Study on predictive value of apoB/apoA1 for activity and poor prognosis of systemic lupus erythematosus
-
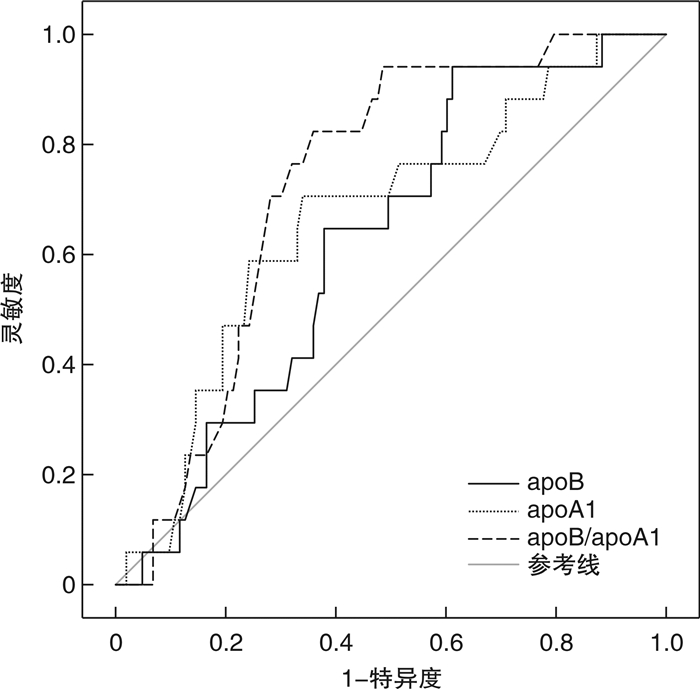
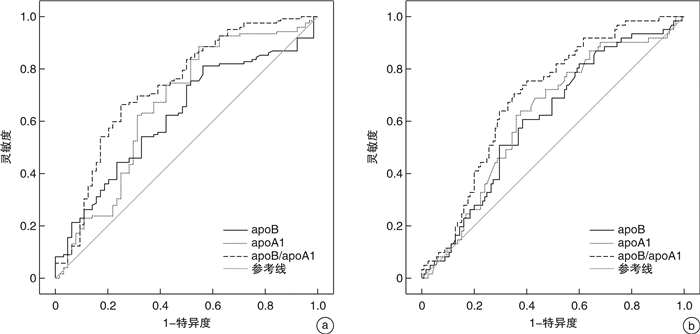
摘要: 目的 分析载脂蛋白B(apoB)/载脂蛋白A1(apoA1)对系统性红斑狼疮(systemic lupus erythematosus,SLE)活动性以及预后不良预测价值的研究。方法 回顾性分析住院治疗的SLE患者131例,根据SLE病情活动程度评分(SLEDAI)分为活动期SLE 81例,其中轻度活动期25例,中度活动期20例,重度活动期36例;稳定期SLE 50例。根据活动期SLE治疗12个月后回访结果,将活动性SLE分为预后不良组(41例)、临床缓解组(40例),分析apoB/apoA1对疾病活动性和预后不良预测价值。结果 apoB、apoA1、apoB/apoA1对活动性SLE的曲线下面积(AUC)分别为0.621、0.662、0.733,对重度活动性SLE的AUC分别为0.609、0.621、0.692,apoB/apoA1对活动性SLE、重度活动性SLE预测价值均高于apoB、apoA1,差异均有统计学意义(Z=3.172、3.981,均P < 0.05)。无论是否校正混杂因素,apoB/apoA1均为SLEDAI≥5分、SLEDAI≥10分、SLEDAI≥15分的影响因素。apoB/apoA1、apoB与SLEDAI呈正相关,apoA1与SLEDAI呈负相关,r值分别为0.474、0.192、-0.273(均P < 0.05)。二元logsitic回归显示,apoB/apoA1、血沉、抗-双链DNA(dsDNA)均为活动性SLE的独立影响因素,白蛋白、补休C3均为保护性因素,OR值分别为5.120、2.142、2.632、0.702、0.621。apoB、apoA1、apoB/apoA1对活动性SLE预后不良AUC分别为0.625、0.650、0.732,apoB/apoA1对活动性SLE预后不良预测价值高于apoB、apoA1,差异有统计学意义(Z=3.525、4.217,均P < 0.05)。二元logsitic回归显示,apoB/apoA1、抗dsDNA均为SLE预后不良独立影响因素,补休C3、ALB则为保护性因素,OR值分别为4.980、2.727、0.610、0.807(均P < 0.05)。结论 apoB/apoA1对活动性SLE、重度活动性SLE、预后不良SLE有较高预测价值,且为活动性SLE、预后不良SLE独立影响因素。Abstract: Objective To analyze the predictive value of apolipoprotein B(apoB)/apolipoprotein A1(apoA1) in the activity and poor prognosis of systemic lupus erythematosus(SLE).Methods A total of 131 SLE patients diagnosed in our hospital were collected and divided into active SLE and stable SLE, severe active SLE and non severe active SLE according to the disease activity. According to the results of 12 months follow-up after the active SLE treatment, active SLE was divided into poor prognosis group and clinical remission group. The predictive value of apoB/apoA1 on disease activity and poor prognosis was analyzed.Results The area under the curve(AUC) of apoB, apoA1, apoB/apoA1 for active SLE was 0.621, 0.662, 0.733, and for severe active SLE was 0.609, 0.621, 0.692, respectively. The predictive value of apoB/apoA1 for active SLE and severe active SLE was higher than that of apoB and apoA1, and the difference was statistically significant(all P < 0.05). Whether or not the confounding factors were corrected, the apoB/apoA1 was still the influencing factor of SLEDAI≥5, SLEDAI≥10 and SLEDAI≥15. The apoB/apoA1 and apoB were positively correlated with SLEDAI, while the apoA1 was negatively correlated with SLEDAI, the r values were 0.474, 0.192 and -0.273 respectively(all P < 0.05). The binary logsitic analysis showed that the apoB/apoA1, ESR and anti dsDNA were independent influencing factors of active SLE, while the ALB and C3 were protective factors, the OR values were 5.120, 2.142, 2.632, 0.702 and 0.621, respectively. The AUC of apoB, apoA1 and apoB/apoA1 for poor prognosis of active SLE were 0.625, 0.650 and 0.732 respectively. The predictive value of apoB/apoA1 for poor prognosis of active SLE was higher than that of apoB and apoA1, and the difference was statistically significant(all P < 0.05). The binary logsitic analysis showed that the apoB/apoA1 and anti dsDNA were independent factors for poor prognosis of SLE, while the C3 and ALB were protective factors, the OR values were 4.980, 2.727, 0.610 and 0.807 respectively(all P < 0.05).Conclusion The apoB/apoA1 had a high predictive value for active, severe active and poor prognosis SLE, and was an independent influencing factor for active and poor prognosis SLE.
-

-
表 1 apoB、apoA1、apoB/apoA1对活动性SLE预测价值
指标 AUC(95%CI) 截断值 灵敏度/% 特异度/% 正确率/% Youden指数 apoB 0.621(0.538~0.704) 1.012 g/L 60.49 62.00 61.07 0.225 apoA1 0.662(0.574~0.769) 1.360 g/L 64.20 62.00 63.36 0.262 apoB/apoA1 0.733(0.654~0.812) 0.850 75.31 60.00 69.47 0.353 表 2 apoB、apoA1、apoB/apoA1对重度活动性SLE预测价值
指标 AUC(95%CI) 截断值 灵敏度/% 特异度/% 正确率/% Youden指数 apoB 0.609(0.525~0.693) 1.250 g/L 61.11 61.05 60.07 0.222 apoA1 0.621(0.537~0.705) 1.185 g/L 63.88 63.16 63.36 0.270 apoB/apoA1 0.692(0.616~0.768) 1.024 75.00 60.00 64.12 0.350 表 3 血脂项目与SLEDAI相关性
变量 apoB/apoA1 TC TG HDL LDL apoA1 apoB TC 0.4411) TG 0.2561) 0.3901) HDL -0.2741) -0.095 -0.096 LDL 0.4121) 0.2021) 0.078 -0.096 apoA1 -0.6301) 0.1961) 0.121 0.4391) 0.102 apoB 0.5421) 0.2201) 0.2741) 0.094 0.4981) 0.110 SLEDAI 0.4741) 0.112 0.2141) -0.1751) 0.1961) -0.2731) 0.1921) 1)P < 0.05。 表 4 校正不同混杂因素前后apoB/apoA1与不同活动性SLE关系
变量 apoB apoA1 apoB/apoA1 OR(95%CI) P OR(95%CI) P OR(95%CI) P SLEDAI≥5分 模型1 2.41(0.85~9.42) 0.104 0.72(0.15~0.93) 0.032 4.41(1.52~8.02) 0.013 模型2 2.11(0.95~10.52) 0.085 0.78(0.43~0.96) 0.048 3.79(1.44~9.56) 0.026 模型3 2.23(0.96~15.35) 0.210 0.69(0.40~0.89) 0.016 6.15(2.02~13.52) <0.001 SLEDAI≥10分 模型1 1.19(0.74~8.52) 0.311 0.74(0.51~1.81) 0.145 3.15(1.19~8.74) 0.035 模型2 1.75(0.81~9.33) 0.220 0.69(0.52~1.35) 0.097 2.54(1.33~7.95) 0.026 模型3 2.13(0.84~20.51) 0.371 0.71(0.52~1.06) 0.054 4.46(1.89~11.55) 0.018 SLEDAI≥15分 模型1 1.69(0.94~6.32) 0.106 0.81(0.67~1.13) 0.072 3.62(1.735~7.52) 0.024 模型2 1.71(0.92~6.53) 0.097 0.79(0.65~1.04) 0.060 2.83(1.247~8.01) 0.035 模型3 2.51(0.93~9.72) 0.068 0.69(0.54~0.93) 0.041 4.41(1.95~11.23) 0.014 模型1为未校正任何混杂因素;模型2为校正了年龄、性别、BMI、病程;模型3为校正了HDL、LDL、TC、TG、AST、ALT、ALB、C3、C4、ESR、自身抗体。 表 5 活动性SLE影响因素分析
临床资料 单因素分析 U/t/χ2 P 多因素分析 P 活动期(n=81) 稳定期(n=50) OR 95%CI 年龄/岁 39.22±10.23 36.92±9.56 1.281 0.202 性别(男/女)/例 8/73 4/46 0.131 0.718 BMI 23.51±1.56 23.14±1.42 1.364 0.175 病程/月 14.47±6.52 13.06±5.74 1.257 0.211 SLEDAI/分 11.59±6.72 2.42±1.96 9.393 <0.001 TG/(mmol/L) 2.02±0.73 1.80±0.63 1.763 0.080 TC/(mmol/L) 4.87±1.14 4.52±0.96 1.810 0.073 HDL/(mmol/L) 1.24±0.48 1.42±0.51 2.006 0.047 LDL/(mmol/L) 2.80±0.75 2.55±0.67 2.315 0.022 apoA1/(g/L) 1.28±0.35 1.42±0.38 2.152 0.033 apoB/(g/L) 1.12±0.41 1.00±0.37 1.688 0.094 apoB/apoA1 0.90(0.42~1.16) 0.63(0.35~1.02) 4.537 <0.001 5.120 2.415~13.626 0.012 AST/(U/L) 46.32±9.78 44.21±10.33 1.174 0.243 ALT/(U/L) 45.78±11.02 43.62±9.76 1.137 0.258 ALB/(g/L) 35.74±6.21 38.29±5.96 2.318 0.022 0.702 0.597~0.934 0.034 ESR/(mm/h) 26.78±7.98 22.59±7.16 3.034 0.003 2.142 1.731~8.563 0.036 C3/(g/L) 0.64±0.26 0.82±0.34 3.416 <0.001 0.621 0.476~0.901 0.015 C4/(g/L) 0.15(0.08~0.21) 0.17(0.10~0.22) 1.574 0.153 抗dsDNA /(IU/mL) 59.33(19.25~ 86.46) 32.19(13.22~ 54.76) 1.892 0.078 抗dsDNA(+)/例(%) 50(61.73) 19(38.00) 6.983 0.008 2.632 1.273~5.438 0.014 抗Sm(+)/例(%) 28(34.57) 12(24.00) 1.628 0.202 抗ANA(+)/例(%) 81(100.00) 50(100.00) <0.001 1.000 抗SSA(+)/例(%) 48(59.26) 27(54.00) 0.349 0.554 抗SSB(+)/例(%) 14(17.28) 10(20.00) 0.152 0.696 ACA(+)/例(%) 51(62.96) 35(70.00) 0.678 0.410 表 6 apoB、apoA1、apoB/apoA1对预后不良SLE预测价值
指标 AUC(95%CI) 截断值 灵敏度/% 特异度/% 正确率/% Youden指数 apoB 0.625(0.515~0.637) 1.10 g/L 65.85 62.50 64.20 0.284 apoA1 0.650(0.550~0.794) 1.25 g/L 70.73 65.00 67.90 0.357 apoB/apoA1 0.732(0.631~0.832) 0.90 82.92 64.50 74.07 0.474 表 7 活动性SLE预后不良影响因素分析
临床资料 单因素分析 U/t/χ2 P 多因素分析 P 预后不良(n=41) 临床缓解(n=40) OR 95%CI 年龄/岁 40.12±9.86 38.30±10.22 0.816 0.417 性别(男/女)/例 5/36 3/37 0.113 0.737 BMI 23.64±1.12 23.38±1.43 0.912 0.364 病程/月 15.21±7.33 13.71±6.97 0.943 0.348 SLEDAI 12.84±5.02 10.31±4.52 2.382 0.020 TG/(mmol/L) 2.17±0.65 1.87±0.59 2.173 0.033 TC/(mmol/L) 4.91±0.71 4.83±0.92 0.439 0.662 HDL/(mmol/L) 1.16±0.37 1.32±0.41 1.842 0.069 LDL/(mmol/L) 2.88±0.54 2.72±0.61 1.251 0.215 apoA1/(g/L) 1.18±0.42 1.38±0.41 2.141 0.033 apoB/(g/L) 1.18±0.36 1.03±0.29 2.068 0.042 apoB/apoA1 0.97(0.51~1.20) 0.79(0.41~1.09) 2.975 <0.001 4.980 2.247~13.525 0.016 AST/(U/L) 45.32±8.59 47.35±7.66 1.122 0.265 ALT/(U/L) 46.17±7.52 45.38±6.37 0.510 0.612 ALB/(g/L) 33.92±5.84 37.61±6.32 2.730 0.008 0.807 0.571~0.937 0.032 ESR/(mm/h) 27.69±6.32 25.86±5.98 1.643 0.103 C3/(g/L) 0.58±0.26 0.71±0.31 2.047 0.044 0.610 0.310~0.854 0.004 C4/(g/L) 0.14(0.07~0.20) 0.16(0.08~0.22) 1.212 0.197 抗dsDNA /(IU/mL) 61.37(20.12~ 89.33) 57.24(16.75~ 84.52) 2.793 0.003 抗dsDNA(+)/例(%) 30(73.17) 20(50.00) 4.601 0.032 2.727 1.112~7.986 0.031 抗Sm(+)/例(%) 16(39.02) 12(30.00) 0.729 0.393 抗ANA(+)/例(%) 41(100.00) 40(100.00) <0.001 1.000 抗SSA(+)/例(%) 25(60.98) 23(57.50) 0.101 0.750 抗SSB(+)/例(%) 8(19.51) 6(15.00) 0.003 0.959 ACA(+)/例(%) 27(65.85) 24(60.00) 0.453 0.501 -
[1] Liu XR, Qi YY, Zhao YF, et al. Albumin-to-globulin ratio(AGR)as a potential marker of predicting lupus nephritis in Chinese patients with systemic lupus erythematosus[J]. Lupus, 2021, 30(3): 412-420. doi: 10.1177/0961203320981139
[2] 曾君, 李时飞, 周小芳, 等. 血清PS-PLA1水平与系统性红斑狼疮疾病活动相关性分析[J]. 中国麻风皮肤病杂志, 2021, 37(5): 281-285. https://www.cnki.com.cn/Article/CJFDTOTAL-MALA202105007.htm
[3] 任雪景, 阎磊, 李纳, 等. T淋巴细胞亚群和血脂水平与系统性红斑狼疮疾病活动度的相关性研究[J]. 中华实用诊断与治疗杂志, 2019, 33(2): 132-135. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD201902008.htm
[4] Hochberg MC. Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus[J]. Arthritis Rheum, 1997, 40(9): 1725.
[5] Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000[J]. J Rheumatol, 2002, 29(2): 288-291.
[6] Zen M, Iaccarino L, Gatto M, et al. Prolonged remission in Caucasian patients with SLE: prevalence and outcomes[J]. Ann Rheum Dis, 2015, 74(12): 2117-2122.
[7] Huang LY, Yang Y, Kuang Y, et al. The impact of T cell vaccination in alleviating and regulating systemic lupus erythematosus manifestation[J]. J Immunol Res, 2016, 2016: 1-9.
[8] Yee CS, Farewell V, Isenberg DA, et al. British Isles Lupus Assessment Group 2004 index is valid for assessment of disease activity in systemic lupus erythematosus[J]. Arthritis Rheum, 2007, 56(12): 4113-4119.
[9] Zhou B, Xia YL, She JQ. Dysregulated serum lipid profile and its correlation to disease activity in young female adults diagnosed with systemic lupus erythematosus: a cross-sectional study[J]. Lipids Health Dis, 2020, 19(1): 40.
[10] Wang X, Wang Z, Li B, et al. Prognosis evaluation of universal acute coronary syndrome: the interplay between SYNTAX score and apoB/apoA1[J]. BMC Cardiovasc Disor, 2020, 20(1): 293.
[11] 董海芸, 宋维兴, 李玉川, 等. 系统性红斑狼疮患者血小板参数、血脂、补体C3、C4水平与病情活动度的关系分析[J]. 现代生物医学进展, 2021, 21(12): 2382-2385, 2400. https://www.cnki.com.cn/Article/CJFDTOTAL-SWCX202112040.htm
[12] Frostegård J. Systemic lupus erythematosus and cardiovascular disease[J]. J Intern Med, 2022, 293: 48-62.
[13] Wang YD, Yu HT, He JC. Role of dyslipidemia in accelerating inflammation, autoimmunity, and atherosclerosis in systemic lupus erythematosus and other autoimmune diseases[J]. Discov Med, 2020, 30(159): 49-56.
[14] Quevedo-Abeledo JC, Sánchez-Pérez H, Tejera-Segura B, et al. Differences in capacity of high-density lipoprotein cholesterol efflux between patients with systemic lupus erythematosus and rheumatoid arthritis[J]. Arthritis Care Res, 2021, 73(11): 1590-1596.
[15] Sjöwall C, Bentow C, Aure MA, et al. Two-parametric immunological score development for assessing renal involvement and disease activity in systemic lupus erythematosus[J]. J Immunol Res, 2018, 2018: 1-9.
[16] 邓胜, 陈键. 血细胞比值、平均血小板体积评估系统性红斑狼疮活动性研究[J]. 临床血液学杂志, 2021, 34(6): 415-418, 422. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2021.06.009
[17] 庞杰, 张宗芳, 李艳霞, 等. 血清补体C5a水平和红细胞沉降率与系统性红斑狼疮疾病活动度及预后的关系[J]. 中华实用诊断与治疗杂志, 2020, 34(11): 1110-1113. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202011009.htm
[18] Wang M, Wang ZQ, Zhang SZ, et al. Relapse rates and risk factors for unfavorable neurological prognosis of transverse myelitis in systemic lupus erythematosus: a systematic review and meta-analysis[J]. Autoimmun Rev, 2022, 21(2): 102996.
[19] Zhao L, Zhang Q, Feng ZG, et al. Serum amyloid A-to-albumin ratio as a potential biomarker to predict the activity, severity, and poor prognosis of systemic lupus erythematosus[J]. J Clin Lab Anal, 2022, 36(3): e24282.
[20] Dai LL, Chen C, Wu J, et al. The predictive value of fibrinogen-to-albumin ratio in the active, severe active, and poor prognosis of systemic lupus erythematosus: a single-center retrospective study[J]. Clin Lab Anal, 2022, 36(9): e24621.
[21] Robinson GA, Waddington KE, Coelewij L, et al. Increased apolipoprotein-B: A1 ratio predicts cardiometabolic risk in patients with juvenile onset SLE[J]. EBio Medicine, 2021, 65: 103243.
-




 下载:
下载: