Correlation between correlation ratio of blood cells and clinical prognosis of patients with multiple myeloma
-
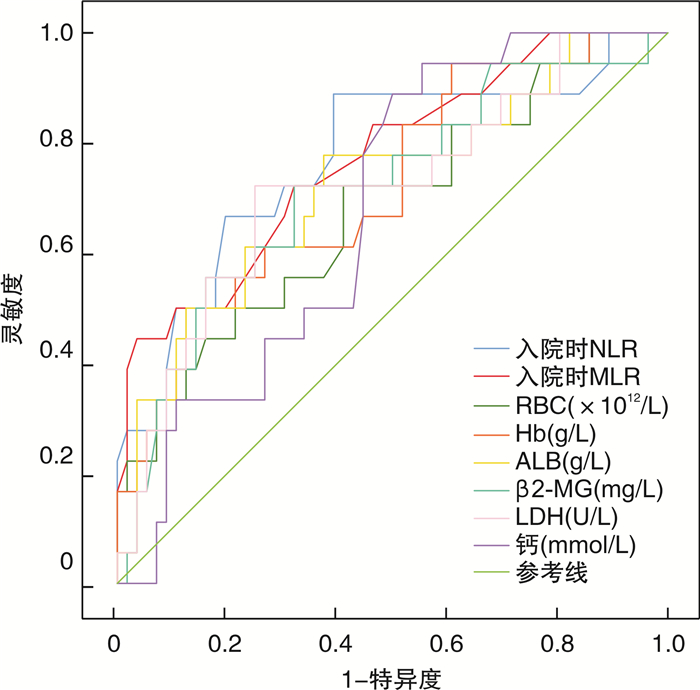
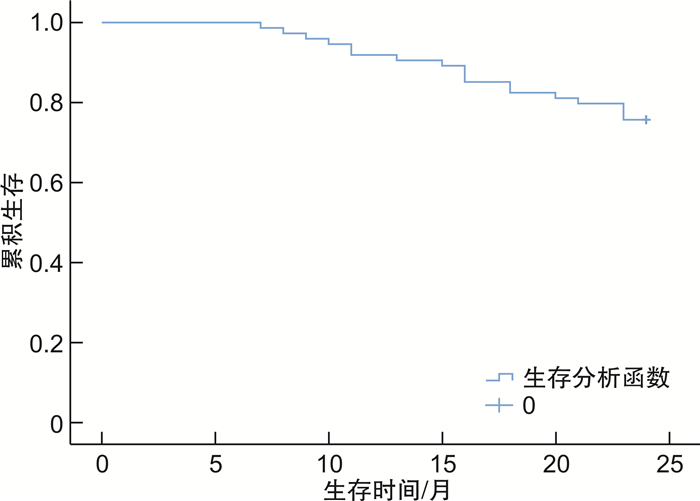
摘要: 目的 分析外周血血细胞中的中性粒细胞/淋巴细胞比值(NLR)、单核细胞/淋巴细胞比值(MLR)与多发性骨髓瘤(MM)患者临床预后的关系。方法 纳入2015年6月至2020年6月收治的85例MM患者为研究对象,患者入院后均接受化疗,自治疗开始随访2年,最后74例患者完成全过程。根据随访期间生存情况分为病死组(18例)与生存组(56例),比较2组一般资料、NLR、MLR与其他实验室指标,重点分析入院时NLR、MLR与患者临床预后的关系。结果 74例患者生存时间7~24个月,中位生存时间24.00(23.75,24.00)个月。随访期间,18例患者死亡,占24.32%;病死组疾病ISS分期较生存组高,差异有统计学意义(P < 0.05);病死组入院时及首次疗效评估时NLR、MLR均较生存组高(P < 0.05);生存组首次疗效评估时NLR、MLR值显著低于入院时(P < 0.05);但病死组首次疗效评估时NLR、MLR值与入院时比较,差异无统计学意义(P>0.05);病死组入院时红细胞计数(RBC)、β2-微球蛋白(β2-MG)、乳酸脱氢酶(LDH)、钙较生存组高,血红蛋白(Hb)、白蛋白(ALB)较生存组低,差异有统计学意义(P < 0.05);Cox回归分析显示,入院时NLR、MLR高表达是MM患者病死的独立危险因素(P < 0.05);ROC曲线显示,入院时RBC、钙预测MM患者临床预后的价值较低,入院时NLR、MLR、Hb、ALB、β2-MG、LDH对MM患者临床预后均有一定预测价值,且入院时NLR、MLR预测价值相对更高。结论 NLR、MLR与MM患者临床预后有关,可能是患者病死的独立危险因素,可作为患者临床预后的早期预测指标。
-
关键词:
- 多发性骨髓瘤 /
- 中性粒细胞/淋巴细胞比值 /
- 单核细胞/淋巴细胞比值 /
- 预后 /
- 相关性
Abstract: Objective To analyze the relationship between neutrophil/lymphocyte ratio(NLR), monocyte/lymphocyte ratio(MLR) in peripheral blood cells and the clinical prognosis of patients with multiple myeloma(MM).Methods A total of 85 MM patients admitted to the hospital from June 2015 to June 2020 were included in the study. All patients received chemotherapy after admission. They were followed up for 2 years from the beginning of treatment. They were divided into death group(18 patients) and survival group(56 patients) according to their survival during the follow-up period. The general data, NLR, MLR and other laboratory indicators of the two groups were compared, and the relationship between NLR, MLR and the clinical prognosis of the patients was analyzed.Results A total of 74 patients completed the whole process of the study. The survival time was 7-24 months, and the median survival time was 24.00(23.75, 24.00) months. During the follow-up period, 18 patients died, accounting for 24.32%. The ISS stage of disease in death group was higher than that in survival group, with statistical significant differences(P < 0.05). The NLR and MLR of the death group were higher than those of the survival group at admission and at the first evaluation of efficacy(P < 0.05). The NLR and MLR values in the survival group at the first efficacy evaluation were significantly lower than those at admission(P < 0.05). However, there was no statistical significant difference in NLR and MLR values between the death group and the admission group(P>0.05). The red blood cell count(RBC), β2-microglobulin(β2-MG), lactate dehydrogenase(LDH) and calcium in the death group were higher than those in the survival group, and hemoglobin(Hb) and albumin(ALB) were lower than those in the survival group, with statistical significant differences(P < 0.05). Cox regression analysis showed that high expression of NLR and MLR on admission were independent risk factors for death in MM patients(P < 0.05). ROC curve showed that RBC and calcium at admission had low value in predicting the clinical prognosis of MM patients. NLR, MLR, Hb, ALB, β2-MG and LDH at admission had certain predictive value for the clinical prognosis of MM patients, and NLR and MLR at admission had relatively higher predictive value.Conclusion NLR and MLR were related to the clinical prognosis of MM patients, and might be independent risk factors of death, and could be used as early predictors of clinical prognosis.-
Key words:
- multiple myeloma /
- neutrophil/lymphocyte ratio /
- monocyte/lymphocyte ratio /
- prognosis /
- relevance
-

-
表 1 2组患者入院时、首次疗效评估时NLR、MLR值比较
X±S 时间 NLR MLR 入院时 病死组 2.78±0.53 0.41±0.10 生存组 2.30±0.45 0.31±0.08 首次疗效评估时 病死组 2.63±0.46 0.35±0.09 生存组 1.96±0.39 0.19±0.09 表 2 2组患者一般资料比较
一般资料 病死组(n=18) 生存组(n=56) t/χ2/Z P 年龄/岁 72.06±2.90 71.48±2.53 0.807 0.422 性别/例(%) 0.147 0.701 男 11(61.11) 37(66.07) 女 7(38.89) 19(33.93) 疾病分型/例(%) 0.320 0.988 IgG型 8(44.44) 22(39.29) IgA型 6(33.33) 19(33.93) IgD型 1(5.56) 3(5.36) 轻链型 2(11.11) 7(12.50) 其他 1(5.56) 5(8.93) 疾病ISS分期/例(%) 2.535 0.011 Ⅰ期 5(27.78) 33(58.93) Ⅱ期 5(27.78) 13(23.21) Ⅲ期 8(44.44) 10(17.86) 慢性病史/例(%) 糖尿病 4(22.22) 9(16.07) 0.058 0.810 高血压 7(38.89) 17(30.36) 0.452 0.501 冠心病 3(16.67) 7(12.50) 0.003 0.957 表 3 2组患者治疗前其他实验室指标比较
X±S 实验室指标 病死组(n=18) 生存组(n=56) t P WBC/(×109·L-1) 5.58±0.62 5.86±0.54 1.805 0.075 RBC/(×1012·L-1) 2.46±0.75 2.98±0.67 2.775 0.007 PLT/(×109·L-1) 249.51±21.85 252.51±20.79 0.527 0.600 Hb/(g·L-1) 70.36±4.21 73.89±3.85 3.312 0.001 ALB/(g·L-1) 32.63±3.50 35.57±3.32 3.223 0.002 CRP/(mg·L-1) 8.03±1.19 7.46±1.23 1.752 0.090 β2-MG/(mg·L-1) 6.31±0.90 5.66±1.00 2.474 0.016 LDH/(U·L-1) 376.85±28.41 351.42±27.83 3.320 0.002 钙/(mmol·L-1) 3.22±0.42 2.90±0.57 2.220 0.030 D-D/(mg·L-1) 1.62±0.35 1.56±0.26 0.684 0.496 FIB/(g·L-1) 4.11±0.85 3.79±0.69 1.622 0.109 表 4 NLR、MLR之间及二者与MM患者临床预后的关系
指标 病死风险 MLR r P r P NLR 0.404 < 0.001 0.280 0.016 MLR 0.455 < 0.001 - - 表 5 NLR、MLR对MM患者临床预后影响的Cox回归分析
指标 β SE Wald P HR 95%CI NLR 1.009 0.484 4.347 0.037 2.742 1.062~7.076 MLR 5.957 2.422 6.051 0.014 386.376 3.355~44 496.020 表 6 NLR、MLR及其他实验室指标对MM患者临床预后的预测价值
指标 AUC 95%CI P 截断值 敏感度 特异度 NLR 0.769 0.634~0.904 0.001 2.360 0.889 0.607 MLR 0.770 0.643~0.898 0.001 0.335 0.722 0.679 RBC 0.681 0.534~0.827 0.022 2.910 0.722 0.589 Hb 0.720 0.583~0.856 0.005 71.835 0.611 0.732 ALB 0.721 0.580~0.863 0.005 35.180 0.778 0.625 β2-MG 0.717 0.575~0.858 0.006 6.030 0.722 0.679 LDH 0.718 0.576~0.861 0.006 368.880 0.722 0.750 钙 0.677 0.551~0.803 0.025 2.920 0.778 0.554 -
[1] 赵建治, 糜坚青. 多发性骨髓瘤相关生物标志物的研究进展[J]. 诊断学理论与实践, 2021, 20(5): 507-511. doi: 10.16150/j.1671-2870.2021.05.016
[2] 钱文斯, 谢彦晖. 老年多发性骨髓瘤治疗进展[J]. 老年医学与保健, 2022, 28(3): 469-474. doi: 10.3969/j.issn.1008-8296.2022.03.003
[3] 陈延杰. 多发性骨髓瘤患者血清sICAM-1, sVCAM-1, Treg水平与预后的相关性分析[J]. 临床血液学杂志, 2021, 34(4): 259-263.
[4] Flynt E, Bisht K, Sridharan V, et al. Prognosis, Biology, and Targeting of TP53 Dysregulation in Multiple Myeloma[J]. Cells, 2020, 9(2): 287. doi: 10.3390/cells9020287
[5] 贾淑青. 多发性骨髓瘤患者预后的相关影响因素分析[J]. 实用癌症杂志, 2022, 37(4): 605-607. doi: 10.3969/j.issn.1001-5930.2022.04.022
[6] 袁成, 邓晰明, 刘成, 等. NLR联合MPR对脓毒症患者辅助诊断及病情评估的价值[J]. 临床急诊杂志, 2022, 23(6): 400-405. doi: 10.13201/j.issn.1009-5918.2022.06.006
[7] Szudy-Szczyrek A, Mlak R, Mielnik M, et al. Prognostic value of pretreatment neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in multiple myeloma patients treated with thalidomide-based regimen[J]. Ann Hematol, 2020, 99(12): 2881-2891. doi: 10.1007/s00277-020-04092-5
[8] 孙延庆, 张启科, 魏小芳, 等. 中性粒细胞/淋巴细胞比值及单核细胞/淋巴细胞比值在多发性骨髓瘤患者中的预后意义[J]. 中国实验血液学杂志, 2021, 29(1): 122-130. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY202101024.htm
[9] 中国医师协会血液科医师分会, 中华医学会血液学分会, 中国多发性骨髓瘤工作组. 中国多发性骨髓瘤诊治指南(2013年修订)[J]. 中华内科杂志, 2013, 52(9): 791-795. doi: 10.3760/cma.j.issn.0578-1426.2013.09.026
[10] 安然, 陈钰, 张苏江, 等. 免疫炎性指标和淋巴细胞亚群在初诊多发性骨髓瘤预后判断中的意义[J]. 临床血液学杂志, 2022, 35(3): 168-173. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2022.03.004
[11] Cowan AJ, Green DJ, Kwok M, et al. Diagnosis and Management of Multiple Myeloma: A Review[J]. JAMA, 2022, 327(5): 464-477. doi: 10.1001/jama.2022.0003
[12] Hofbauer D, Mougiakakos D, Broggini L, et al. β2-microglobulin triggers NLRP3 inflammasome activation in tumor-associated macrophages to promote multiple myeloma progression[J]. Immunity, 2021, 54(8): 1772-1787. doi: 10.1016/j.immuni.2021.07.002
[13] 郭苗, 刘玮, 李伟. FIB, NLR, PLR联合检测在非小细胞肺癌早期诊断及预后评估中的价值[J]. 海南医学, 2020, 31(15): 1954-1957. https://www.cnki.com.cn/Article/CJFDTOTAL-HAIN202015014.htm
[14] 潘志鹏, 张黎, 王安琪, 等. 全血MLR, NLR及血清癌胚抗原在胃癌诊断中的价值[J]. 安徽医科大学学报, 2021, 56(11): 1807-1810. https://www.cnki.com.cn/Article/CJFDTOTAL-YIKE202111025.htm
[15] 王营, 倪虹. 中性粒细胞淋巴细胞比值动态变化对卵巢癌预后的预测价值[J]. 陕西医学杂志, 2020, 49(2): 197-200, 204. https://www.cnki.com.cn/Article/CJFDTOTAL-SXYZ202002019.htm
[16] 姜金彤, 卓杨, 赵倩, 等. NLR与急性冠状动脉综合征中OCT诊断的冠状动脉斑块破裂的关系研究[J]. 临床心血管病杂志, 2023, 39(1): 45-50.
[17] 李静, 金仁华, 洪亮, 等. 中性粒细胞与淋巴细胞和血小板比值对急性Stanford A型主动脉夹层患者急性肾损伤的早期预测价值[J]. 临床急诊杂志, 2022, 23(11): 787-793. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202211009.htm
[18] Li M, Lin C, Deng H, et al. A Novel Peptidylarginine Deiminase 4(PAD4) Inhibitor BMS-P5 Blocks Formation of Neutrophil Extracellular Traps and Delays Progression of Multiple Myeloma[J]. Mol Cancer Ther, 2020, 19(7): 1530-1538.
[19] Stork M, Bezdekova R, Kralova R, et al. Prognostic significance of lymphocyte patterns in multiple myeloma patients after autologous transplant[J]. Neoplasma, 2021, 68(3): 519-527.
[20] Suzuki K, Nishiwaki K, Nagao R, et al. Clinical significance of the lymphocyte-to-monocyte ratio in multiple myeloma patients with negative minimal residual disease: a single-center retrospective analysis[J]. Int J Hematol, 2021, 114(5): 599-607.
-




 下载:
下载: