Diagnosis and treatment of newly diagnosed hematological malignancies with critical COVID-19 and literature review
-
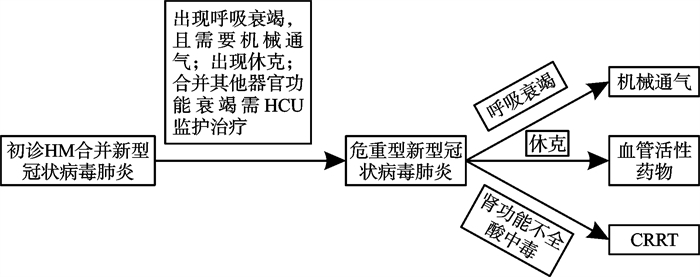
摘要: 目的 分析在2022年12月我国疫情防控政策调整后,奥密克戎传播高峰时期初诊恶性血液病(HM)合并危重新型冠状病毒肺炎患者的诊治。方法 回顾性分析苏州大学附属第一医院血液重症监护病房(HCU)收治的8例初诊HM合并危重新型冠状病毒肺炎的临床表现、治疗及预后,结合既往文献总结此类患者的救治经验。结果 8例患者均因呼吸衰竭接受了机械通气,其中4例为有创通气,3例患者接受升压药治疗,3例接受连续性肾脏替代治疗,7例接受诱导化疗,经血液专科治疗结合ICU生命支持后院内生存率为62.5%。结论 初诊HM患者免疫功能低下,在大流行的背景下感染后易进展为重型/危重型新型冠状病毒肺炎,血液专科ICU能充分结合血液专科治疗和高级生命支持提高患者救治成功率。Abstract: Objective To analyze the diagnosis and treatment of newly diagnosed patients with hematological malignancies (HMs) and critical COVID-19 during the peak of Omicron transmission after the adjustment of China's epidemic prevention and control policy in December 2022.Methods A retrospective analysis was conducted on the clinical manifestations, treatment, and prognosis of 8 patients with newly diagnosed HM suffering from critical COVID-19 admitted to the Hematology ICU of the First Affiliated Hospital of Soochow University. The rescue experience for such patients was summarized in combination with previous literature.Results All 8 patients underwent mechanical ventilation due to respiratory failure, including 4 cases of invasive mechanical ventilation. Three patients received vasopressors, 3 underwent continuous renal replacement therapy(CRRT), and 7 received induction chemotherapy. The in-hospital survival rate after treatment of HMs combined with ICU life support was 62.5%.Conclusion Patients with newly diagnosed HM have decreased immune function and are prone to progressing to severe/critical COVID-19 upon infection against the backdrop of the pandemic. The Hematology ICU can effectively improve the survival of this population by fully integrating hematological treatment and advanced life support.
-
Key words:
- hematological malignancy /
- COVID-19 /
- Omicron /
- intensive care unit
-

-
表 1 8例初诊HM合并危重新型冠状病毒肺炎患者的基本临床特征
序号 性别 年龄/岁 HM类型 白细胞计数/(×109/L) 血红蛋白水平/(g/L) 血小板计数/(×109/L) CRP /(mg/L) 分期/基因突变 ECOG /分 1 男 32 T-ALL 209.39 125 16 58.90 NOTCH1 4 2 女 20 APL 93.29 88 47 220.77 阴性 4 3 男 54 AML 86.34 90 110 181.00 DNMT3A、FLT3-ITD、NPM1 4 4 男 69 APL 47.75 137 33 70.96 阴性 3 5 女 64 PCL 1.72 57 22 4.89 DSⅢ期B组 3 6 男 79 DLBCL 13.43 76 105 3.82 Ⅳ期A组 4 7 女 44 T-ALL/LBL 47.40 61 14 192.59 未知 4 8 女 80 MM 3.39 58 82 73.76 DSⅢ期B组 4 注:T-ALL:急性T淋巴细胞白血病;APL:急性早幼粒细胞白血病;DLBCL:弥漫大B细胞淋巴瘤;T-ALL/LBL:T淋巴母细胞白血病/淋巴瘤;MM:多发性骨髓瘤。 表 2 8例初诊HM合并危重新型冠状病毒肺炎患者的合并症和干预措施
序号 CPIS/分 SOFA/分 APACHEⅡ/分 机械通气 CRRT 血管活性药物 HCU住院天数/d 1 8 10 17 是 是 是 17 2 8 8 22 是 是 是 16 3 8 5 21 是 否 否 40 4 4 5 13 是 否 否 33 5 5 5 14 是 否 否 8 6 5 4 16 是 否 否 7 7 4 8 22 是 是 是 8 8 5 6 27 是 否 否 9 注:CPIS:临床肺部感染评分;SOFA:序贯器官衰竭评分;APACHEⅡ:急性生理与慢性健康评分。 表 3 8例初诊HM合并危重新型冠状病毒肺炎患者的原发病治疗和转归
序号 原发病 治疗方案 骨髓评估 后续治疗 转归(死亡时间) 1 T-ALL 长春地辛+地塞米松 CR / 死亡(d17) 2 APL 维甲酸+复方黄黛片/亚砷酸+米托蒽醌 未评估 / 死亡(d16) 3 AML 维奈克拉+阿扎胞苷 CR 维奈克拉+阿扎胞苷,HSCT 存活 4 APL 维甲酸+亚砷酸/复方黄黛片 CR 维甲酸+复方黄黛片 存活 5 PCL BiRd+维奈克拉 PR 支持治疗 存活 6 DLBCL CD20单抗+来那度胺+泽布替尼 未评估 来那度胺+泽布替尼 存活 7 T-ALL/LBL 地塞米松 未评估 化疗 存活 8 MM VRD-lite 未评估 / 死亡(d9) 注:死亡时间:HCU的住院时间。 -
[1] Wang J, Shao L, Liang J, et al. Chinese expert consensus on the management of patients with hematologic malignancies infected with SARS-CoV-2[J]. J Cancer Res Ther, 2023, 19(6): 1495-1500. doi: 10.4103/jcrt.JCRT_782_23
[2] 何文娟, 陈智超, 胡豫. 高白细胞急性白血病常见近期并发症[J]. 临床血液学杂志, 2024, 37(3): 205-209.
[3] 季浩, 凌小穗, 李增政, 等. 急性白血病并发肺部感染诊疗的研究进展[J]. 中国实验血液学杂志, 2024, 32(4): 1284-1289.
[4] Aries JA, Davies JK, Auer RL, et al. Clinical outcome of coronavirus disease 2019 in haemato-oncology patients[J]. Br J Haematol, 2020, 190(2): e64-e67.
[5] Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia[J]. Blood, 2016, 127(20): 2391-2405. doi: 10.1182/blood-2016-03-643544
[6] 中华人民共和国国家卫生健康委员会. 新型冠状病毒肺炎诊疗方案(试行第九版)[J]. 中华临床感染病杂志, 2022, 15(2): 81-89. doi: 10.3760/cma.j.issn.1674-2397.2022.02.001
[7] Zhu X, Jiang Q, Lu J, et al. COVID-19 infection in patients with haematological malignancies: a single-centre survey in the latest Omicron wave in China[J]. Br J Haematol, 2023, 202(1): 31-39. doi: 10.1111/bjh.18823
[8] Zhao H, He Y, Li Z, et al. Impact of SARS-CoV-2 infection on patients with hematological malignancies: a retrospective study[J]. Hematology, 2023, 28(1): 2288480. doi: 10.1080/16078454.2023.2288480
[9] Fu J, Kong J, Wang W, et al. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: A retrospective study in Suzhou China[J]. Thromb Res, 2020, 192: 3-8. doi: 10.1016/j.thromres.2020.05.006
[10] Nadkarni AR, Vijayakumaran SC, Gupta S, et al. Mortality in Cancer Patients With COVID-19 Who Are Admitted to an ICU or Who Have Severe COVID-19: A Systematic Review and Meta-Analysis[J]. JCO Glob Oncol, 2021, 7: 1286-1305.
[11] Lahmer T, Salmanton-García J, Marchesi F, et al. Need for ICU and outcome of critically ill patients with COVID-19 and haematological malignancies: results from the EPICOVIDEHA survey[J]. Infection, 2024, 52(3): 1125-1141. doi: 10.1007/s15010-023-02169-7
[12] Pagano L, Salmanton-García J, Marchesi F, et al. COVID-19 infection in adult patients with hematological malignancies: a European Hematology Association Survey(EPICOVIDEHA)[J]. J Hematol Oncol, 2021, 14(1): 168. doi: 10.1186/s13045-021-01177-0
[13] Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study[J]. Lancet, 2020, 395(10229): 1054-1062. doi: 10.1016/S0140-6736(20)30566-3
[14] Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis[J]. Eur Respir J, 2020, 55(5): 2000547. doi: 10.1183/13993003.00547-2020
[15] Li X, Zhao A, Jiang H, et al. Clinical characteristics and outcomes of COVID-19 infection in Chinese patients with hematologic malignancies in the Omicron era[J]. Hematology, 2023, 28(1): 2288477. doi: 10.1080/16078454.2023.2288477
[16] Guo W, Zheng Y, Feng S. Omicron related COVID-19 prevention and treatment measures for patients with hematological malignancy and strategies for modifying hematologic treatment regimes[J]. Front Cell Infect Microbiol, 2023, 13: 1207225. doi: 10.3389/fcimb.2023.1207225
[17] Liang P, Xie Y, Liu Z, et al. Venetoclax and hypomethylating agents in critically ill patients with newly diagnosed acute myeloid leukaemia[J]. Br J Haematol, 2024, 204(4): 1219-1226. doi: 10.1111/bjh.19291
[18] Civriz Bozdağ S, Cengiz Seval G, Yönal Hindilerden ł, et al. Clinical Characteristics and Outcomes of COVID-19 in Turkish Patients with Hematological Malignancies[J]. Turk J Haematol, 2022, 39(1): 43-54. doi: 10.4274/tjh.galenos.2021.2021.0287
-




 下载:
下载: