Predictive value of blood glucose gap for perioperative blood transfusion in elderly patients with lower limb fracture surgery
-
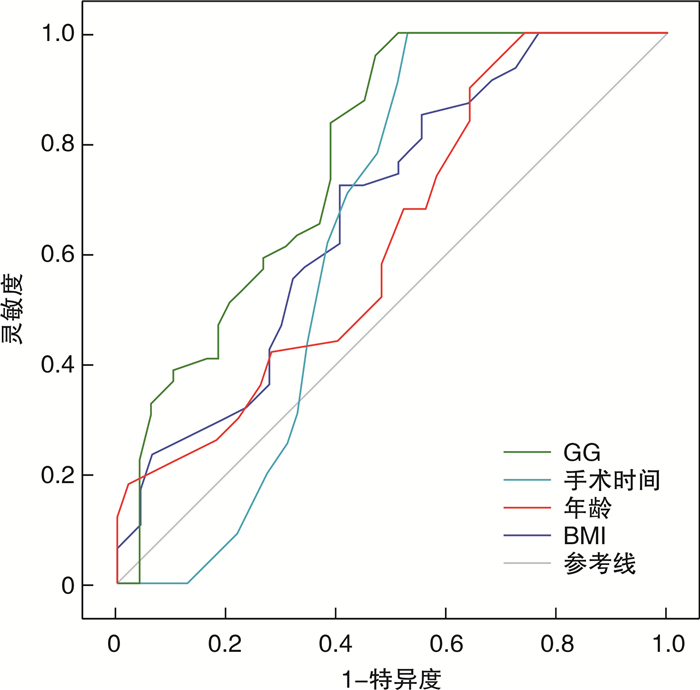
摘要: 目的 探讨血糖间隙(glycemic gap,GG)对老年下肢骨折手术患者围术期输血的预测价值。方法 选取医院2020年1月至2023年11月期间收治的行择期手术治疗的老年下肢骨折患者161例,根据患者围术期是否输血将其分为输血组(n=38)和未输血组(n=123)。比较2组临床资料,绘制受试者工作特征曲线分析GG对老年下肢骨折手术患者围术期输血的预测价值。结果 多因素logistic回归分析结果显示:年龄(OR=3.255,95%CI 1.078~9.832)、体重指数(BMI)(OR=1.688,95%CI 0.958~2.974)、手术时间(OR=1.792,95%CI 0.880~3.650)、血红蛋白(Hb)(OR=3.469,95%CI 1.799~6.689)、GG(OR=2.827,95%CI 1.432~5.581)是老年下肢骨折患者围术期输血的重要影响因素(P < 0.05)。ROC曲线分析结果显示:年龄、BMI、手术时间、GG预测老年下肢骨折患者围术期输血的曲线下面积分别为0.629、0.677、0.637、0.774,其中以GG的预测价值最佳。结论 GG预测老年下肢骨折患者围术期输血具有良好的效能,且具有容易获取、计算简单等优势,可为临床鉴别高输血人群提供参考依据。Abstract: Objective To investigate the predictive value of blood glucose gap for perioperative blood transfusion in elderly patients undergoing lower limb fracture surgery.Methods From January 2020 to November 2020, 161 elderly patients with lower extremity fractures who underwent elective surgery in our hospital were selected, patients were divided into transfusion group(n=38) and non-transfusion group(n=123) according to whether or not they received blood transfusion during the perioperative period. The clinical data of the two groups were compared, and the ROC curve was drawn to analyze the predictive value of blood glucose gap for perioperative blood transfusion in elderly patients with lower extremity fracture.Results Multivariate logistic regression analysis showed that age(OR=3.255, 95%CI 1.078-9.832), BMI(OR=1.688, 95%CI 0.958-2.974), operation time(OR=1.792, 95%CI 0.880-3.650), Hb(OR=3.469, 95%CI 1.799-6.689), blood glucose gap(OR=2.827, 95%CI 1.432-5.581) were the important influencing factors of blood transfusion in the elderly patients with lower extremity fracture during perioperative period(P < 0.05). The results of ROC curve analysis showed that the area under the curve of age, BMI, operation time and GG in predicting perioperative blood transfusion in elderly patients with lower limb fracture were 0.629, 0.677, 0.637 and 0.774, respectively, among which GG had the best predictive value.Conclusion Blood glucose gap prediction of perioperative blood transfusion in elderly patients with lower extremity fracture may have good efficacy, and have advantages of easy access, simple calculation, and can provide reference for clinical identification of high blood transfusion population.
-

-
表 1 输血组和未输血组临床资料比较
项目 输血组(n=38) 未输血组(n=123) χ2/t P 年龄/岁 78.58±8.85 72.73±6.95 4.239 < 0.001 性别/例(%) 男 9(23.68) 31(25.20) 0.036 0.850 女 29(76.32) 92(74.80) BMI/(kg/m2) 21.18±1.98 23.40±1.50 7.364 < 0.001 骨折部位/例(%) 股骨 17(44.74) 57(46.34) 0.101 0.992 股骨颈 7(18.42) 20(16.26) 胫腓骨 8(21.05) 26(21.14) 其他 6(15.79) 20(16.26) 合并基础病/例(%) 是 23(60.53) 72(58.54) 0.048 0.827 否 15(39.47) 51(41.46) ASA分级/例(%) Ⅰ级 6(15.79) 22(17.89) 7.788 0.020 Ⅱ级 21(55.26) 88(71.54) Ⅲ级 11(28.95) 13(10.57) 手术方式/例(%) 内固定术 27(71.05) 51(41.46) 10.181 0.002 关节置换术 11(28.95) 72(58.54) 手术时间/min 78.58±6.45 71.52±8.41 4.757 < 0.001 Hb/(g/L) 99.77±18.26 126.02±14.15 9.301 < 0.001 WBC/(×109/L) 9.01±1.69 9.52±2.50 1.176 0.241 PLT/(×109/L) 203.36±61.15 222.51±55.59 1.812 0.072 HCT 0.25±0.09 0.32±0.05 6.116 < 0.001 RDW 16.93±2.41 16.84±2.91 0.173 0.863 INR 0.89±0.20 0.88±0.24 0.233 0.816 PT/s 9.71±1.87 9.83±2.01 0.327 0.744 APTT/s 27.34±2.95 26.96±4.74 0.466 0.642 Fib/(g/L) 3.66±1.00 4.03±0.46 3.172 0.002 GG/(mmol/L) 2.29±0.91 0.25±0.10 24.555 < 0.001 表 2 影响老年下肢骨折患者围术期输血的多因素logistic回归分析
因素 β SE Ward χ2 P OR 95%CI 年龄 1.180 0.564 4.379 < 0.001 3.255 1.078~9.832 BMI 0.524 0.289 3.282 0.015 1.688 0.958~2.974 手术时间 0.583 0.363 2.582 0.039 1.792 0.880~3.650 Hb 1.244 0.335 13.787 < 0.001 3.469 1.799~6.689 GG 1.039 0.347 8.969 < 0.001 2.827 1.432~5.581 表 3 GG预测老年下肢骨折患者围术期输血的ROC曲线分析结果
变量 AUC 95%CI P 最佳截断值 灵敏度 特异度 年龄 0.629 1.078~9.832 0.026 68岁 0.688 0.488 BMI 0.677 0.569~0.785 0.003 20.8 kg/m2 0.723 0.595 手术时间 0.637 0.524~0.751 2.582 67.2 min 0.709 0.581 GG 0.774 0.681~0.868 < 0.001 1.07 0.837 0.612 -
[1] Donohoe E, Roberts HJ, Miclau T, et al. Management of lower extremity fractures in the elderly: a focus on post-operative rehabilitation[J]. Injury, 2020, 51(Suppl 2): S118-S122.
[2] Fadhel WB, Taieb L, Villain B, et al. Outcomes after primary ankle arthrodesis in recent fractures of the distal end of the tibia in the elderly: a systematic review[J]. Int Orthop, 2022, 46(6): 1405-1412. doi: 10.1007/s00264-022-05317-0
[3] Kaur G, Selhi HS, Delmotra NJ, et al. Tranexamic acid and reduction of blood transfusion in lower limb trauma surgery: a randomized controlled study[J]. SICOT J, 2021, 7: 53. doi: 10.1051/sicotj/2021053
[4] Xu LL, Shen JJ, Sun JL, et al. The effects of leukocyte filtration on cell salvaged autologous blood transfusion on lung function and lung inflammatory and oxidative stress reactions in elderly patients undergoing lumbar spinal surgery[J]. J Neurosurg Anesthesiol, 2019, 31(1): 36-42. doi: 10.1097/ANA.0000000000000495
[5] Scheen M, Giraud R, Bendjelid K. Stress hyperglycemia, cardiac glucotoxicity, and critically ill patient outcomes current clinical and pathophysiological evidence[J]. Physiol Rep, 2021, 9(2): e14713.
[6] Roberts G, Sires J, Chen A, et al. A comparison of the stress hyperglycemia ratio, glycemic gap, and glucose to assess the impact of stress-induced hyperglycemia on ischemic stroke outcome[J]. J Diabetes, 2021, 13(12): 1034-1042. doi: 10.1111/1753-0407.13223
[7] 董航, 谢秀巧, 黄雪原, 等. 患者血液管理国际专家共识(2018年)的主要推荐及其启示[J]. 中国输血杂志, 2019, 32(12): 1292-1298.
[8] Nathan DM, Kuenen J, Borg R, et al. Translating the A1C assay into estimated average glucose values[J]. Diabetes Care, 2008, 31(8): 1473-1478. doi: 10.2337/dc08-0545
[9] Bennett KJ, Millar SC, Fraysse F, et al. Postoperative lower limb joint kinematics following tibial plateau fracture: a 2-year longitudinal study[J]. Gait Posture, 2021, 83: 20-25. doi: 10.1016/j.gaitpost.2020.10.005
[10] Lancaster P, Kocialkowski C, Pearce O, et al. Open lower limb fractures in the elderly[J]. Injury, 2022, 53(6): 2268-2273. doi: 10.1016/j.injury.2022.03.029
[11] Abdallah R, Rai H, Panch SR. Transfusion reactions and adverse events[J]. Clin Lab Med, 2021, 41(4): 669-696. doi: 10.1016/j.cll.2021.07.009
[12] 刘潺, 陈杰, 闫保娟, 等. 未成年人脊柱侧凸后路矫形术中异体输血的危险因素分析[J]. 临床血液学杂志, 2023, 36(10): 723-727. doi: 10.13201/j.issn.1004-2806.2023.10.007
[13] Mowla SJ, Kracalik IT, Sapiano MRP, et al. A comparison of transfusion-related adverse reactions among apheresis platelets, whole blood-derived platelets, and platelets subjected to pathogen reduction technology as reported to the national healthcare safety network hemovigilance module[J]. Transfus Med Rev, 2021, 35(2): 78-84. doi: 10.1016/j.tmrv.2021.03.003
[14] 阴瑞兰, 魏希建, 王小霞, 等. 术前贫血对急性颅脑损伤手术术中输血患者的影响[J]. 临床血液学杂志, 2023, 36(4): 288-291, 294. doi: 10.13201/j.issn.1004-2806.2023.04.014
[15] Luo XP, He SQ, Li ZA, et al. Quantification and influencing factors of perioperative hidden blood loss during intramedullary fixation for intertrochanteric fractures in the elderly[J]. Arch Orthop Trauma Surg, 2020, 140(10): 1339-1348. doi: 10.1007/s00402-019-03311-7
[16] 郝泽宇, 孙建涛, 刘明辉, 等. 老年股骨近端防旋髓内钉治疗围手术期输血需求的相关因素分析[J]. 滨州医学院学报, 2023, 46(2): 112-116.
[17] Erben HC, Hess F, Welter J, et al. Perioperative blood transfusions in hip and knee arthroplasty: a retrospective assessment of combined risk factors[J]. Arch Orthop Trauma Surg, 2022, 142(8): 1817-1822. doi: 10.1007/s00402-021-03763-w
[18] 王卓, 刘序强, 陈延朕, 等. 老年股骨转子间骨折患者术后输血的相关因素[J]. 中国矫形外科杂志, 2024, 32(2): 104-108.
[19] Ştefan M, Lupu AR, Andrei Ş, et al. Perioperative trajectory of haemoglobin, predictors of blood transfusion and tailoring targets for patient blood management interventions: a single-centre, retrospective study of Non-emergent cardiac surgery patients[J]. Rom J Anaesth Intensive Care, 2021, 28(2): 47-56.
[20] 张忠印, 崔海东, 乔泽星, 等. 老年髋部骨折围术期异体红细胞输血预测的列线图模型构建[J]. 中国老年学杂志, 2022, 42(24): 5986-5990.
[21] Moorthy V, Sim MA, Liu WL, et al. Risk factors and impact of postoperative hyperglycemia in nondiabetic patients after cardiac surgery: a prospective study[J]. Medicine, 2019, 98(23): e15911.
[22] El-Menyar A, Asim M, Mir F, et al. Patterns and effects of admission hyperglycemia and inflammatory response in trauma patients: a prospective clinical study[J]. World J Surg, 2021, 45(9): 2670-2681.
[23] Wang CY, Wang WJ, Li GS, et al. Prognostic value of glycemic gap in patients with spontaneous intracerebral hemorrhage[J]. Eur J Neurol, 2022, 29(9): 2725-2733.
[24] Wu S, Yang YM, Zhu J, et al. Impact of glycemic gap on 30-day adverse outcomes in patients with acute ST-segment elevation myocardial infarction[J]. Atherosclerosis, 2022, 360: 34-41.
[25] Zarean E, Lattanzi S, Looha MA, et al. Glycemic gap predicts in-hospital mortality in diabetic patients with intracerebral hemorrhage[J]. J Stroke Cerebrovasc Dis, 2021, 30(5): 105669.
-




 下载:
下载: