The impact of helper T cell reconstitution on clinical outcomes after HLA-haploidentical allogeneic hematopoietic stem cell transplantation in patients with hematologic malignancy
-
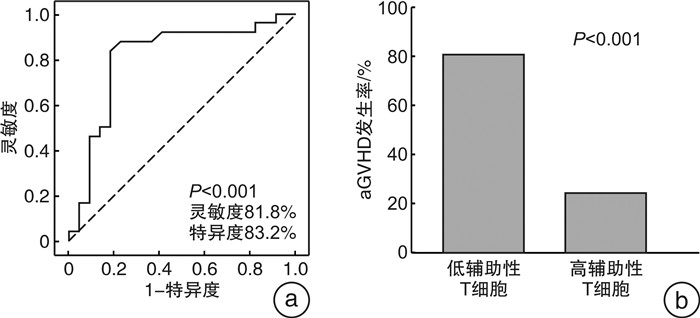
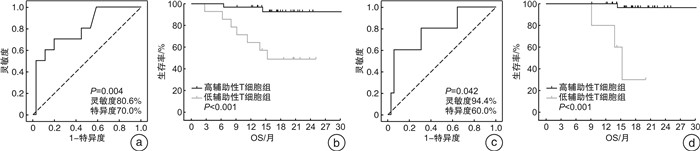
摘要: 目的 探讨恶性血液病患者半相合造血干细胞移植后辅助性T细胞重建对临床预后的影响。方法 纳入2020年7月—2022年12月于西安交通大学第一附属医院血液内科接受半相合造血干细胞移植的恶性血液病患者46例,通过流式细胞术检测移植后外周血T细胞亚群,以供者作为健康对照,分析移植后T细胞重建的规律。通过ROC曲线、Kaplan-Meier生存分析、χ2检验等分析辅助性T细胞重建对移植后患者总生存期(OS) 和急性移植物抗宿主病(aGVHD)的影响。结果 移植后辅助性T细胞恢复较慢,移植后12个月仍显著低于对照组,但呈上升趋势。移植后3个月辅助性T细胞计数 < 70/μL组及移植后9个月辅助性T细胞计数 < 95/μL组OS更差。移植后3个月辅助性T细胞计数 < 90/μL组aGVHD的发生率更高。结论 恶性血液病患者半相合造血干细胞移植后辅助性T细胞恢复较慢,移植后辅助性T细胞重建不良预示更差的OS和更高的aGVHD发生率。可通过动态监测辅助性T细胞重建情况筛选潜在预后不良患者。
-
关键词:
- 辅助性T细胞 /
- 半相合造血干细胞移植 /
- 临床预后 /
- 急性移植物抗宿主病
Abstract: Objective To explore the impact of helper T cell reconstitution on clinical outcomes in patients with hematologic malignancies after HLA-haploidentical allogeneic hematopoietic stem cell transplantation(allo-HSCT).Methods Forty-six patients who received HLA-haploidentical allo-HSCT in the Department of Hematology of the First Affiliated Hospital of Xi'an Jiaotong University from July 2020 to December 2022 were analyzed. T lymphocyte subsets were detected by flow cytometry at different time after transplantation. The clinical data of healthy donors were used as controls to analyze the regularity of T cell reconstitution after transplantation. ROC curves, Kaplan-Meier survival analysis and Chi-square tests were used to analyze the effects of helper T cell reconstitution on overall survival(OS) and acute graft versus host disease(aGVHD).Results Helper T cell recovered slowly after transplantation which were significantly lower than those of healthy controls at 12 months after transplantation, but showed an increasing trend. Helper T cell count < 70/μL after 3 months of transplantation and < 95/μL at 9 months after transplantation predicted poor OS. Helper T cell count < 90/μL at 3 months after transplantation predicted a high incidence of aGVHD.Conclusion The reconstruction of helper T cell after allo-HSCT was slow. Poor reconstruction of helper T cell after transplantation predicted worse OS and a higher incidence of aGVHD. Patients with potentially poor prognosis could be screened by monitoring of helper T cell reconstruction. -

-
表 1 移植患者临床特征
临床特征 数值 移植时年龄/岁 34.5(25.0,48.3) 男性/例(%) 27(58.7) 疾病类型/例(%) AML 26(56.5) ALL 16(34.8) MDS 4(8.7) 供者类型/例(%) 子女供父母 17(37.0) 父母供子女 16(34.8) 兄弟姐妹供 13(28.3) 随访时间/月 17.3(13.7,20.9) MNC输注量/(×108/kg) 8.61(7.31,10.71) CD34+细胞输注量/(×106/kg) 6.11(5.24,7.97) 中性粒细胞植入时间/d 11(10,12) 血小板植入时间/d 12(11,14) 表 2 移植组与对照组T细胞的比较
M(P25,P75) 免疫细胞计数/μL 移植后3个月 移植后6个月 移植后9个月 移植后12个月 对照组 辅助性T细胞 90.62
(53.30,153.66)1)125.74
(86.44,253.86)1)265.43
(148.69,341.91)1)285.64
(175.15,499.95)1)484.92
(334.99,565.49)杀伤性T细胞 368.31
(235.93,645.09)437.69
(308.78,696.73)707.19
(497.77,1 059.15)1)1 000.02
(657.74,1 410.30)1)445.85
(335.99,569.29)与对照组比较,1)P < 0.05。 表 3 辅助性T细胞与移植后OS及aGVHD的相关性
项目 移植3个月 移植后6个月 移植后9个月 移植后12个月 r P r P r P r P 辅助性T细胞与OS -0.429 0.003 - - -0.321 0.041 - - 辅助性T细胞与aGVHD -0.528 < 0.001 - - - - - - -
[1] Gomez-Arteaga A, Gyurkocza B. Recent advances in allogeneic hematopoietic cell transplantation for acute myeloid leukemia[J]. Curr Opin Hematol, 2020, 27(2): 115-121. doi: 10.1097/MOH.0000000000000572
[2] Troullioud Lucas AG, Lindemans CA, Bhoopalan SV, et al. Early immune reconstitution as predictor for outcomes after allogeneic hematopoietic cell transplant; a tri-institutional analysis[J]. Cytotherapy, 2023, 25(9): 977-985. doi: 10.1016/j.jcyt.2023.05.012
[3] Huang JT, Pan ZK, Wang LX, et al. Early T-cell reconstitution predicts risk of EBV reactivation after allogeneic hematopoietic stem cell transplantation[J]. Clin Exp Med, 2024, 24(1): 22. doi: 10.1007/s10238-023-01270-3
[4] Ando T, Tachibana T, Tanaka M, et al. Impact of graft sources on immune reconstitution and survival outcomes following allogeneic stem cell transplantation[J]. Blood Adv, 2020, 4(2): 408-419. doi: 10.1182/bloodadvances.2019001021
[5] Drokov M, Davydova Y, Popova N, et al. High expression of granzyme B in conventional CD4+T cells is associated with increased relapses after allogeneic stem cells transplantation in patients with hematological malignancies[J]. Transpl Immunol, 2021, 65: 101295. doi: 10.1016/j.trim.2020.101295
[6] Yanir A, Schulz A, Lawitschka A, et al. Immune reconstitution after allogeneic haematopoietic cell transplantation: from observational studies to targeted interventions[J]. Front Pediatr, 2021, 9: 786017.
[7] Khoury JD, Solary E, Abla O, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms[J]. Leukemia, 2022, 36(7): 1703-1719. doi: 10.1038/s41375-022-01613-1
[8] Schoemans HM, Lee SJ, Ferrara JL, et al. EBMT-NIH-CIBMTR Task Force position statement on standardized terminology & guidance for graft-versus-host disease assessment[J]. Bone Marrow Transplant, 2018, 53(11): 1401-1415. doi: 10.1038/s41409-018-0204-7
[9] Elmariah H, Brunstein CG, Bejanyan N. Immune reconstitution after haploidentical donor and umbilical cord blood allogeneic hematopoietic cell transplantation[J]. Life, 2021, 11(2): 102. doi: 10.3390/life11020102
[10] 郑晓燕, 刘哲, 王晓宁, 等. 异基因造血干细胞移植后巨细胞病毒再激活的危险因素分析[J]. 临床血液学杂志, 2024, 37(5): 339-342, 348. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2024.05.010
[11] Justus JLP, Beltrame MP, de Azambuja AP, et al. Immune recovery and the role of recent thymic emigrated T lymphocytes after pediatric hematopoietic stem cell transplantation[J]. Cytotherapy, 2024, 26(9): 980-987. doi: 10.1016/j.jcyt.2024.04.073
[12] Mazzolari E, Forino C, Guerci S, et al. Long-term immune reconstitution and clinical outcome after stem cell transplantation for severe T-cell immunodeficiency[J]. J Allergy Clin Immunol, 2007, 120(4): 892-899. doi: 10.1016/j.jaci.2007.08.007
[13] Velardi E, Tsai JJ, van den Brink MRM. T cell regeneration after immunological injury[J]. Nat Rev Immunol, 2021, 21: 277-291. doi: 10.1038/s41577-020-00457-z
[14] 上官思雨, 惠卉, 余浩源, 等. 异基因造血干细胞移植后巨细胞病毒感染的危险因素分析[J]. 临床血液学杂志, 2023, 36(5): 349-353. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2023.05.010
[15] 王雯娟, 龚莎, 马乐, 等. 供者干细胞淋巴细胞亚群检测对异基因造血干细胞移植后免疫排斥反应及免疫重建的临床意义[J]. 临床血液学杂志, 2023, 36(3): 170-174. https://lcxy.whuhzzs.com/article/doi/10.13201/j.issn.1004-2806.2023.03.006
[16] Fedele R, Martino M, Garreffa C, et al. The impact of early CD4+lymphocyte recovery on the outcome of patients who undergo allogeneic bone marrow or peripheral blood stem cell transplantation[J]. Trasfusione Del Sangue, 2012, 10(2): 174-180.
[17] Kim DH, Sohn SK, Won DI, et al. Rapid helper T-cell recovery above 200×106/L at 3 months correlates to successful transplant outcomes after allogeneic stem cell transplantation[J]. Bone Marrow Transplant, 2006, 37(12): 1119-1128. doi: 10.1038/sj.bmt.1705381
[18] Bejanyan N, Brunstein CG, Cao Q, et al. Delayed immune reconstitution after allogeneic transplantation increases the risks of mortality and chronic GVHD[J]. Blood Adv, 2018, 2(8): 909-922. doi: 10.1182/bloodadvances.2017014464
[19] Massei MS, Capolsini I, Mastrodicasa E, et al. HLA-haploidentical hematopoietic stem cells transplantation with regulatory and conventional T-cell adoptive immunotherapy in pediatric patients with very high-risk acute leukemia[J]. Bone Marrow Transplant, 2023, 58: 526-533. doi: 10.1038/s41409-023-01911-x
[20] Li LL, Shang LM, Gao J, et al. Janus kinase inhibitor ruxolitinib blocks thymic regeneration after acute Thymus injury[J]. Biochem Pharmacol, 2020, 171: 113712. doi: 10.1016/j.bcp.2019.113712
[21] Dower WJ, Park AI, Bakker AV, et al. A mechanistically novel peptide agonist of the IL-7 receptor that addresses limitations of IL-7 cytokine therapy[J]. PLoS One, 2023, 18(10): e0286834. doi: 10.1371/journal.pone.0286834
[22] Gao D, Yi XM, Feng L, et al. MARCH8 mediates K27-linked polyubiquitination of IL-7 receptor α to negatively regulate IL-7-triggered T cell homeostasis[J]. J Immunol, 2024: ji2400253.
[23] Pagliuca S, Schmid C, Santoro N, et al. Donor lymphocyte infusion after allogeneic haematopoietic cell transplantation for haematological malignancies: basic considerations and best practice recommendations from the EBMT[J]. Lancet Haematol, 2024, 11(6): e448-e458. doi: 10.1016/S2352-3026(24)00098-X
[24] Harada K, Mizuno S, Yano S, et al. Donor lymphocyte infusion after haploidentical hematopoietic stem cell transplantation for acute myeloid leukemia[J]. Ann Hematol, 2022, 101(3): 643-653. doi: 10.1007/s00277-021-04731-5
[25] Mallhi KK, Srikanthan MA, Baker KK, et al. HLA-haploidentical hematopoietic cell transplantation for treatment of nonmalignant diseases using nonmyeloablative conditioning and post-transplant cyclophosphamide[J]. Biol Blood Marrow Transplant, 2020, 26(7): 1332-1341. doi: 10.1016/j.bbmt.2020.03.018
-

计量
- 文章访问数: 185
- 施引文献: 0



 下载:
下载: