-inflammatory-bowel-disease-a-challenge-in-everyday-clinical-practice,41,31239,1,1.html
[32] Akhuemonkhan E, Parian A, Carson KA, et al. Adverse Reactions After Intravenous Iron Infusion Among Inflammatory Bowel Disease Patients in the United States, 2010-2014[J]. Inflamm Bowel Dis, 2018, 24(8): 1801-1807. https://academic.oup.com/ibdjournal/article/24/8/1801/4969822
[33] Ganzoni AM. Intravenous iron-dextran: therapeutic and experimental possibilities[J]. Schweiz Med Wochenschr, 1970, 100(7): 301-303.
[34] Evstatiev R, Marteau P, Iqbal T, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease[J]. Gastroenterology, 2011, 141(3): 846-853. e841-842. https://www.sciencedirect.com/science/article/pii/S0016508511007621
[35] Kaitha S, Bashir M, Ali T. Iron deficiency anemia in inflammatory bowel disease[J]. World J Gastrointest Pathophysiol, 2015, 6(3): 62-72.
[36] Moreno López R, Sicilia Aladrén B, Gomollón García F. Use of agents stimulating erythropoiesis in digestive diseases[J]. World J Gastroenterol, 2009, 15(37): 4675-4685. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2754516/
[37] Snook J, Bhala N, Beales ILP, et al. British Society of Gastroenterology guidelines for the management of iron deficiency anaemia in adults[J]. Gut, 2021, 70(11): 2030-2051. https://gut.bmj.com/content/60/10/1309
[38] Bergamaschi G, Di Sabatino A, Corazza GR. Pathogenesis, diagnosis and treatment of anaemia in immune-mediated gastrointestinal disorders[J]. Br J Haematol, 2018, 182(3): 319-329. https://onlinelibrary.wiley.com/doi/full/10.1111/bjh.15254
[39] Kulnigg S, Teischinger L, Dejaco C, et al. Rapid recurrence of IBD-associated anemia and iron deficiency after intravenous iron sucrose and erythropoietin treatment[J]. Am J Gastroenterol, 2009, 104(6): 1460-1467. https://www.cabdirect.org/cabdirect/abstract/20093176852
-

| 引用本文: | 张红杰, 王璐. 炎症性肠病相关贫血的诊治进展[J]. 临床血液学杂志, 2022, 35(11): 771-775. doi: 10.13201/j.issn.1004-2806.2022.11.004 |
| Citation: | Advance in diagnosis and treatment of inflammatory bowel disease associated anemia[J]. J Clin Hematol, 2022, 35(11): 771-775. doi: 10.13201/j.issn.1004-2806.2022.11.004 |
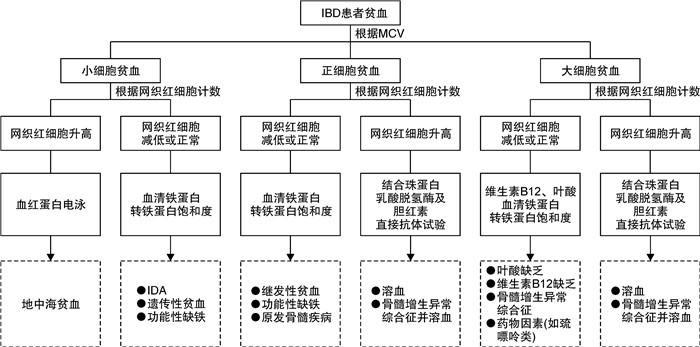
- Figure 1.



 下载:
下载: